Abstract
Background
Prospective studies have established the mycophenolate mofetil (MMF) efficiency in childhood idiopathic nephrotic syndrome (INS) but reports on the long-term outcome are lacking. Moreover, the search for factors influencing its efficiency would be useful to define its place among the other treatments.
Methods
We performed a monocentric retrospective study including 96 children with steroid-dependent INS followed for 4.7 years (median) (IQ 3–6) after the onset of MMF treatment. The characteristics of responder patients (n = 74), as defined by a 50 % decrease of relapse rate and/or a 60 % decrease of steroid dose, and of non-responder patients (n = 22) were compared by univariate analysis and multivariate logistic regression.
Results
Withdrawal of prednisone was achieved in 48/96 patients after a median duration of 18.1 months (IQ 7.8–30.0) of MMF. Only 26/48 patients did not relapse under MMF alone. After MMF was stopped in these patients, only six remained in remission without any treatment at last follow-up. Responders had a shorter time to remission at the first flare (9.5 vs. 15 days, p = 0.02), a shorter disease duration prior to the onset of MMF (22.2 vs. 94.5 months, p = 0.001), and were younger at the MMF initiation (6.7 vs. 10.1 years, p = 0.02) than non-responder patients. The age of MMF initiation was an independent factor associated with efficiency (OR = 0.80, 95 % CI [0.69, 0.93], p < 0.01).
Conclusions
MMF is more efficient in young patients treated early in the disease course. Nevertheless, MMF has no remnant effect while nearly all patients relapsed after withdrawal of the drug.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic nephrotic syndrome is the most frequent glomerulopathy in children between 1.5 and 10 years of age [1]. After an acute onset occurring in children without any significant medical history, the disease relapses in about 80 % of the patients and can last for many years, especially in patients that are dependent on steroids [2]. Treatments to control and prevent relapses are similar to those used in autoimmune disorders, including steroids, cyclophosphamide, rituximab, calcineurin inhibitors, and mycophenolate [3, 4]. At least six prospective studies demonstrated the efficiency of mycophenolate to prevent relapses of idiopathic nephrotic syndrome with a high level of evidence [5–10]. Nevertheless, the long-term outcome of patients treated by mycophenolate is lacking. Herein, we report the long-term follow-up of a large cohort of patients treated with mycophenolate for steroid-dependent nephrotic syndrome (SDNS).
Patients and methods
Study population
This retrospective, single-center observational study included patients with SDNS treated with mycophenolate between January 1995 and June 2012 at the Department of Pediatric Nephrology of Robert-Debré Hospital-APHP, Paris, France. Patients with SDNS were included in this study if they were 1–18 years of age at the start of mycophenolate treatment and if they had a minimum follow-up of 12 months after the start of mycophenolate. Patients were excluded from the study if (1) they were treated with a combination of mycophenolate with other immunosuppressive drugs, (2) they had a history of treatment with anti-CD20 antibody, (3) or a history of either early or late steroid resistance during the course of the disease.
For each patient, data were collected from medical records. The protocol (no. 1614078v0) was submitted and accepted by the CNIL, the French data protection authority. This work was approved by the local ethics committee.
Definitions and treatment protocol
The definitions and criteria for NS, remission, relapse, frequent relapse, and steroid resistance were those of the French Society of Pediatric Nephrology [11]. The initial treatment followed the guidelines of the French Society of Pediatric Nephrology [11]. Patients were considered to have a steroid-sensitive NS (SSNS) if remission (ratio proteinuria/urine creatinine < 0.02 g/mmol and albumin > 30 g/l) occurred within 4 weeks of oral prednisone treatment at the dose of 60 mg/m2/day as well as those who responded within 8 days following three methylprednisolone (MP) infusions of 1 g/1.73 m2 in case of resistance to 4 weeks of oral prednisone. Then after, prednisone was decreased as described: 60 mg/m2/eod for 8 weeks then 45 mg/m2/eod for 2 weeks, 30 mg/m2/eod, and 15 mg/m2/eod for 2 weeks. The total cumulative dose of prednisone given for the first flare was 3990 mg/m2 in 18 weeks. Steroid dependency (SDNS) was defined if a relapse occurred during the decrease of steroid or within 14 days after stopping this treatment [2, 12].
Relapse was defined as a proteinuria/creatininuria ratio higher than 0.25 g/mmol of urine creatinine associated along with a serum albuminemia below 30 g/l. Relapses were treated with oral prednisone at a daily dose of 60 mg/m2/ day until remission. After remission, steroid therapy was continued at the same dose for 6 days, then gradually reduced to a threshold dose of prednisone (5 mg eod or a dose 10 to 25 % higher than the dose for which the relapse occurred).
Mycophenolate mofetil (Cellcept®; Roche, Basel, Switzerland) was given in two divided doses at 600 mg/m2/day during the first 7 days, and then increased to 1200 mg/m2/day. Previous treatment with levamisole or cyclosporine was stopped when starting mycophenolate.
The mycophenolate effectiveness was defined as a reduction of at least 50 % of relapses frequency and/or a reduction of at least 60 % of the steroid cumulative dose during the first year after initiation of mycophenolate. These two criteria allowed identifying two groups of patients: non-responders who did not fulfill the above criteria and responders who fulfilled the above criteria of mycophenolate efficiency.
Follow-up
Patients were systematically followed at the outpatient clinics every 3 months. At each appointment, weight, height, blood pressure, proteinuria monitoring (dipstick Albustix® or proteinuria dosage), side effects assessment (i.e., digestive disorders) and laboratory tests (CBC, liver function tests) were collected. Moreover, we require proteinuria screening by urine dipstick Albustix® twice a week at home. If the dipsticks were positive with 2 + for more than 3 days, a dosage of proteinuria and serum albumin were performed to confirm NS relapse. A renal biopsy was only available in patients who had a previous treatment with cyclosporin A during more than 2 years.
Statistical analyses
Qualitative data were described as numbers and percentages and quantitative data as median and inter quartiles. Data of both groups were first compared by univariate analysis to select factors that may be related to the effectiveness of mycophenolate. When applicable, Chi-square test was used to compare qualitative variables. If the variables did not satisfy the conditions of validity of a Chi-square then, Fisher’s exact test was used. Comparison of quantitative variables was performed by Student’s t test, after prior verification of equality of variances and normality of variables. If the variables were not normally distributed, we used non-parametric tests (Wilcoxon test or Mann–Whitney). Variables with a p value less than 0.05 in the univariate analysis were then included in a multivariate logistic regression. Kaplan–Meier method was used to study the time without relapse and to draw survival curves. The significance level was set at 0.05. Statistical analysis was performed using Prism 5 for Windows, version 5.01 1992–2007, GraphPad Software, Inc.
Results
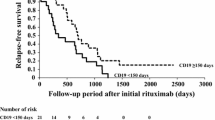
Among the 121 patients who received mycophenolate for SDNS during the study period, only 96 fulfilled inclusion criteria and were included in this study (Fig. 1). The main characteristics of the 96 patients are presented in Table 1. The median follow-up time was 4.7 years (IQ 3.0–6.0). The median doses of mycophenolate were 1117 mg/m2/day (IQ 991–1190; n = 88), 1098.4 mg/m2/day (IQ 1024–1168; n = 80) and 1063 mg/m2/day (IQ 967–1158; n = 63) at 6, 12, and 24 months, respectively. The median duration of mycophenolate therapy was 32 months (IQ 22–46). All patients received prednisone at the onset of mycophenolate therapy. Figure 2 presents relapse-free survival from the first day of treatment with mycophenolate. The median relapse-free survival was 15 months (IQ 5.6–37.1). Compared to the last year, prior to the start of mycophenolate, there was a 67 % reduction in the rate of relapse, a 75 % reduction of the threshold dose of prednisone needed to maintain remission, and a 40 % reduction of the cumulative annual dose of prednisone after 12 months of mycophenolate (Table 2). Withdrawal of prednisone was achieved in 48/96 patients after a median duration of 18.1 months (IQ 7.8–30.0) of mycophenolate treatment. Those 48 patients had no relapse since the onset of the mycophenolate. Only 26 of 48 patients did not relapse under mycophenolate alone after the withdrawal of prednisone. In those 26 patients successfully treated with mycophenolate and without prednisone, mycophenolate was stopped after a median delay of 13.7 months (IQ 5.8–18.8) from the withdrawal of prednisone. Six patients remained in remission at last follow-up (3.9–19.6 months) while 20 of 26 patients relapsed within a median time of 11.8 months (IQ 6.0–18.1).
At 12 months of follow-up, 22 patients were classified as non-responders and 74 as responders to mycophenolate therapy according to the definitions shown in the “Definitions and treatment protocol” section. Patients’ characteristics of non-responders and responders are showed in Table 3. Among the 22 non-responders, 14 had no significant changes in the severity of the disease and eight had a worsened outcome with an increased rate of relapse despite the addition of mycophenolate. No significant difference was observed between responders and non-responders for ethnicity, gender, renal histology, or MP infusion at the first flare. As expected, non-responders displayed a more severe disease with a longer time of remission at 1st flare, a longer duration of the disease with more relapses and received more cyclosporine prior to mycophenolate. Paradoxically, responders had a more active disease with a significantly higher rate of relapse (median 3.0/year; IQ 2.0–4.1) compared to non-responders (median 1.5/year; IQ 1.0–3.0; p < 0.001) and a heavier cumulative dose of prednisone (median 590.3 mg/m2/month; IQ 370–1052) compared to non-responders (median 332 mg/m2/month; IQ 278–527; p < 0.005) in the year preceding the onset of mycophenolate. Of note, univariate analysis showed that responders were treated earlier in age and after a shorter duration of disease compared to non-responders (Table 3). The multivariate analysis showed that only the age at the onset of the treatment was an independent factor in its efficacy (odds ratio 0.8, CI 95 % [0.69–0.93], p < 0.01). By performing an ROC curve, the age threshold below which the chances of increased mycophenolate efficacy was 5.8 years with an AUC of 0.67 (CI 95 % [0.5314; 0.8003]; p < 0.02). The median time without relapse in the responders was 27.8 months when it was only 3.9 months in the non-responders (p < 0.0001). Nevertheless, at 60 months of follow-up, after the withdrawal of treatment, the same proportion of responders and non-responders had relapsed.
At last follow-up 58/96 patients were in remission without treatment. The disruption of the disease was obtained after the addition of levamisole in 4/58 patients, rituximab in 38/58 patients, and prednisone in 11/58. Only five patients were driven to a stable remission without any additional treatment. Thirty-eight patients out of 96 were still under treatment including one or several of the following drugs: prednisone (n = 22), mycophenolate (n = 16), tacrolimus (n = 10), cyclosporine A (n = 5), and levamisole (n = 4).
Rare side effects were observed. Six patients (6 %) had mild gastrointestinal symptoms (mild abdominal pain, dyspepsia) at the start of mycophenolate, which disappeared after a few weeks without specific treatment. More severe gastrointestinal symptoms were found in five patients (5.2 %) (diarrhea, severe abdominal pain, weight loss, and poor appetite): treatment had to be stopped in only one patient, symptomatic treatment was prescribed for two patients, and no treatment in the last two patients. Two patients had leukopenia and one patient had major depressive disorder leading to mycophenolate discontinuation.
Discussion
Although several prospective trials brought strong evidence of the efficiency of mycophenolate mofetil in treating steroid-dependent nephrotic syndrome, data on long-term treatment and follow-up after treatment withdrawal were lacking. Such data were needed to refine the use of mycophenolate in clinical practice. The main results of this study are that although mycophenolate was useful in preventing relapses and spare steroids, it has no disruptive effect on the disease. In addition, the analysis at 1 year showed that mycophenolate was more effective in young patients treated early in the course of the disease.
Steroid-dependent nephrotic syndrome is a clinical condition with a high morbidity due to the toxicity of long-lasting steroid therapy with high doses of prednisone and to the length of the disease. Cyclophosphamide, as well as chlorambucil in some teams, was used to control steroid toxicity until from the 60′ to the 90′ [13]. Although these drugs allowed improvement in a significant fraction of patients [14–16], the course of the disease was not changed in the majority of them. In addition, their use was limited by the gonadotoxicity [17] and by the risk of severe infections. Then after, in the 90′, levamisole and cyclosporine A were somehow preferred as the first-line treatment of steroid dependency but with a limited availability and efficiency for the levamisole and a risk of renal fibrosis for the cyclosporine A.
Mycophenolate mofetil is an inhibitor of the de novo purine pathway with preferential inhibitory effects on T and B lymphocyte proliferation [18] as well as on immunoglobulin production [19]. The success of mycophenolate to treat steroid-dependent patients certainly relies on the efficiency to limit the exposure to prednisone as well as to the lack of irreversible side effects. Six prospective studies provided strong evidence of mycophenolate efficiency in patients with steroid-dependent nephrotic syndrome [5–10]. In all studies, mycophenolate showed the ability to decrease the relapse rate and the cumulative prednisone dose. In addition, mycophenolate has a similar efficacy as cyclosporine, but with less side effects, and especially no risk of nephrotoxicity and no cosmetic adverse events [20]. Digestive troubles, infectious events, as well as anemia, lymphopenia, or thrombocytopenia, have been reported in several series, but were always mild and transient [3, 5]. As expected, the efficacy of mycophenolate is proportional to the drug exposure while an AUC over 50 μg h/ml showed a better effect compared to AUC below 50 μg h/ml [10, 21]. Consistently, our study showed similar effects on steroid sparing. Prednisone could have been stopped in only half of the patients. This result is consistent with other series that show that 40 % of patients relapse in the first year of treatment [21, 22].
The main strength of our study is the long duration of treatment as well as the long-term follow-up, while most studies are limited to a 1-year follow-up [5–9, 23]. A major finding is that only 5 % of the patients had a complete and apparently definite recovery of the disease after withdrawal of all oral treatments. Kim et al. report a better result of 34 % of sustained remission but the duration of the follow-up is not mentioned in this paper [24], whereas other studies also found a relapse within 1 year after stopping mycophenolate in the majority of patients [5, 7, 25]. Moreover, the withdrawal of prednisone in half of the patients was unsuccessful, leading to a relapse in another half of the patients treated with mycophenolate alone. Consequently, we suggest that mycophenolate is a useful treatment either to wait for the spontaneous definitive recovery of the disease or to wait for the appropriate time to use drugs with a remnant effect as cyclophosphamide or rituximab. Considering the physiopathological aspect, mycophenolate is limiting the proliferation of immune cells without any known effects on immune cell apoptosis. The lack of apoptotic effect of mycophenolate might explain the absence of remnant effect found in some studies including our study. By contrast, cyclophosphamide and rituximab, which are specifically cytotoxic for B cells and plasma cells, lead a fraction of patients to long-lasting remission or definite recovery [26, 27]. Indeed, cyclophosphamide is more efficient after the age of 7 years [14, 16] and rituximab is widely considered to be quite dangerous before the age of 5 years due to the random possibility of hazardous primary viral infection especially with the polyoma viruses [28].
Another strength of our study is the use of a primary outcome, namely the decrease of relapse rate and/or the decrease of cumulative dose of steroids, designed to be clinically relevant and closer to the expectations of the clinicians. By contrast, those criteria of efficiency were highly variable (number of relapses in 6 months, or minimum dose of steroid without relapse for example) in other studies [5, 10, 22]. The comparison of the disease evolution during the first year of mycophenolate treatment between groups shows that our criteria seem useful for separating responders from non-responders.
Some deleterious APO-L1 variants have been associated with a lesser response to prednisone and calcineurin antagonists in patients with idiopathic nephrotic syndrome and are more frequent in African Americans. In our series, responders and non-responders to mycophenolate were not different in the distribution of ethnicity and the APO-L1 were not systematically investigated in this retrospective study [29].
Noteworthy, our analysis at the first year of treatment confirmed that mycophenolate is more efficient in patients under 6 years old, even if they presented a more severe disease in the year preceding the treatment, than in patients treated later in life and during the course of the disease. Consistently, a prospective randomized study is underway in France to compare the respective efficacy of mycophenolate and cyclophosphamide according to age.
In conclusion, this study confirms the efficacy of prolonged treatment with mycophenolate in patients with steroid-dependent nephrotic syndrome and found that mycophenolate is more efficient when patients are treated at a younger age and early in the course of the disease. However, mycophenolate showed no remnant effect, since nearly all patients relapsed after the withdrawal of the drug. This finding calls for the development of other treatment strategies not only containing the disease but aiming to stop it.
References
Deschênes G, Leclerc A (2010) Epidemiology of the idiopathic nephrotic syndrome. Arch Pédiatrie Organe Off Sociéte Fr Pédiatrie 17:622–623. 693X(10)70028-2
Gipson DS, Massengill SF, Yao L, Nagaraj S, Smoyer WE, Mahan JD, Wigfall D, Miles P, Powell L, Lin JJ, Trachtman H, Greenbaum LA (2009) Management of childhood onset nephrotic syndrome. Pediatrics 124:747–757. doi:10.1542/peds.2008-1559
van Husen M, Kemper MJ (2011) New therapies in steroid-sensitive and steroid-resistant idiopathic nephrotic syndrome. Pediatr Nephrol 26:881–892
Büscher AK, Kranz B, Büscher R, Hildebrandt F, Dworniczak B, Pennekamp P, Kuwertz-Bröking E, Wingen AM, John U, Kemper M, Monnens L, Hoyer PF, Weber S, Konrad M (2010) Immunosuppression and renal outcome in congenital and pediatric steroid-resistant nephrotic syndrome. Clin J Am Soc Nephrol CJASN 5:2075–2084
Bagga A, Hari P, Moudgil A, Jordan SC (2003) Mycophenolate mofetil and prednisolone therapy in children with steroid-dependent nephrotic syndrome. Am J Kidney Dis 42:1114–1120
Mendizábal S, Zamora I, Berbel O, Sanahuja MJ, Fuentes J, Simon J (2005) Mycophenolate mofetil in steroid/cyclosporine-dependent/resistant nephrotic syndrome. Pediatr Nephrol 20:914–919
Hogg RJ, Fitzgibbons L, Bruick J, Ault B, Baqi N, Trachtman H, Swinford R (2006) Mycophenolate mofetil in children with frequently relapsing nephrotic syndrome: a report from the Southwest Pediatric Nephrology Study Group. Clin J Am Soc Nephrol 1:1173–1178
Fujinaga S, Ohtomo Y, Umino D, Takemoto M, Shimizu T, Yamashiro Y, Kaneko K (2007) A prospective study on the use of mycophenolate mofetil in children with cyclosporine-dependent nephrotic syndrome. Pediatr Nephrol 22:71–76
Dorresteijn EM, Kist-van Holthe JE, Levtchenko EN, Nauta J, Hop WC, van der Heijden AJ (2008) Mycophenolate mofetil versus cyclosporine for remission maintenance in nephrotic syndrome. Pediatr Nephrol 23:2013–2020
Baudouin V, Alberti C, Lapeyraque A-L, Bensman A, André JL, Broux F, Cailliez M, Decramer S, Niaudet P, Deschênes G, Jacqz-Aigrain E, Loirat C (2012) Mycophenolate mofetil for steroid-dependent nephrotic syndrome: a phase II Bayesian trial. Pediatr Nephrol 27:389–396
Bérard E, Broyer M, Dehennault M, Dumas R, Eckart P, Fischbach M, Loirat C, Martinat L, Pediatric Society of Nephrology (2005) Corticosensitive nephrotic syndrome (or nephrosis) in children. Therapeutic guideline proposed by the Pediatric Society of Nephrology. Néphrol Thér 1:150–156
(1984) Minimal change nephrotic syndrome in children: deaths during the first 5 to 15 years’ observation. Report of the International Study of Kidney Disease in Children. Pediatrics 73:497–501
Abeyagunawardena AS, Dillon MJ, Rees L, van’t Hoff W, Trompeter RS (2003) The use of steroid-sparing agents in steroid-sensitive nephrotic syndrome. Pediatr Nephrol 18:919–924
Azib S, Macher MA, Kwon T, Dechartres A, Alberti C, Loirat C, Deschênes G, Baudouin V (2011) Cyclophosphamide in steroid-dependent nephrotic syndrome. Pediatr Nephrol 26:927–932
Cammas B, Harambat J, Bertholet-Thomas A, Bouissou F, Morin D, Guigonis V, Bendeddouche S, Afroukh-Hacini N, Cochat P, Llanas B, Decramer S, Ranchin B (2011) Long-term effects of cyclophosphamide therapy in steroid-dependent or frequently relapsing idiopathic nephrotic syndrome. Nephrol Dial Transplant 26:178–184
Zagury A, de Oliveira AL, de Moraes CAP, de Araujo Montalvão JA, Novaes RH, de Sá VM, Monteiro de Carvalho Dde B, Matuck T (2011) Long-term follow-up after cyclophosphamide therapy in steroid-dependent nephrotic syndrome. Pediatr Nephrol 26:915–920
Latta K, von Schnakenburg C, Ehrich JH (2001) A meta-analysis of cytotoxic treatment for frequently relapsing nephrotic syndrome in children. Pediatr Nephrol 16:271–282
Allison AC, Eugui EM (2000) Mycophenolate mofetil and its mechanisms of action. Immunopharmacology 47:85–118
Heidt S, Roelen DL, Eijsink C, van Kooten C, Claas FH, Mulder A (2008) Effects of immunosuppressive drugs on purified human B cells: evidence supporting the use of MMF and rapamycin. Transplantation 86:1292–1300
Gellermann J, Querfeld U (2004) Frequently relapsing nephrotic syndrome: treatment with mycophenolate mofetil. Pediatr Nephrol 19:101–104
Gellermann J, Weber L, Pape L, Tönshoff B, Hoyer P, Querfeld U (2013) Mycophenolate mofetil versus cyclosporin A in children with frequently relapsing nephrotic syndrome. J Am Soc Nephrol 24:1689–1697
Banerjee S, Pahari A, Sengupta J, Patnaik SK (2013) Outcome of severe steroid-dependent nephrotic syndrome treated with mycophenolate mofetil. Pediatr Nephrol 28:93–97
Novak I, Frank R, Vento S, Vergara M, Gauthier B, Trachtman H (2005) Efficacy of mycophenolate mofetil in pediatric patients with steroid-dependent nephrotic syndrome. Pediatr Nephrol B 20:1265–1268
Kim J, Patnaik N, Chorny N, Frank R, Infante L, Sethna C (2014) Second-line immunosuppressive treatment of childhood nephrotic syndrome: a single-center experience. Nephron Extra 4:8–17
Afzal K, Bagga A, Menon S, Hari P, Jordan SC (2007) Treatment with mycophenolate mofetil and prednisolone for steroid-dependent nephrotic syndrome. Pediatr Nephrol 22:2059–2065
Frange P, Frey MA, Deschênes G (2005) Immunity and immunosuppression in childhood idiopathic nephrotic syndrome. Arch Pediatr 12:305–315
Sellier-Leclerc A-L, Macher M-A, Loirat C, Guérin V, Watier H, Peuchmaur M, Baudouin V, Deschênes G (2010) Rituximab efficiency in children with steroid-dependent nephrotic syndrome. Pediatr Nephrol 25:1109–1115
Gea-Banacloche JC (2010) Rituximab-associated infections. Semin Hematol 47:187–198
Larsen CP, Freedman BI (2015) Apolipoprotein L1-associated nephropathy and the future of renal diagnostics. J Am Soc Nephrol 26:1232–1235
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This work was approved by the local ethics committee.
Conflict of interest
The author(s) declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Dehoux, L., Hogan, J., Dossier, C. et al. Mycophenolate mofetil in steroid-dependent idiopathic nephrotic syndrome. Pediatr Nephrol 31, 2095–2101 (2016). https://doi.org/10.1007/s00467-016-3400-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-016-3400-y