Abstract
Cyclophosphamide (CP) has been used for over 40 years in patients with steroid-sensitive nephrotic syndrome (SSNS) presenting frequent relapses or steroid dependence (SD). We evaluated retrospectively and tried to identify parameters possibly associated with a prolonged and sustained remission (PSR+) ≥5 years in 108 children with steroid-dependent nephrotic syndrome (SDNS) treated with oral CP. Patients had a follow-up time ≥5 years and were divided into two groups according to achievement of PSR (+ and –). Gender, histological injury, cumulative doses of CP, age of onset of illness, and start of treatment and prednisone dose on the occasion of relapse were analyzed. The overall cumulative sustained remission for 5 and 10 years was 25 and 21.6%, respectively. The only factor that influenced a PSR was the degree of SD: the group PSR+ relapsed at prednisone dose of 0.96 ± 0.51 mg/kg vs. 1.29 ± 0.59 mg/kg in group PSR– (p = 0.01). Also, patients who relapsed in the presence of prednisone doses ≤1.4 mg/kg showed a cumulative sustained remission of 43, 35, and 32.7% at 2, 5, and 10 years, respectively, versus 22.5, 12.5, and 5% in those with prednisone >1.4 mg/kg (p = 0.001). Our findings suggest that patients with SDNS who relapse on prednisone dose >1.4 mg/kg are especially prone to an unfavorable response to CP use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic nephrotic syndrome (INS) in children is characterized by high sensitivity to steroids and about 77% had minimal change disease (MCD) [1]. Approximately 80% of children with steroid-sensitive NS (SSNS) have one or more relapses, and about 50% have frequent relapses and/or steroid dependence, [2–4] requiring higher exposure to steroids. Prolonged use of steroids can cause significant side-effects such as hypertension, obesity, cataracts, psychosis, striae and growth failure [5], and alternative therapies such as cyclophosphamide (CP), levamisole, calcineurin inhibitors, and mofetil mycophenolate may be used. CP has been used for over 40 years and several clinical studies have shown its effectiveness in reducing risk of relapse and maintaining a prolonged remission [6, 7]. The therapeutic response to CP can be influenced by several factors. Children with SSNS and frequent relapses have a higher proportion of cumulative sustained remission than patients with steroid-dependent nephrotic syndrome (SDNS) [6]. Higher cumulative doses of CP appear to provide a better answer, but this is not universally reported. A study of the Arbeitsgemeinschaft für pädiatrische Nephrologie (APN) [8] showed that children with SDNS treated with 2 mg/kg/day of CP for 12 weeks showed a remission rate of 67% at 2 years compared to 22% of children treated for 8 weeks in the previous study. Moreover, Ueda [9] in a prospective study showed that children with SDNS due to MCD treated with 2 mg/kg/day of CP had a similar percentage of remission at 5 years when treated for 8 (25%) and 12 weeks (24%). Therapeutic response of CP may also be influenced by the age at treatment initiation as well as the age of onset of disease. Patients aged >5.5 years at the start of treatment were more likely to achieve sustained cumulative remission versus those younger than 5 years [10]. Patients whose nephrotic syndrome began before 3 years of age had a lower probability of sustained remission [11]. The objective of this study is to identify parameters possibly associated with a prolonged and sustained remission.
Patients and methods
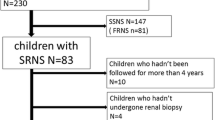
We retrospectively analyzed 108 children (69 boys and 39 girls) with SDNS who underwent therapy with oral CP. The analyzed period was between May 1974 and July 2004 at the Hospital Federal de Bonsucesso, Rio de Janeiro, Brazil. No child had previously used cytotoxic agents or any other type of adjunctive therapy for NS. The median age of disease onset and initiation of treatment were 2.95 years (range 1.1–14.1) and 4.92 years (range 2–14.94), respectively, and the median time between disease onset and start of treatment was 1.18 years (0.5–12.7). All patients had a follow-up period ≥5 years after treatment with a median of 9.5 years (5–29.2). Fifty-nine patients underwent renal biopsy and only 18 had pre-treatment biopsy. The criteria used in the definition of nephrotic syndrome were the same as in the International Study of Kidney Disease in Children (ISKDC) [12]. The initial treatment of NS, as well as that of relapse was: prednisone (2 mg/kg/day) for 4 weeks and in case of remission, the same dose was administered on alternate days for 4 weeks and thereafter, 25% reduction of every 2 weeks. We defined remission when as urine free of protein, evaluated by proteinuria ≤4 mg/ m2/h, zero or traces of albumin in dipstick probe for 3 consecutive days. Relapse was defined as a reappearance of proteinuria ≥40 mg/m2/h or Albustix 2+ or greater for 3 consecutive days. Steroid-dependency was defined as the occurrence of two consecutive relapses during alternate-day steroid treatment, or the appearance of recurrence until 14 days after its withdrawal. The CP was introduced after the induction of remission of NS by prednisone, which was continued in alternate days and tapered subsequently. The dose of CP in mg/kg/day, cumulative dose (CD) in mg/kg, or in mg/m2/body surface area (BSA), duration of treatment, and dose of prednisone in mg/kg at the time of relapse were calculated. For comparison purposes, we define prolonged and sustained remission (PSR +) as 5 or more years without relapse and no other immunosuppressive treatment. Patients were then divided into two groups: group I, with prolonged sustained remission (PSR +) and group II, those who did not achieve a PSR (PSR–). For statistical analysis, the software MedCalc® for Windows, Statistics for Biomedical Research Software version 9 was used. Student's t test was used to compare differences between means, and Mann–Whitney U test for non-parametric comparisons. Fisher's exact test to compare frequencies of qualitative variables, the ROC curve to identify the best cut-off of the CP dose/m2/BSA, prednisone dose at relapse and age of onset of illness and start of treatment, the Kaplan–Meier survival analysis to compare time of remission, log-rank test to compare survival curves, and Cox proportional hazards analysis to examine the effect of various factors on survival. A p value < 0.05 was set to indicate a significant difference.
Results
Patients' characteristics, treatment and its results are depicted in Table 1. The percentage of overall cumulative sustained remission was 34.3, 25, and 21.6% at 2, 5, and 10 years, respectively. Three patients relapsed after 5.1, 6, and 7.3 years in remission. In our study, 18 patients underwent renal biopsy prior to treatment: MCD in 15 patients, diffuse mesangial proliferation (DMP) in two patients, and focal and segmental glomerulosclerosis (FSGS) in one patient. Forty-one patients underwent renal biopsy 32 months (0.1–145) after starting treatment, with the following diagnosis: MCD (30), DMP (two), FSGS (eight) and membranous glomerulonephritis (MGN) (one). The percentage of cumulative sustained remission was similar in children who received treatment without biopsy versus those who had prior biopsy, 23.3% and 21.9% vs. 33.3% and 22.2% at 5 and 10 years, respectively (p = 0.64). There was no difference between the response to CP in relation to the MCD and other histologic lesions (p = 0.66) Table 1. Gender and duration of NS before CP did not influence the PSR (p = 0.72 and 0.88, respectively).
Concerning the degree of steroid dependence, patients who achieved a PSR + relapsed with an average dose of prednisone equal to 0.96 ± 0.51 mg/kg versus 1.29 ± 0.59 in those with RPS (p = 0.01). With a cut-off of 1.4 mg/kg, patients who relapsed on doses ≤1.4 mg/kg/prednisone, the overall cumulative probability of sustained remission was 43, 35, and 32.5% at 2, 5, and 10 years, respectively, versus 22.5, 12.5, and 5% for those who relapsed at doses >1.4 mg/kg (p = 0.001) (see Fig. 1).
The CD of CP (mg/kg) was not statistically different between those with and without PSR+. A cut-off point of 168 mg/kg (equivalent to 2 mg/kg/12 weeks), the cumulative probability of sustained remission was similar in patients treated with CD higher as well as lower than this dose (Fig. 2), despite the different total doses: 145 ± 18.66 mg/kg versus 209.96 ± 22.66 mg/kg (p < 0.0001). The median cumulative CP dose in mg/m2/BSA was similar between patients with or without RPS+ (Table 1) but the patients who used a CD/m2/BSA >5,020 mg had sustained a longer cumulative remission than those with doses ≤5,020 mg, p = 0.016 (Fig. 3). These two groups differed significantly in the total dose (5,879 ± 730 vs. 4,106 ± 639 mg, p < 0.0001). The group with CD >5,020 mg showed age at start of treatment significantly higher: 7 (2.37–14.94) versus 4.71 years (2–14.31), p = 0.0027. However, 24/31 patients (77.4%) who used a CD >5,020 mg/m2/BSA relapsed while using prednisone at a dose ≤1.4/kg mg versus 39/72 (54.1%) that had a CD ≤5,020 mg/m2/BSA (p = 0.04) at the same dose of prednisone. Age at start of treatment did not differ significantly between the patients that had or did not have a PSR: 5.7 years (2.3–14.2) vs. 4.6 years (2–14.9), p = 0.08. Considering a cut-off of 7 years, i.e., patients that began treatment with age ≥7 years, showed a higher cumulative sustained remission than those with age under 7, p = 0.017 (Fig. 4) and 24/32 (75%) of patients with age ≥7 years relapsed under prednisone daily dose ≤1.4 mg/kg vs. 39/71 (55%) of patients with age <7 years (p = 0.08). Concerning age at disease onset, no difference was observed between patients with or without PSR: 3.1 years (1.4–13.7) vs. 2.9 years (1.1–14.1) (p = 0.12). However, children whose disease onset was >2.2 years had higher cumulative sustained remission than those younger than ≤2.2 years (Fig. 5). Of patients aged >2.2 years, 66% relapsed on a daily prednisone dose ≤1.4 mg/kg vs. 51% in those younger than <2.2 years (p = 0.21).
The Cox proportional hazards regression identified the dose of prednisone ≤1.4 mg/kg at relapse was the only parameter that had an influence on cumulative sustained remission, p = 0.0043 (Table 2).
Discussion
A single-center retrospective analysis was conducted involving 108 children with SDNS treated with cyclophosphamide (CP). Of these patients, 25% remained without relapse for a period of 5 years or more and were compared to 75% of the original group that relapsed. Out of these patients that relapsed, 48, 65, and 75%, experienced relapse during the first 1, 2, and 5 years following the CP treatment, respectively. The present study showed that the grade of steroid dependence was the main factor (compared to the others analyzed in our study) related to a prolonged sustained remission. We should remark that comparison with other studies is difficult due to the different criteria adopted concerning patient selection, definition of steroid dependence, initial treatment of NS, as well as recurrence and the indication of CP use.
The authors are aware of the limitations imposed by a retrospective study design. However, both analyzed groups were homogeneous and allowed to obtain some conclusions.
In the literature, some parameters such as histological lesion, age of disease onset and initiation of treatment with CP, cumulative dose of CP in mg/kg or mg/m2/BSA were related to a successful outcome [8, 10, 11].
Renal biopsy prior to CP begun in patients with SDNS is unusual in our department. Eighty-three percent of patients began treatment without performing renal biopsy and were similar to those treated with a previous biopsy, showing that the therapeutic response to CP best correlates with steroid sensitivity than the histological lesion [13–15].
Vester [10] showed that an age at onset of treatment >5.5 years correlated with better sustained remission in children with SSNS due to MCD. Srivastava et al. [16] reported that children older than 8 years at the beginning of treatment is a good predictor of response to oral CP. Regarding age of onset, Kyrieleis [11] showed that an age <3 years predicts a low likelihood of achieving remission in children with SSNS (MCD) treated with CP. In our patients, ages at onset and initiation of treatment were similar in patients who achieved or did not achieve a prolonged sustained remission. However, despite the fact that the overall rate of sustained remission was higher when patients were older than 2.2 years at disease onset, and start of treatment older than 7 years, these factors are not significant after the Cox proportional-hazard regression analysis. An age <4 years at the start of SSNS is associated with an increased likelihood of frequent relapses and a greater time interval to achieve remission [17]. Recently, Andersen et al. [18] showed that an early age of onset of SSNS and male gender were associated with a high risk of steroid-dependence and frequent relapses. Possibly a better response to CP in patients whose NS began and started CP later would be explained by the natural course of disease.
An important aspect is that side-effects of CP are related to higher cumulative dose [6] and the ideal would be to use a dose as low as possible to get a better effect. There are controversies in the literature in relation to cumulative dose and its effectiveness. Higher CDs showed a higher recurrence-free period [8, 19, 20] while others have not confirmed this finding [9, 10]. The study of APN [8] showed better response with higher cumulative dose. Ueda [9] in contrast, showed in a prospective study a remission rate of 25 and 24% at 5 years in patients with SDNS with CDs of 112 and 168 mg/kg, respectively. Kyrieleis [11] and Kemper [21] found a remission rate of 35 and 30% at 2 years, with cumulative doses of 168 mg/kg. Our data showed no benefit of CP treatment with a higher cumulative dose in mg/kg. The best response of patients in the APN study could be explained by patients’ characteristics: predominance of females, which is not common in patients with SDNS, age of onset of disease at an older age, as well as at treatment start in opposition to our study and others [9, 21]. Regarding the CD in mg/m2/BSA,Vester [10] found that patients using CD >5,040 mg had remission’s rates sustained at 10 years of 45 versus 11% from who used doses <5,040 mg. Patients who used doses >5,040 mg were older at age of start of treatment with CP than those patients who used CD <5,040 mg/m2/BSA. Vester speculated that preschool children may have been undertreated, but this study included patients with SDNS and patients with frequent relapsing NS, which could have influenced the results. Our study showed that a CD in mg/m2 of CP was not different between groups with or without PSR, but with a cut-off of 5,020 mg, the patients who used doses >5,020 mg showed a probability of sustained remission significantly higher than those with doses <5,020 mg. These patients had a higher age at start of treatment and the majority (77.4%) recurred with treatment doses of prednisone <1.4 mg/kg, which could have provided a better response.
The present study showed that the only factor related to a cumulative sustained remission ≥5 years was the degree of steroid dependence. Patients who relapsed at doses of prednisone ≤1.4 mg had a higher percentage of cumulative sustained remission versus those who relapsed with doses >1.4 mg/kg. Given the unfavorable results of treatment with CP in patients that relapsed with a dose of prednisone >1.4 mg/kg, we wonder whether cyclophosphamide should be indicated in these patients, thus avoiding possible side-effects of the drug.
Abbreviations
- NS:
-
Nephrotic syndrome
- MCNS:
-
Minimal change nephrotic syndrome
- CP:
-
Cyclophosphamide
- SPR:
-
Sustained prolonged remission
- SDNS:
-
Steroid-dependent nephrotic syndrome
- SSNS:
-
Steroid-sensitive nephrotic syndrome
- ISKDC:
-
International Study of Kidney Disease in Children
- APN:
-
Arbeitsgemeinschaft für pädiatrische Nephrologie
References
(1981) The primary nephrotic syndrome in children: Identification of patients with minimal change nephrotic syndrome from initial response to prednisone; A report of International Study of Kidney Disease in Children. J Pediatr 98:561–564
Koskimies O, Vilka J, Rapola J, Hallman N (1982) Long-term outcome of primary nephrotic syndrome. Arch Dis Child 57:544–548
Tarshish P, Tobin JN, Bernstein J, Edelamamn CMJ (1977) Prognostic significance of the early course of minimal change nephrotic syndrome: report of the International Study of Kidney Disease in Children. J Am Soc Nephrol 8:769–776
Hodson EM, Willis NS, Craig JC (2008) Non-corticosteroid treatment for nephrotic syndrome in children. Cochrane Database Syst Rev:CD002290
Hodson EM, Craig JC, Willis NS (2005) Evidence-based management of steroid-sensitive nephrotic syndrome. Pediatr Nephrol 20:1523–1530
Latta K, Von Schnakenburg C, Ehrich JHH (2001) A meta-analysis of cytotoxic treatment in frequently relapsing nephrotic syndrome in children. Pediatr Nephrol 16:271–282
Cameron JS, Chantler C, CS OGG, White RHR (1974) Long-term stability of remission in nephrotic syndrome after treatment with ciclophosphamide. BMJ 4:7–11
Report of Arbeitsgemeinschaft fur pädiatrische Nephrologie (1987) Cyclophosphamide treatment of steroid dependent nephrotic syndrome: comparison of eight week with 12 week course. Arch Dis Child 62:1102–1106
Ueda N, Kuno K, Ito S (1990) Eight and 12 week courses of cyclophosphamide in nephrotic syndrome. Arch Dis Child 65:1147–1150
Vester U, Kranz B, Zimmermann S, Hoyer FP (2003) Cyclophosphamide in steroid-sensitive nephrotic syndrome: outcome and outlook. Pediatr Nephrol 18:661–664
Kyrieleis HA, Levtchenko EN, Wetzels JF (2007) Long-term outcome after cyclophosphamide treatment in children with steroid-dependent and frequently relapsing minimal change nephrotic syndrome. Am J Kidney Dis 49:592–597
International Study of Kidney Disease in Children (1978) Nephrotic syndrome in children: Prediction of histopathology from clinical and laboratory characteristics at time of diagnosis. Kidney Int 13:159–165
Gulati S, Sharma AP, Sharma RK, Gupta A, Gupta RK (2002) Do current recommendations for kidney biopsy in nephrotic syndrome need modifications? Pediatr Nephrol 17:404–408
Stadermann MB, Lilien MR, van de Kar NC, Monnens LA, Schröder CH (2003) Is biopsy required prior to cyclophosphamide in steroid-sensitive nephrotic syndrome? Clin Nephrol 60:315–317
Mattoo TK (1991) Kidney biopsy prior to cyclophosphamide therapy in primary nephrotic syndrome. Pediatr Nephrol 5:617–619
Srivastava RN, Agarwal RK, Chowdhary VP, Moudgil A, Bhuyan UN, Sunderram KL (1987) Cyclophosphamide therapy in frequently relapsing nephrotic syndrome with and without steroid dependence. Int J Pediatr Nephrol 6:245–250
Kabuki N, Okugawa T, Hayakawa H, Tomizawa S, Kasahara T, Uchiyama M (1998) Influence of age at onset on the outcome of steroid-sensitive nephrotic syndrome. Pediatr Nephrol 12:467–470
Andersen RF, Thrane N, Noergaard K, Rytter L, Jespersen B, Rittig S (2010) Early age at debut is a predictor of steroid-dependent and frequent relapsing nephrotic syndrome. Pediatr Nephrol 25:1299–1304
Barratt TM, Cameron JS, Chantler C, Ogg CS, Soothill JF (1973) Comparative trial of 2 weeks and 8 weeks cyclophosphamide in steroid-sensitive relapsing nephrotic syndrome of childhood. Arch Dis Child 48:286–290
Pennisi AJ, Grushkin CM, Lieberman E (1976) Cyclophosphamide in the treatment of idiopathic nephrotic syndrome. Pediatrics 57:948–951
Kemper MJ, Altrogge H, Ludwig K, Timmermann K, Müller-Wiefel DE (2000) Unfavorable response to cyclophosphamide in steroid-dependent nephrotic syndrome. Pediatr Nephrol 14:772–775
Acknowledgements
We wish to thank Lilimar da Silveira Rioja, M.D., for her support at the Department of Pathology, Hospital Federal Servidores do Estado, Rio de Janeiro and Marcelo de Sousa Tavares, M.D., PhD (UFMG) for reviewing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zagury, A., de Oliveira, A.L., de Moraes, C.A.P. et al. Long-term follow-up after cyclophosphamide therapy in steroid-dependent nephrotic syndrome. Pediatr Nephrol 26, 915–920 (2011). https://doi.org/10.1007/s00467-011-1825-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-011-1825-x