Abstract
The purpose of this study was to identify characteristics of patients with steroid-sensitive nephrotic syndrome (SSNS) that point to a high risk of frequent relapsing (FR) or steroid-dependent (SD) SSNS. A retrospective analysis of 54 consecutive patients with SSNS was performed. In this cohort, the incidence of idiopathic NS was 1.9/100,000, age at debut was 5.5 years, and the mean follow-up was 4.0 years. A total of 56% (30/54) of our patients were classified with FR/SD SSNS. FR/SD patients were significantly younger at debut than non-FR/SD patients (3.5 vs. 8.5 years, respectively; p < 0.002). Males were overrepresented in the FR/SD group (69 vs. 38%; p = 0.03). No differences were found in terms of haematuria, hypoalbuminaemia, or days to achieve remission. In total, 31 and 23 patients were on a 6 + 6-week (pred-long) and 4 + 4-week (pred-short) steroid treatment regimen, respectively. There was a reduction in the number of FR/SD patients in the pred-long group relative to the pred-short group (38 vs. 80%, respectively). In the pred-long group, the 12 FR/SD patients were younger than the 19 non-FR/SD patients (4.4 ± 3.1 vs. 8.4 ± 4.1 years; p<0.005). Low age at debut and male gender was associated with a high risk of SD/FR in this unselected series of SSNS patients despite the prolongation of the steroid course at debut of SSNS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Childhood idiopathic nephrotic syndrome (NS) is characterized by minimal change on light microscopic examination in approximately 80% of patients [1] and by steroid responsiveness in approximately 90% of patients [2]. Despite the favourable long-term renal outcome in steroid-sensitive nephrotic syndrome (SSNS), the road to stable remission is often complicated. The relapsing nature of the disease presents a major challenge, and 60% of the patients have a high relapse rate [3], with a subsequent risk of steroid toxicity. Several attempts have been done to identify patient characteristics at debut associated with a high risk of frequent relapsing (FR) or steroid-dependent (SD) NS. An early identification of these patients would enable the clinician to give more accurate information to the patient and the family on the prognosis and the risk of long-term immunosuppressive therapy. In addition, early prognostic indicators may enable the selection of patients who would benefit from supplementing the treatment regimen with immunosuppressive agents and be an inclusion criterion for planning new randomized studies aimed at improving treatment protocols. The duration from initial steroid therapy to remission, relapses during the first half year after disease onset, low serum protein level and hematuria have been proposed as independent risk factors [4–6]. Additionally, several studies have investigated the association of young age at the initial episode of NS and a complicated relapse pattern, but the results have been conflicting [5, 7, 8].
The aim of this study was to determine clinical characteristics at the initial episode of SSNS that may be correlated to an adverse relapse pattern in an unselected, population-based series of patients.
Material and methods
The cohort of patients enrolled in this study was identified at the four paediatric departments in the Central Region of Denmark, which cover a population of 227,000 children aged 0–14 years (source: Key indicators, Statistic Denmark, www.dst.dk) using the ICD 10 codes N00-N08 (“glomerular disease”). Standard computerized inpatient and outpatient statistics listed patients admitted to the departments between 1 January 1997 and 31 December 2008 with the relevant ICD 10 codes. The medical records of all listed patients were reviewed to identify and study children with SSNS.
The inclusion criteria were idiopathic SSNS, age <15 years at disease debut, residency in the geographical area covered by the four paediatric departments and no evidence of underlying systemic disease. Exclusion criteria were steroid-resistant NS (SRNS), low C3 complement, post-infectious glomerulonephritis, vasculitis, such as Henoch–Schönlein nephritis, or specific glomerulonephritis, such as dense deposit disease.
Definitions
Nephrotic syndrome was defined as proteinuria >40 mg/m2/h, serum albumin <25 g/L, oedema formations and hyperlipidaemia. Relapse was defined as three consecutive days with 3+ on urinary albumin dipstick. SRNS was present if proteinuria continued despite 4 weeks of prednisone treatment. SDNS was defined as episodes with relapse during the tapering down of steroid treatment or within 14 days of ending treatment [9]. FR nephrotic syndrome was the occurrence of more than two relapse episodes during the first half year after disease debut or four episodes during a random subsequent year [4]. Remission was achieved when the urinary albumin dipstick was negative on three consecutive days.
Initial presentation data included age, gender and ethnic origin. Renal function was estimated by the Schwartz formula, with a k value = 0.55 (estimated glomerular filtration rate, eGFR) [10]. Data on plasma albumin and creatinine were collected. The level of proteinuria at the initial episode was based on 24-h urine collections. Haematuria was defined as +1 or more on the urinary deep stick.
Treatment regimens
The initial NS episodes were treated differently depending on the time of debut. Patients with debut before 2003 received a pred-short treatment regimen, which consists of 4 weeks of daily prednisone treatment (2 mg/kg/day or 60 mg/m2/day, maximum 80 mg/day) followed by 4 weeks of alternate-day treatment (40 mg/m2). From 2003 to 2009, the initial episode was treated with a pred-long treatment regimen (60 mg/m2/day, maximum 80 mg/day) for 6 weeks followed by 6 weeks of alternate-day prednisone (40 mg/m2). Relapses were treated with daily prednisone (60 mg/m2/day) until remission was achieved, followed by 40 mg/m2 on alternate days for 4 weeks. Indication for second-line immunosuppressive therapy was FR/SD and included cyclophosfamide, cyclosporine A (CyA), tacrolimus (Tac) and mycophenolat mofetile (MMF).
Statistical analysis
Statistical analysis was performed using Stata software, release 10 (College Station, TX) for Windows. Normally distributed data were expressed as means and standard deviations (SD). Comparison between groups was performed using Student’s t test. Data not normally distributed were expressed as medians and ranges, and comparisons between such data were performed using the Wilcoxon rank sum test. For binary data, the chi-squared test was used to test the hypothesis of no association, and when data were sparse Fisher’s exact test was applied. The relationship between age at disease debut and the risk of FR/SD were analyzed by linear regression analysis. The model was checked by diagnostic plots of the residuals. p<0.05 was considered to be statistically significant.
Results
A total of 76 patients were admitted to the four departments between 1 January 1997 and 31 December 2008 with a diagnosis of NS. Of these, 62 were defined as idiopathic (3 with mesangial proliferative glomerulonephritis, 5 SRNS patients and 54 SSNS patients). The medical record of one patient was unavailable. The incidence of idiopathic NS was 1.9/100,000 children (age 0–14 years) and the prevalence was 10.1/100,000.
Fifty-four patients (43 Caucasian, 4 Asian, 3 Arabic, 2 African, 2 mixed) met the criteria of SSNS and were included in the study. The male:female ratio was 1.2:1 (29:25). The median age at debut was 5.5 years (range 14 months to 14 years and 4 months), and the median follow-up time was 4.0 years (range 3 months to 19 years). Two patients with debut in 2008 were followed for less than 12 months when inclusion was stopped with the collection of data on 31 December 2008. At latest contact, December 2009 and January 2010, respectively, these patients had had no further episodes. One patient was lost to follow-up after 2 years and was classified as steroid dependent at that time.
In total, 56% (30/54) of the SSNS patients had frequent relapses or were steroid dependent (FR/SD group), and 29 of these 30 patients were treated with immunosuppressive regimens other than prednisone. None of the patients in the non-FR/SD group received other immunosuppressive therapy in addition to steroids. The relapse rate in the FR/SD group was significantly higher than that in the non-FR/SD group (1.4±0.82 vs.0.28±0.44 relapse/year, respectively; p < 0.01, Student’s t test).
The patients’ clinical presentation characteristics are shown in Table 1. The median age of the patients at debut was significantly lower in the FR/SD group than in the non-FR/SD group [3.5 (range 1–14) vs. 8.5 (range 1–14) years, respectively; p = 0.002, Wilcoxon rank sum test. Males were overrepresented in the FR/SD group compared to the non-FR/SD group (20/30 vs. 9/24, respectively; p = 0.03, chi-square test). In the FR/SD group, there were no differences in the number of males treated with pred-short compared to females treated with pred-long (males 11/20 vs. females 6/10; p = 0.5, Fisher exact test). At debut, the median age of the males was not significantly lower than that of the females [5.0 (range 1–14) vs. 7.0 (range 1–14), respectively; p = 0.26, Wilcoxon rank sum test].
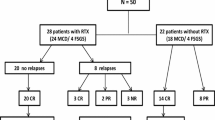
The risk of FR/SD was related to low age at initial presentation. In total, 88% of the patients with debut before the age of 4 years were subsequently classified as FR/SD. Two different treatment regimens were applied, and pred-long significantly reduced the relapse frequency during the first year after debut (Fig. 1). A total of 31 patients were treated with pred-long and 23 with pred-short (Fig. 2). The mean age in the pred-long group was 6.9 ± 4.1 years, which was not significantly different from the mean age of 5.1 ± 4.0 years in the pred-short group (t test p = 0.11). In the pred-short group, 80% (18/23) of the patients were FR/SD, which was significantly higher than the proportion in the pred-long group (38%, 12/31) (p < 0.006, Fisher’s exact test). In the pred-long group, patients with FR/SD were significantly younger at debut than non-FR/SD patients (4.4 ± 3.1 vs. 8.4 ± 4.1 years, respectively; t test p < 0.005). To avoid the influence of the steroid protocol used, we included only the 31 patients in the pred-long group in an analysis of the relationship between age at debut and the risk of FR/SD using a linear regressions model (n = 31, y = 0.85 − 0.17x, r 2= 0.93, p = 0.009) (Fig. 3). This analysis revealed that the youngest patients had the highest risk of FR/SD and that the risk declined with increasing age at first episode of SSNS.
The number of relapses during the first year was reduced in patients treated with 60 mg/m2/day for 6 weeks followed by alternate-day 40 mg/m2 (Pred-long) compared to the patients treated with 60 mg/m2/day or 2 mg/kg/day for 4 weeks followed by alternate-day prednisone for 4 weeks (Pred-short). Mean relapse number in Pred-long was 0.77 ± 1.05 relapse/year versus 2.0 ± 1.5 relapse/year in the Pred-short group. The difference was significant at p < 0.001 (Student’s t test)
A total of 54 patients were included, and 31 were treated with the pred-long treatment regimen and 23 with pred-short treatment regimen. Mean age in the pred-long and pred-short groups was 6.9 ± 4.1 vs. 5.1 ± 4.0 years, respectively (p = 0.11, t test). In the pred-long group, the mean age of frequent relapsing/steroid-dependent (FR/SD) nephrotic syndrome (NS) patients was 4.4 ± 3.1 versus 8.4 ± 4.1 years for the non-FR/SD patients (p < 0.005, t test). In the pred-short group, there was no significant difference in mean age between FR/SD and non-FR/SD patients (6.6±2.4 vs. 4.7± 4.3 years, respectively; p = 0.36, t test)
The age at initial episode of NS and the number of patients with subsequent FR/SD in the 31 patients treated with the pred-long regimen. Grey bars Total number of patients with debut of NS at a given age, black bars number of patients with FR/SD related to the age at NS debut. The ratio of patients with FR/SD declines with increasing age at debut of NS
A total of 51% of all patients had haematuria at initial presentation, but no differences were found between the non-FR/SD group and the FR/SD group. No significant differences were seen between the groups in terms of duration from initiation of steroid treatment to remission or the level of plasma albumin at initial presentation (Table 1).
At last contact, all patients had normal renal function, and only two patients were still treated with antihypertensive therapy to stay normotensive.
Discussion
Steroid-sensitive nephrotic syndrome in childhood is generally considered to be a benign disorder with an excellent long-term renal outcome, a finding also demonstrated in the unselected patient population presented here. Nevertheless, more than half of the patients suffer from multiple relapses. The results of our study demonstrate that debut at early age and male gender constitute a significant risk of FR/SD nephrotic syndrome.
The incidence of idiopathic NS has been surprisingly stable for the last few decades and independent of the population studied. We found an incidence in our region of 1.9/100,000, which is much similar to the 2/100,000 and 2.3/100,000 reported in the 1950s in the UK and USA, respectively [11, 12]. Recently, an incidence of 1.9/100,000 was reported from New Zealand [13].
One interesting finding of this study was the relationship between age at initial episode and the number of patients subsequently developing FR/SD nephrotic syndrome. The ratio of patients with FR/SD declined with a higher age at debut while nearly 90% of patients with debut under the age of 4 years developed FR/SD. The association between young age and relapses has previously been proposed by Takeda et al. [5] and Kabuki et al. [7]. Takeda reported that the sustained cumulative remission rate is significantly lower when patients present with NS at 7 years of age or younger. One disadvantage in the methodology by Takeda is that the infrequent relapsing patients were included in the group of relapsing patients, and there is therefore a potential risk of overestimating the number of patients developing a complicated disease course from a clinical perspective. To ensure that our approach was clinically relevant, we focused on patients with FR/SD because of the significant risk of steroid toxicity in this patient population and, subsequently, a need for second-line immunosuppressive therapy. Kabuki et al. reported that a subgroup of patients with debut of NS before the age of 4 years had a higher risk of frequent relapse, as revealed by a Kaplan–Meier analysis. As demonstrated here and elsewhere [14], prolongation of the initial steroid treatment course decreases the first-year relapse rate and, more importantly, it also reduces the proportion of patients subsequently being FR/SD from 80% to approximately 40%. This has previously been reported in patients suffering from frequent relapses [15]. However, our study illustrates that despite prolongation of the initial steroid treatment protocol, most patients with debut at a low age will still suffer from FR/SD. It must be noted, however, that our finding carries the limitations of all retrospectively designed studies and that the number of included patients was limited.
In contrast to the findings just mentioned, Constantinescu et al. did not find that age at debut influenced the relapse pattern [8]. This difference may be a consequence of the longer follow-up in our study compared to that of Constantinescu et al. who only studied the relapse pattern in the first year of disease and thereby may have underestimated the true number of patients with FR/SD. An International Study of Kidney Disease in Children (ISKDC) report from the early 1980s also did not find a correlation between age at debut and subsequent frequent relapses [4]. This study identified 389 patients with minimal change nephrotic syndrome, but 171 patients were excluded because of steroid resistance (27), incomplete data (99) or treatment with other immunosuppressive therapy (45). One major advantage of our study is that the enrolled patients were from a well-defined and unselected population, thereby limiting the risk of selection bias, and that we lost only one patient to follow-up.
Contrary to the results reported by Yap et al. [6], we did not find that the duration from initiation of steroid therapy to remission correlated with the risk of FR/SD. This discrepancy may be related to the steroid regimen used. A significant number of the patients included by Yap were treated by the 40-day drug course proposed by Arneil in 1968 [16]. This regimen reduces the steroid dosage after 10 days irrespective of the response on proteinuria, thereby increasing the risk of an insufficient steroid concentration and, consequently, prolongation of the time to achieve remission. Additionally, the ethnic population described by Yap differs significantly from the population described here. Indeed, the ethnic composition of our study cohort may limit the relevance of our findings to a population that is predominantly Caucasian.
Another interesting finding of this study was that the males were more at risk of developing FR/SD. Lewis et al. reported a similar tendency in 68 patients observed in the UK from 1963 to 1976 [17]. This finding may be a consequence of the overall predominance of male patients with NS, although this seems to be less pronounced here than in previously reports [18].
The findings presented here may suggest that steroids should be supplemented with second-line immunosuppressive therapy at the first episode of NS in certain groups of patients where even prolongation of the steroid protocols seems insufficient to significantly reduce the risk of FR/SD. A randomized trial by Hoyer et al. found a significantly lower relapse rate in a patient group treated with prednisone and supplementary CyA for 8 weeks compared to steroids alone at the initial episode of NS. The beneficial effect was most pronounced in patients younger than 7 years [19]. However, the effect was lost after 9 months, indicating that the initial CyA therapy should be prolonged to achieve a better sustained remission rate.
In conclusion, we have demonstrated that low age at debut and male gender is associated with an increased risk of FR/SD in an unselected population of Danish SSNS patients and that the relation between young age and FR/SD persisted despite a prolongation of the initial steroid protocol. These data must be validated in a prospective study, and further randomized studies are necessary to evaluate whether the use of supplementary immunosuppressive treatment to prednisone at first episode of NS will lower the risk of FR/SD without any unacceptable short- or long-term risks.
Abbreviations
- CyA:
-
Cyclosporine A
- eGFR:
-
Estimated glomerular filtration rate
- ESRD:
-
End stage renal disease
- FR:
-
Frequent relapsing
- MMF:
-
Mycophenolat mofetile
- NS:
-
Nephrotic syndrome
- SD:
-
Steroid dependent
- SSNS:
-
Steroid-sensitive nephrotic syndrome
- Tac:
-
Tacrolimus
References
Report of the International Study of Kidney Disease in Children (1978) Nephrotic syndrome in children: prediction of histopathology from clinical and laboratory characteristics at time of diagnosis. A report of the International Study of Kidney Disease in Children. Kidney Int 13:159–165
Report of the International Study of Kidney Disease in Children (1981) The primary nephrotic syndrome in children. Identification of patients with minimal change nephrotic syndrome from initial response to prednisone. A report of the International Study of Kidney Disease in Children. J Pediatr 98:561–564
Ruth EM, Kemper MJ, Leumann EP, Laube GF, Neuhaus TJ (2005) Children with steroid-sensitive nephrotic syndrome come of age: long-term outcome. J Pediatr 147:202–207
Report of the International Study of Kidney Disease in Children (1982) Early identification of frequent relapsers among children with minimal change nephrotic syndrome. A report of the International Study of Kidney Disease in Children. J Pediatr 101:514–518
Takeda A, Matsutani H, Niimura F, Ohgushi H (1996) Risk factors for relapse in childhood nephrotic syndrome. Pediatr Nephrol 10:740–741
Yap HK, Han EJ, Heng CK, Gong WK (2001) Risk factors for steroid dependency in children with idiopathic nephrotic syndrome. Pediatr Nephrol 16:1049–1052
Kabuki N, Okugawa T, Hayakawa H, Tomizawa S, Kasahara T, Uchiyama M (1998) Influence of age at onset on the outcome of steroid-sensitive nephrotic syndrome. Pediatr Nephrol 12:467–470
Constantinescu AR, Shah HB, Foote EF, Weiss LS (2000) Predicting first-year relapses in children with nephrotic syndrome. Pediatrics 105:492–495
Gordillo R, Spitzer A (2009) The nephrotic syndrome. Pediatr Rev 30:94–105
Schwartz GJ, Haycock GB, Edelmann CM Jr, Spitzer A (1976) A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 58:259–263
Arneil GC (1961) 164 children with nephrosis. Lancet 2:1103–1110
Rothenberg MB, Heymann W (1957) The incidence of the nephrotic syndrome in children. Pediatrics 19:446–452
Wong W (2007) Idiopathic nephrotic syndrome in New Zealand children, demographic, clinical features, initial management and outcome after twelve-month follow-up: results of a three-year national surveillance study. J Paediatr Child Health 43:337–341
Hodson EM, Knight JF, Willis NS, Craig JC (2005) Corticosteroid therapy for nephrotic syndrome in children. Cochrane Database Syst Rev CD001533
Ehrich JH, Brodehl J (1993) Long versus standard prednisone therapy for initial treatment of idiopathic nephrotic syndrome in children. Arbeitsgemeinschaft fur Pädiatrische Nephrologie. Eur J Pediatr 152:357–361
Arneil GC (1968) Management of the nephrotic syndrome. Arch Dis Child 43:257–262
Lewis MA, Baildom EM, Davis N, Houston IB, Postlethwaite RJ (1989) Nephrotic syndrome: from toddlers to twenties. Lancet 1:255–259
Heymann W, Makker SP, Post RS (1972) The preponderance of males in the idiopathic nephrotic syndrome of childhood. Pediatrics 50:814–817
Hoyer PF, Brodehl J (2006) Initial treatment of idiopathic nephrotic syndrome in children: prednisone versus prednisone plus cyclosporine A: a prospective, randomized trial. J Am Soc Nephrol 17:1151–1157
Financial disclosure
None
Conflict of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Andersen, R.F., Thrane, N., Noergaard, K. et al. Early age at debut is a predictor of steroid-dependent and frequent relapsing nephrotic syndrome. Pediatr Nephrol 25, 1299–1304 (2010). https://doi.org/10.1007/s00467-010-1537-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-010-1537-7