Abstract
Paediatric registries worldwide report that congenital abnormalities of the kidney and urinary tract (CAKUT) account for approximately 50% of end-stage renal failure and other congenital and familial diseases account for another 20% (together 70%). Does the same hold true for young adults? Almost nothing has been published about primary renal disease in adults who have reached end-stage before 30 years of age. I have reviewed the UK renal registry (2000–2006) and the United States Renal Data System (USRDS) data base (2005) to answer this question. While paediatric registries have reduced the number of children with ‘no specific diagnosis’ from 39% in 1976 to fewer than 5%, the adult registries still report rates of 20–27%, which rise to 28–36% when all unspecified groups, predominantly ‘glomerulonephritis (GN) (histologically not examined)’, are considered together. For UK data, this rise in ‘no specific diagnosis’ mirrors a fall in CAKUT to 26% for the age group 18–21 years. According to USRDS data, CAKUT falls from 31% for ages 0–19 years to only 5% for ages 20–30 years. Nephrologists probably under-diagnose CAKUT in young adult patients, and this diagnosis can account for many of the 30% that currently have no specified primary renal disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Registry data from around the world, recording the primary renal disease (PRD) causing end-stage renal failure (ESRF) in children, show that approximately 50% of cases are owing to ‘congenital abnormalities of the kidney and urinary tract’ (CAKUT) and a further 20% to ‘other congenital and inherited diseases’ (CONGEN) (Table 1, [1–26]). These proportions still hold true for children aged 12–15 years [British Association for Paediatric Nephrology (BAPN) data, Table 2] [27].
There seems little reason that this should not also hold true for adult populations of up to 25–30 years of age, when other diagnoses such as diabetes become significant. Reports from adult registry data, however, give almost no information on PRD categorised by ages at ESRF. Moreover, almost all adult registries include a large group reported as ‘aetiology unknown’ or ‘2 small kidneys’. This value is generally around 20%.
The BAPN has recently taken the view that “renal dysplasia, with or without vesico-ureteric reflux (VUR), is the most common cause of ESRF in the childhood population. On the basis that the clinical overlap between reflux nephropathy and renal dysplasia is so great and that clinical distinction between these two groups is quite arbitrary, these two categories have been united. In doing so, they account for 32.8% of childhood ESRF [in the UK]” [28].
When paediatricians ask adult nephrologists “how common is CAKUT in young adults?”, the answer is “probably quite common but I’m not really sure”. In this review I look at the published data that might answer this question and analyse the European Dialysis and Transplant Association (EDTA) returns from the UK renal registry for the period 2000–2006 and the United States Renal Data System (USRDS) data for 2005.
Methods
The UK renal registry provided an Excel file of three columns: (1) age at ESRF; (2) PRD; (3) ethnic group, when recorded, for all patients aged 18 years and over and registered with them in the period 2000–2006. There were 33,615 patients, of whom 1,555 had been aged 18–29 years at onset of ESRF.
The USRDS provided “Incident counts of Reported ESRD Patients by demographic characteristics & detailed primary diagnosis” for each year from 1991 to 2005. The data for 2005 was analysed for the age groups 0–19 years (n = 1,112) and 20–30 years (n = 2,521). (The data reported here were supplied by the USRDS. The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy or interpretation of the US government.)
For all databases missing data were excluded. Thus, if data on 1,000 patients were provided but the PRD was missing (not provided) in 50 cases, the denominator for analysis of that set of data would be 950.
Congenital abnormality of the kidney and urinary tract (CAKUT) is, in summary, renal dysplasia/reflux nephropathy with or without obstructive uropathy. The diagnoses from the EDTA and USRDS codes used for this group are shown in the Supplementary Tables.
Other congenital and familial diseases (CONGEN) are the tubular, cystic, other hereditary nephropathies, and metabolic diseases, shown in the Supplementary Tables.
Glomerulonephritis (GN): when no specific diagnosis was recorded it was assumed that the diagnosis was unknown/uncertain/unspecified. This was noted, and these cases were added to a summary group called ‘Unknown’ (see below). Thus, the following categories were all classed as “Unknown”:
For the EDTA report [29]: (1) no histological examination; (2) chronic GN with other histological lesions; (3) advanced chronic GN, sclerosing and other types.
For the UK Renal Registry: (1) Glomerulonephritis; histologically NOT examined; EDTA code 10; (2) Glomerulonephritis; histologically examined, not given above, code 19.
For the USRDS: (1) Glomerulonephritis (GN) (histologically not examined) (USRDS code 4).
Those with Alport’s syndrome and all patients identified as having congenital or familial nephropathy were included in the group “Other congenital and familial diseases” (CONGEN) (EDTA codes 50, 51, 59; USRDS codes 43, 47, 48).
Unknown: most registries have one or more categories for “aetiology uncertain”/“no specific diagnosis”. Thus,
For the UK Renal Registry: (1) Chronic renal failure; aetiology uncertain (EDTA code 0). To this “unknown” group have been added (2) Other identified renal disorders (but not specified), code 99, plus the two histology categories (shown above, codes 10, 19).
For the USRDS: (1) Hypertension unspecified with renal failure, code 35; (2) Etiology uncertain, code 69. To these “unknown” groups the following has been added: (3) Glomerulo-nephritis (GN) (histologically not examined), code 4.
For the EDTA (1975): (1) Others (not specified), plus the three histology categories (shown above).
Paediatric data
Background
In 1976 the annual EDTA report from its Paediatric Registry gave details of PRD in 1,111 children up to the age of 16 years. CAKUT accounted for 30%, and other familial and congenital diseases (CONGEN) 13%, while 39% were unspecified (“Unknown”) [29] (Table 2).
In 2004 an EDTA report from 12 countries of 3,184 children gave values of 32%, 18% and 11%, respectively [25]. The main difference from the earlier study was the reduction in the numbers of those with ‘glomerulonephritis’, from 39% to 23%. In 1976 the great majority of them (68%) had not undergone biopsy; the 2004 report does not give any further details of this group. USRDS data (2005) for the age group 0–19 years give very similar values (see Table 2).
Current situation
A consistent but different conclusion is found when individual national paediatric registries are reviewed today (Table 1).
From data in Table 1, the median upper age of children in registries was 16 years (range of upper age 12–22 years); the median male majority was 61% (51–74%); the median percentage with CAKUT was 51%, and the median total of CAKUT plus other familial and congenital diseases (CONGENs) was 67%.
There are three points to be made:
-
1.
There is a consensus that, worldwide, CAKUT accounts for approximately 50% of renal failure, and other congenital and familial diseases account for 20% (together 70%).
-
2.
The inadequacy of diagnosis coding systems—such as the old EDTA system, which has seven forms of ‘pyelonephritis’ to choose from—coupled with routine compulsory reporting to large registries means that USRDS data and EDTA data appear to under-report the true situation.
-
3.
China seems to be genuinely different, with glomerulonephritis as the major cause of renal failure (this may also be true for Nigeria). Data reported from China [7] and Japan [13] suggest that CAKUT, at least that associated with bladder outflow obstruction, is much less common than in the West, and the latter also seems to apply to Black Africans.
The absence of obstructive uropathy in Japan is confirmed in the 1998 report of the Japanese National registry on paediatric patients with ESRF [13]. Out of 582 children, a maximum of four boys had posterior urethral valves (PUVs) (0.7%) compared with 11.3% in the UK data [27]. In contrast, non-obstructive renal dysplasia was similar in the two populations, with 34.4% in Japan and 31.8% in the UK.
Foreground
There are now probably many countries that collect excellent data, but three have reported their data in a sufficiently comprehensive form to warrant detailed analysis and comparisons. From Italy there is the ItalKid study [8], from the UK the British Association for Paediatric Nephrology (BAPN) [27], and, in North America, there is the North American Pediatric Renal Transplant Cooperative Study (NAPRTCS) [1]. The Italian and US registries are of chronic renal insufficiency (creatinine clearance <75 ml/min per 1.73 m2 body surface area), although the mean estimated creatinine clearances at registration were 42 ml/min per 1.73 m2 and 39 ml/min per 1.73 m2, respectively.
These data are broadly very much as expected from the consensus above (see Table 2), but with some exceptions.
-
1.
All report total glomerulonephritis rates of up to only 20%. For the UK and American series the glomerulonephritis reported as unspecified “chronic” is down to 1%, and the series also have focal segmental glomerulosclerosis (FSGS) as 9%, accounting for almost half the glomerulonephritis.
-
2.
“Unknown” rates are reported in the range 2.6–4.5%, although this increases by at least 1% when “unspecified chronic glomerulonephritis” is added in.
-
3.
NAPRTCS report only 9.5% for “other CONGEN”, but they also have a group of 15% of “Other” (unspecified) diseases.
Summary
When data from children (up to 20 years of age) are collected accurately, it appears that CAKUT is approximately 50%, other CONGENs 20%, unknown is 4–5%, and glomerulonephritis decreases from around 35–40% to 20%, with only 1–2% of glomerulonephritis being uncharacterised. The fact that almost half the glomerulonephritis is reported as “FSGS” still raises the question of how accurately this is reported in the sense of “Focal segmental glomerulosclerosis with nephrotic syndrome in children [EDTA code 11]”.
Hypothesis
My analysis is driven by several opinions:
-
1.
Adult nephrologists are probably not well aware that CAKUT can commonly present in adulthood. In fact, only 10–20% of adults with ESRF as a consequence of reflux nephropathy/renal dysplasia present in childhood [30].
-
2.
Adult nephrologists are unfamiliar with the possibility that congenital chronic tubular disease can cause ESRF. Such patients have slowly progressive disease, with minimal symptoms, minimal proteinuria, and no peripheral oedema, and they often present at end stage when a biopsy is not feasible or is uninterpretable.
-
3.
Until recently, many nephrologists used the acronym FSGS as a clinical expression or clinical diagnosis to signify the severe nephrotic syndrome with progressive renal failure that we now call primary FSGS. The concept that several other conditions, such as reflux nephropathy, can lead to a secondary FSGS is only now being appreciated. This means that the term FSGS used as a PRD diagnosis is likely to contain a large mixture of primary conditions—with only a minority accompanied by nephrotic syndrome.
-
4.
Hypertension is not a cause of ESRF in young, non-black adults.
Data from adults
The invitation for this review concerned the question “how often is CAKUT diagnosed in young adults?” I was not aware of any detailed age-related data on PRD in young adults and, in fact, have not been able to find anything published.
In 1976 the annual EDTA report gave details of 41,132 adult patients on the Registry [31]. They observed that in the past 10 years the mean age of patients entering the registry had increased from 36 years to 40 years. Given that only 1.6% had diabetes, I will summarise the other relevant data. Of the 40,881 patients who had a PRD reported, 22% had CAKUT, 10% CONGEN, and 49% were reported as having ‘glomerulonephritis’, of whom 81% had no biopsy, and a further 7% showed only end-stage changes. The total left, therefore, with some characterised form of glomerulonephritis, amounted to only 5.6% of those on the registry. In addition, a further 6% had “other (but not specified) disease”. Thus, for 49% of patients on the registry, their PRD was uncharacterised.
Have things improved? Up to a point.
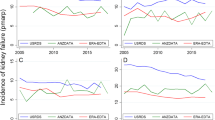
For the age groups 20–29 years, both the UK and USRDS registries still report “unknown” rates of 20% and 26%, respectively, which rise to 28% and 36% when all unspecified groups, predominantly “Glomerulonephritis (GN) (histologically not examined)”, are considered together (see Table 2).
For CAKUT, the UK rate drops, from the BAPN data level of 45% for ages 12–15 years [27], to 26% for the 18–21 year age group and to 20% for those aged 18–29 years, while for USRDS the rate is only 4.6% for those aged 20–29 years and the CONGEN rate is only 3% compared with 9% for UK all under 30 years. This compares with the paediatric North American data (NAPRTCS), which includes all those with chronic renal insufficiency (<75 ml/min) below the age of 21 years, for which CAKUT is 51%, CONGEN 9.8%, unknown 3.8%, and “other unspecified” 15% (Table 2).
The USRDS data has 36% “unknown/unspecified” diseases (which includes 10% that were reported as “glomerulonephritis: histologically not examined, code 4”), and there are a further 2% with “Other renal disorders (unspecified) - code 68” that should perhaps be included.
Clinical nephrology (a refresher course)
As adult registry data still often resemble EDTA data from 1976, it is important to rehearse some diagnostic criteria.
Clinical syndromes
Glomerulonephritis can present in various ways but not as asymptomatic end-stage renal failure.
All forms of glomerulonephritis (except possibly Alport’s syndrome, which, in this discussion, comes under the heading of “Other congenital and familial disease”) will present with macroscopic haematuria, nephritic syndrome, nephrotic syndrome, fluid retention, or malignant hypertension, and some will be diagnosed via routine investigations—but not at the end stage.
Nephrotic syndrome is something very specific. It should not be confused with nephrotic-range proteinuria (>3 g/day or 300 mg/mmol) occurring in a patient with normal levels of plasma albumin and no peripheral oedema.
FSGS. Primary FSGS is a cause of nephrotic syndrome, commonly leading to renal failure in children and sometimes adults (EDTA codes 11, 17). EDTA has no code for secondary FSGS. USRDS has only a catch-all “Focal glomerulosclerosis, focal sclerosing” code 5 (with no clinical conditions attached).
Many patients with slowly progressive renal disease such as reflux nephropathy/renal dysplasia, develop a secondary FSGS. This is commonly associated with heavy proteinuria (nephrotic-range) but normal plasma albumin levels.
Furthermore:
A young man with ESRF and 2+ proteinuria does not necessarily have primary glomerulonephritis.
A young man with ESRF and 2+ proteinuria, 1+ haematuria does not necessarily have immunoglobulin A (IgA) glomerulonephritis.
Hypertension in young white patients does not cause renal failure. The underlying renal disease can lead to malignant or accelerated hypertension, which can certainly result in rapid loss of remaining function.
Young patients who do reach end-stage renal failure with minimal symptoms, minimal proteinuria, and no peripheral oedema and without malignant hypertension have to have some form of tubular disease.
Imaging
Imaging patients with advanced renal failure was virtually impossible until the advent of routine ultrasound, and that was relatively recently (circa 1980). It is difficult to obtain accurate information on the shape of small contracted kidneys. Computed tomography and magnetic resonance imaging should give useful information, but there is very little published on renal imaging in uraemia, with the exception of analgesic nephropathy [32, 33].
Biopsy interpretation
One good reason for the nephrologist not to obtain a biopsy at end-stage renal failure is that the sample is unlikely to show enough viable tissue for a specific diagnosis to be made. The majority of glomeruli will show global sclerosis. The only EDTA code for this would be “Glomerulonephritis; histologically examined, not given above, code 19 ”.
Summary
While paediatricians have progressively reduced their numbers of undiagnosed patients to 5% or fewer, nephrologists treating adults still report much higher levels. There may be several reasons for this, but it is likely that many are patients who present at end stage and for whom a definitive clinical or histological diagnosis is not possible. It is also likely that such nephrologists are often unfamiliar with the more esoteric congenital conditions, particularly tubular diseases, and are unaware of the possibility that renal dysplasia/reflux might present at this age.
Some assumptions that I have made may tend to overestimate the “Unknowns” by adding in all patients described as “Other diagnoses” (but un-specified). Nevertheless, I believe these estimates will give us a much truer picture of the extent of our knowledge.
Different diseases have different rates of progression. But, generally, the CAKUT groups decline relatively slowly, at 2–3 ml/min per year [30, 34, 35], suggesting that patients with less severe CAKUT will not reach end stage until adulthood. Renal function with glomerulonephritis declines more quickly, but the ItalKid study reported only 9.4% with glomerulonephritis (primary and secondary) in their chronic renal insufficiency group (<75 ml/min per 1.73 m2) [8], suggesting that adult services were not about to be deluged with end-stage glomerulonephritis.
It needs to be part of our culture to make a diagnosis in all cases of renal failure, even if this highlights our inability to diagnose certain patients, which, in turn, should lead to novel research initiatives.
The data that I have presented support the view that many cases of congenital diseases are probably not recognised, or are mis-diagnosed as glomerulonephritis. Certainly, the experience of paediatric nephrologists over the past 30 years supports this hypothesis.
Does this matter?
Yes it does.
-
Dialysis may be a big business these days, but we still have a primary responsibility to our patients to find out what is wrong with them, prevent it recurring, and counsel them about possible inherited risk.
-
Treatment designed to slow progression might be difficult to interpret if we do not know the underlying disease. [Do angiotensin-converting enzyme (ACE) inhibitors slow progression in Alport’s disease?] The outcome of CAKUT in young adults is reported in a second review [36].
-
Research is ultimately directed at the problems and questions that we face. When grants begin ‘the commonest cause of end-stage renal failure is glomerulonephritis, ..” Is this correct?
-
Academic meetings and symposia aim to tackle the leading questions and problems. How often do the clinical issues of CAKUT come up in your national society of nephrology?
Abbreviations
- BAPN:
-
British Association for Paediatric Nephrology
- CAKUT:
-
Congenital abnormalities of the kidney and urinary tract
- CONGEN:
-
Other familial and congenital conditions (excluding CAKUT)
- EDTA:
-
European Dialysis and Transplant Association
- ESRF:
-
End-stage renal failure
- ItalKid:
-
Italian Paediatric Study of Renal Failure
- NAPRTCS:
-
North American Pediatric Renal Transplant Cooperative Study
- PRD:
-
Primary renal disease
- USRDS:
-
US Renal data system
References
NAPRTCS (2007) North American Pediatric Renal Trials and Collaborative Studies. Available at https://doi.org/web.emmes.com/study/ped/annlrept/annlrept2007.pdf
Zurowska A, Zagozdzon I, Balasz I, Boguszewska A, Prokurat C, Pietrzyk J, Drozdz D, Szczepanska M, Stefaniak E, Jander A, Roszkowska-Blaim D, Ziolkowska H, Makulska I, Kollataj B, Jarmolinski T, Siten G, Stankiewicz R, Wiercinski R (2006) Congenital and genetic related causes of end-stage renal disease—data from Polish Registry of Renal Replacement Therapy in Children 2000–2004. Przegl Lek 63 [Suppl 3]:57–59
British Association for Paediatric Nephrology (2005) Report from the paediatric renal registry. In: Ansell D, Feest TG, Byrne C (eds) The UK Renal Registry 8th Annual Report; pp 269–291
Al Eisa A, Naseef M, Al Hamad N, Pinto R, Al Shimeri N, Tahmaz M (2005) Chronic renal failure in Kuwaiti children: an eight-year experience. Pediatr Nephrol 20:1781–1785
Miklovicova D, Cornelissen M, Cransberg K, Groothoff JW, Dedik L, Schroder CH (2005) Etiology and epidemiology of end-stage renal disease in Dutch children 1987–2001. Pediatr Nephrol 20:1136–1142
Rahman MH, Karim MA, Hoque E, Hossain MM (2005) Chronic renal failure in children. Mymensingh Med J 14:156–159
Yang JY, Yao Y (2004) Analysis of 1268 patients with chronic renal failure in childhood: a report from 91 hospitals in China from 1990 to 2002. Zhonghua Er Ke Za Zhi 42:724–730
Ardissino G, Dacco V, Testa S, Bonaudo R, Claris-Appiani A, Taioli E, Marra G, Edefonti A, Sereni F (2003) Epidemiology of chronic renal failure in children: data from the ItalKid project. Pediatrics 111:e382–e387
Peco-Antic A, Bogdanovic R, Godubovic E, Djapic M (2003) Chronic renal failure in children in Yugoslavia. Srp Arh Celok Lek 131:5–9
Hari P, Singla IK, Mantan M, Kanitkar M, Batra B, Bagga A (2003) Chronic renal failure in children. Indian Pediatr 40:1035–1042
Anochie I, Eke F (2003) Chronic renal failure in children: a report from Port Harcourt, Nigeria (1985–2000). Pediatr Nephrol 18:692–695
Jamro S, Channa NA, Shaikh AH, Ramzan A (2003) Chronic renal failure in children. J Pak Med Assoc 53:140–142
Hattori S, Yosioka K, Honda M, Ito H (2002) The 1998 report of the Japanese National Registry data on pediatric end-stage renal disease patients. Pediatr Nephrol 17:456–461
Hamed RM (2002) The spectrum of chronic renal failure among Jordanian children. J Nephrol 15:130–135
Miller ME, Williams JA (2002) Chronic renal failure in Jamaican children. West Indian Med J 51:220–224
Madani K, Otoukesh H, Rastegar A, Van Why S (2001) Chronic renal failure in Iranian children. Pediatr Nephrol 16:140–144
Lagomarsimo E, Valenzuela A, Cavagnaro F, Solar E (1999) Chronic renal failure in pediatrics 1996. Chilean survey. Pediatr Nephrol 13:288–291
Fivush BA, Jabs K, Neu AM, Sullivan EK, Feld L, Kohaut E, Fine R (1998) Chronic renal insufficiency in children and adolescents: the 1996 annual report of NAPRTCS. North American Pediatric Renal Transplant Cooperative Study. Pediatr Nephrol 12:328–337
Esbjorner E, Berg U, Hansson S (1997) Epidemiology of chronic renal failure in children: a report from Sweden 1986–1994. Swedish Pediatric Nephrology Association. Pediatr Nephrol 11:438–442
Sirin A, Emre S, Alpay H, Nayir A, Bilge I, Tanman F (1995) Etiology of chronic renal failure in Turkish children. Pediatr Nephrol 9:549–552
Deleau J, Andre JL, Briancon S, Musse JP (1994) Chronic renal failure in children: an epidemiological survey in Lorraine (France) 1975–1990. Pediatr Nephrol 8:472–476
Mattoo TK, Al-Mohalhal S, Al-Sowailem A, Mahmood MA (1990) Chronic renal failure in children in Saudi Arabia. Ann Saudi Med 10:496–499
Pistor K, Olbing H, Scharer K (1985) Children with chronic renal failure in the Federal Republic of Germany: I. Epidemiology, modes of treatment, survival. Arbeitsgemeinschaft fur Padiatrische Nephrologie. Clin Nephrol 23:272–277
Potter DE, Holliday MA, Piel CF, Feduska NJ, Belzer FO, Salvatierra O Jr (1980) Treatment of end-stage renal disease in children: a 15-year experience. Kidney Int 18:103–109
van der Heijden BJ, van Dijk PC, Verrier-Jones K, Jager KJ, Briggs JD (2004) Renal replacement therapy in children: data from 12 registries in Europe. Pediatr Nephrol 19:213–221
USRDS Annual Data Report (1999) Chap VIII. Pediatric end-stage renal disease. Available at https://doi.org/www.usrds.org/chapters/ch08.pdf
Lewis M, Shaw J, Reid C, Evans J, Webb N, Verrier-Jones K (2007) Demography and management of childhood established renal failure in the UK (chapter 13). Nephrol Dial Transplant 22 [Suppl 7]:165–175
Lewis MA (2008) Demography of renal disease in childhood. Semin Fetal Neonatal Med 13:118–124
Schärer K, Chantler C, Brunner FP, Gurland HJ, Jacobs C, Selwood NH, Spies G, Wing AJ (1976) Combined report on regular dialysis and transplantation of children in Europe, 1975. Proc Eur Dial Transplant Assoc 13:59–105
Neild GH, Thomson G, Nitsch D, Woolfson RG, Connolly JO, Woodhouse CR (2004) Renal outcome in adults with renal insufficiency and irregular asymmetric kidneys. BMC Nephrol 5:12
Gurland HJ, Brunner FP, Chantler C, Jacobs C, Scharer K, Selwood NH, Spies G, Wing AJ (1976) Combined report on regular dialysis and transplantation in Europe, 1975. Proc Eur Dial Transplant Assoc 13:1–58
Henrich WL, Clark RL, Kelly JP, Buckalew VM, Fenves A, Finn WF, Shapiro JI, Kimmel PL, Eggers P, Agodoa LE, Porter GA, Shapiro S, Toto R, Anderson T, Cupples LA, Kaufman DW (2006) Non-contrast-enhanced computerized tomography and analgesic-related kidney disease: report of the national analgesic nephropathy study. J Am Soc Nephrol 17:1472–1480
Elseviers MM, Waller I, Nenoy D, Levora J, Matousovic K, Tanquerel T, Pommer W, Schwarz A, Keller E, Thieler H (1995) Evaluation of diagnostic criteria for analgesic nephropathy in patients with end-stage renal failure: results of the ANNE study. Analgesic Nephropathy Network of Europe. Nephrol Dial Transplant 10:808–814
Gonzalez Celedon C, Bitsori M, Tullus K (2007) Progression of chronic renal failure in children with dysplastic kidneys. Pediatr Nephrol 22:1014–1020
Wingen AM, Fabian-Bach C, Schaefer F, Mehls O (1997) Randomised multicentre study of a low-protein diet on the progression of chronic renal failure in children. European Study Group of Nutritional Treatment of Chronic Renal Failure in Childhood. Lancet 349:1117–1123
Neild GH (2009) What do we know about chronic renal failure in young adults? II. Adult outcome of pediatric renal disease. Pediatr Nephrol doi: s00467-008-1107-4
Acknowledgements
I am very grateful for the immediate help I received from the Registries I contacted and, in particular, Dr. David Ansell, at the UK Renal Registry, and Beth Forrest, at the USRDS.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at https://doi.org/dx.doi.org/10.1007/s00467-009-1177-y
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Tables
(DOC 65.5 KB)
Rights and permissions
About this article
Cite this article
Neild, G.H. What do we know about chronic renal failure in young adults? I. Primary renal disease. Pediatr Nephrol 24, 1913–1919 (2009). https://doi.org/10.1007/s00467-008-1108-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-008-1108-3