Abstract
Background
There are a variety of strategies for the treatment of patients with cholecysto-choledocholithiasis (CCL). Although the surgical approach of choice is preoperative ERCP and laparoscopic cholecystectomy (ERCP + LC), controversy remains regarding which procedure is optimal for CCL.
Methods
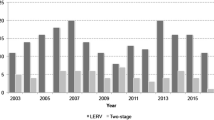
To evaluate the safety and effectiveness of laparoendoscopic rendezvous (LERV) versus ERCP + LC for CCL, a total of 528 patients with CCL were retrospectively studied from January 2013 to December 2018. The patients were scheduled to undergo either the LERV or ERCP + LC procedure. The LERV group included 123 cases, whereas the ERCP + LC group contained 137 cases. The incidence of postoperative complications, success of stone clearance, length of hospital stay, and hospitalization charges were statistically analyzed.
Results
The incidence of pancreatitis was lower in the LERV group than in the ERCP + LC group (3/123 vs. 12/137, P = 0.0291). The median level of post-ERCP amylase was much lower in the LERV group (202.5 U/dL vs. 328.1 U/dL, P < 0.01). However, there was no significant difference in the stone clearance rate or other early complications between the two groups. Further study showed that the length of hospital stay and cost in the LERV group were less than those in the ERCP + LC group (12 days vs. 18 days, P < 0.01; 53591.4¥ vs. 60089.2¥, P < 0.01). In addition, more patients in the two-stage procedure group experienced later biliary complications compared with those in the one-stage approach group (34/137 vs. 4/123, P < 0.05). However, the median operation time was 107.7 min in the two-stage group and 139.8 min in the one-stage group (P < 0.05).
Conclusions
The LERV technique is a safe and effective approach for CCL with lower pancreatitis; it was associated with few later biliary complications, shortened hospital stays, and fewer charges but significantly longer operative time.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Cholecysto-choledocholithiasis refers to the simultaneous presence of stones in the gallbladder and the common bile duct (CBD). The prevalence of concomitant choledocholithiasis in patients with symptomatic gallstone disease varies from approximately 10 to 18% [1]. While laparoscopic cholecystectomy (LC) is considered the “gold standard” for the treatment of cholecystolithiasis, the preferred therapy for cholecysto-choledocholithiasis is still controversial.
In the past, open CBD exploration combined with cholecystectomy was a conventional method for treating patients with cholecysto-choledocholithiasis. Along with the improvement of laparoscopic and endoscopic techniques, the surgical management of concomitant gallstones with CBD stones encompasses a variety of strategies, including simultaneous or sequential approaches [2]. Currently, the most commonly applied procedure is preoperative endoscopic retrograde cholangiopancreatography (ERCP) and endoscopic sphincterotomy (EST) and stone extraction followed by LC, the so-called sequential two-stage intervention, which was also recommended by the 2016 EASL (the European Association for the Study of the Liver) clinical practice guidelines for the prevention, diagnosis, and treatment of gallstones [3]. Nevertheless, accumulated evidence suggests that ERCP/EST may lead to unpredictable severe complications, such as post-ERCP pancreatitis (PEP), perforation, and hemorrhage [4, 5]. It is reported that ERCP/EST is associated with a failure to cannulate the ampulla of Vater, with a rate ranging from 4 to 18% [6]. Meanwhile, PEP is a major concern that can result from prolonged and repeated pancreatic duct cannulation and inadvertent contrast injection.
Considering the above disadvantages of ERCP/EST, a fascinating alternative approach could be the laparoendoscopic rendezvous technique (LERV), the so-called simultaneous one-stage intervention, which was first described by Deslandres in 1993 and completed by Feretis in 1994 [7]. LERV involves a combined laparoendoscopic procedure in which cholecystectomy is performed laparoscopically while choledocholithiasis is cleared endoscopically via the simultaneous application of biliary cannulation over the papilla of Vater. In the rendezvous cannulation, the guide wire goes through the cystic duct into the duodenum under laparoscopy. This method might theoretically achieve immediate bile duct cannulation and prevent inadvertent pancreatic cannulation [8]. Moreover, it does not require additional equipment apart from what is usually employed in ERCP/EST and LC procedures.
Previously, limited data have indicated that LERV is associated with a lower incidence of PEP than preoperative ERCP/EST and LC [9]. However, whether the combination of rendezvous cannulation with the ERCP strategy has better or worse results than the preoperative ERCP/EST approach for choledocholithiasis complicated with cholecystolithiasis remains controversial. A number of studies have suggested that both methods are equivalent in terms of efficacy, morbidity, and mortality [10,11,12]. Therefore, we performed a retrospective cohort analysis to determine the effectiveness and safety of the simultaneous intervention (LERV) versus sequential management (pre-ERCP/EST + LC) in patients with cholecysto-choledocholithiasis.
Materials and methods
Patients and selection
From January 2013 to December 2018, 528 consecutive patients with concomitant cholecysto-choledocholithiasis (CCL) were enrolled in the Department of Hepato-Biliary Pancreatic Surgery, Zhongnan Hospital of Wuhan University, P. R. China. We retrospectively analyzed the medical records of 260 patients with CCL who were scheduled for either a single-stage or two-stage procedure. A total of 123 of these patients were treated with the one-stage procedure, and 137 patients were managed with the two-stage procedure. The flow chart of patients is presented in Fig. 1. Ethical approval for this study was granted by the Medical Ethics Committee of the Zhongnan Hospital of Wuhan University, and informed consent from the retrospective patient cohort was waived. The exclusion criteria of this study included the following: (i) previous biliary tract surgical history, (ii) American Society of Anesthesiologists (ASA) score ≥ 4, (iii) suppurative cholangitis, (iv) acute pancreatitis, (v) decompensated cirrhosis, and (vi) pregnancy. All patients received reasonable treatment before surgery. A preoperative diagnosis of CCL was routinely determined based on clinical presentation, abdominal ultrasonography, and magnetic resonance cholangiopancreatography (MRCP).
Surgical and endoscopic techniques
The techniques of the two-stage procedure (ERCP/EST followed by LC) have been described in previous studies [13, 14]. All ERCP/EST procedures were performed by experienced endoscopic physicians, and all LC procedures were performed by skilled laparoscopic surgeons. Before proceeding to LC, a waiting period was mandatory. The median interval period was 3 days in this study.
Currently, there are many described techniques for performing LERV. Miscusi G et al. presented a procedure with traditional LERV [15]. During LC, a catheter was introduced into the cystic duct, and then intraoperative cholangiography was performed. Subsequently, ERCP/EST was performed by an endoscopist. Finally, LC was completed after the stones were completely removed. An LERV approach with technical adjustments may be more commonly performed due to its simplicity. In our study, a slightly modified LERV technique was applied. A guide wire was inserted into the cystic duct and out through the duodenal papilla. The guide wire was further endoscopically gripped with a polypectomy loop or a snare and retrieved through the mouth. Sequently a water balloon catheter dilator was inserted over the wire and selective CBD cannulation was performed followed by intraoperative ERCP and clearance of CBD stones. It should be noted that all LERV procedures were performed by the authors in the absence of endoscopic physicians.
Outcome measures
The primary outcome measure was the incidence of early surgical complications, including bile leakage, postoperative bleeding, perforation, and post-ERCP pancreatitis. The secondary outcome measures were the success of the stone clearance, operation time, length of hospital stay, cost, and rate of later biliary complications.
Statistical analysis
All statistical analyses were performed using the SPSS software package (version 19.0, SPSS Inc., Chicago IL, United States). Quantitative data are presented as the mean ± SD. Statistical comparisons between the two groups were analyzed by Student’s t test, ANOVA, Mann–Whitney U test, or the Chi-square test, when appropriate. A P value < 0.05 was considered statistically significant.
Results
Demographic characteristics of patients with CCL
In this study, a total of 260 patients with CCL (128 females and 132 males) were included and retrospectively analyzed. Among them, 137 patients were treated with the two-stage procedure (ERCP + LC), and 123 patients underwent one-stage management (LERV). The ERCP + LC group consisted of 73 females and 64 males with a median age of 58.2 years, whereas the LERV group was composed of 55 females and 68 males with a median age of 56.3 years. The relevant preoperative characteristics of CCL patients are shown in Table 1. There were no significant differences between the two groups in terms of sample size, gender, median age, BMI, ASA score, clinical presentation, mean diameter of CBD stones, serum levels of total bilirubin, and alkaline phosphatase (P > 0.05 for each).
Clinical outcomes for one-stage and two-stage management
The intraoperative and postoperative parameters of the patients with CCL who underwent different management were measured and are depicted in Table 2. There was no death of patients in our study. We found no difference in the rate of stone clearance between the LERV approach and the conventional one-stage procedure group (97.5% vs. 96.3%, P > 0.05). The overall operation time, including the preoperative time of ERCP/EST and LC, was 107.7 ± 40.6 min in the two-stage group and 139.8 ± 46.8 min in the one-stage group. This difference may exist because with the LERV technique it is difficult to perform selective cannulation during LC. Moreover, the mean duration of endoscopic part of the procedure did differ between the two groups (one-stage: 60.5 ± 16.2 min; two-stage: 41.4 ± 20.7 min, P < 0.01).
The incidence of complications in the two groups was further investigated. The incidence of PEP in the single-stage group was 2.4% (3/123); in the two-stage group, it was 8.8% (12/137); and there was a significant difference between the two groups (P < 0.05). Consistent with the PEP rate, the level of serum amylasemia was lower post-LERV than post-ERCP. The incidences of bile leakage, bleeding, and perforation did not differ significantly between the two groups. All patients with early complications were managed successfully with timely treatment. Nevertheless, the occurrence rates of later biliary complications, including cholangitis (2.2% vs. 0%, P < 0.05), recurrence of CBD stones (16.8% vs. 3.3%, P < 0.01), and papillary stenosis (4.4% vs. 0%, P < 0.01) in the two-stage group were higher than in the one-stage group. The later biliary complication incidence in the two-stage management group was in accordance with previous publications concerned with ERCP/EST.
The patients’ duration of hospital stay and economic expenses were important clinical outcomes. The median hospital stay of the one-stage group was significantly shorter than that of the two-stage group (12 days vs. 18 days, P < 0.01). Meanwhile, the total cost in the one-stage group was 53591.4 ± 11361.2 RMB and 60089.2 ± 11311.3 RMB. There was a significant difference between the two groups (P < 0.01). Several factors may have contributed to the prolonged length of hospital stay and increased cost. In the present series, the median interval from ERCP/EST to LC was 3 days, and this seems to be the main reason for the differences in hospital stay and total cost.
All patients were followed up for a median of 9 months (2–30 months). Laboratory tests, ultrasonography, and MRCP were employed for postoperative review. Patients with residual or recurrent stones were treated successfully with repeat ERCP.
Discussion
The treatment of concomitant choledocholithiasis in patients with gallstones aims to remove the stones thoroughly. However, there is still no consensus regarding which strategy is optimal for cholecysto-choledocholithiasis. Although the risk of complications, including acute pancreatitis, hemobilia, and cholangitis, has been reported in many studies, preoperative ERCP/EST followed by LC, the so-called two-stage approach, remains the most frequently applied approach worldwide [16, 17]. In recent years, improvements in laparoscopic surgery techniques have made it possible to manage cholecysto-choledocholithiasis with traditional one-stage procedures, including laparoscopic CBD exploration (LCBDE) and laparoscopic trans-cystic bile duct exploration (LTCBDE) [18]. The traditional one-stage approach is associated with fewer procedures, shorter hospital stays, and lower costs compared to the one-stage strategy [19]. Furthermore, accumulating evidence has suggested that there are no significant differences in outcomes between these two procedures [20, 21].
Laparoendoscopic rendezvous (LERV), a novel and feasible one-stage technique, is a combined laparoscopic and endoscopic approach for removing stones in the gallbladder and common bile duct [22]. It is regarded as safe, effective, and economical in theory. The procedure facilitates the identification and cannulation of the papilla because a guide wire is inserted through the cystic duct, which allows the catheter to be grasped and avoids cannulation of the pancreas and the creation of a false passage. In the past, most patients with CCL were firstly treated by ERCP in department of Gastroenterology in our hospital. Subsequently, the patients were transferred to our department of Hepato-Biliary Pancreatic Surgery for performing LC. In recent years, the LERV was found by many experts to be safety, effective, and less expensive single-session management. Moreover, with the progress of our endoscopy skills, we switched to perform LERV by ourselves. In this study, we showed equivalent feasibility (one-stage, 97.5%; two-stage, 96.3%) between the two management options. These results were in accordance with previous published literature [23, 24]. Furthermore, we compared the complications and outcomes between the sequential two-step procedure and single-stage management. As our findings show, the incidence rate of post-ERCP pancreatitis was 2.4% in the LERV group and 8.8% in the ERCP/EST + LC group. Moreover, the average level of serum amylase in the one-stage procedure was significantly lower than that in the two-stage approach. Several studies have indicated that post-ERCP pancreatitis ranges between 1 and 14% [25, 26]. Currently, the pathogenic factors related to post-ERCP pancreatitis are considered to be associated with inadvertent cannulation, contrast injection into the pancreatic duct, and multiple attempts to cannulate the ampulla of Vater [27]. The LERV technique may avoid these complications to a large extent, especially in cases of anatomically difficult endoscopic intubation. Thus, we concluded that the one-stage approach can reduce the incidence of post-ERCP pancreatitis for patients with cholecysto-choledocholithiasis.
In addition, the overall complication occurrence rate was not significantly different between groups, and no patient died in either group, similar to previous publications. These results suggest that the LERV technique provides the same safety and efficacy as ERCP/EST followed by LC for the treatment of cholecysto-choledocholithiasis. Interestingly, late recurrent biliary complications were found in only four cases in the one-stage procedure group but in 34 cases in the two-stage approach group. The rate of recurrent biliary problems such as stenosis of the ampulla in the management of traditional ERCP + LC procedures is reported to range from 11 to 24% [28]. The lower incidence of later biliary complications was attributable to the LERV technique, which decreased the risk of the destruction of the sphincter of Oddi. Further research found that the median hospital stay and cost were both much lower in the group that underwent the one-stage approach. Longer hospital stays obviously contributed to the high cost of the group that underwent the two-stage approach. However, the surgical time was significantly longer for the one-stage procedure. The interval between ERCP and LC seems extended hospitalization time and increased costs. Recent studies have shown that it is extremely difficult to reduce this time interval [29, 30]. Twenty-four hours is the minimal waiting period to ensure that no post-ERCP complications have occurred before proceeding to LC, and this is an obvious disadvantage of two-stage management.
Although the LERV technique has many benefits, its application is still limited in many medical centers. This is largely because it is difficult to ensure the presence of an experienced endoscopist and a skilled laparoscopic surgeon [31, 32]. Close cooperation between the surgeon and the endoscopist is essential for this approach. However, the performance of LERV by surgeons alone without an endoscopic team has been reported [33]. In this article, 123 patients with cholecysto-choledocholithiasis who underwent LERV were treated by the authors. The median operation time was much lower in our series than that indicated in other studies following the LERV technique, which took minutes [34, 35]. This is likely because we did not have to wait for the endoscopist during the operation.
Recently, a few studies have demonstrated that the traditional LERV technique is an optimal approach for patients with cholecysto-choledocholithiasis [36, 37]. Nevertheless, the applied strategy has presented some technical problems [38, 39]: (a) the supine position is inconvenient for performing ERCP; (b) the guide wire is difficult to manipulate when passing across the Oddi sphincter under certain conditions, such as in cases of impacted stones, an excessive diameter of stones, or cystic duct stenosis; (c) the pushing and pulling of the guide wire out of the endoscope for papillary cannulation increases the operation time; (d) the intraoperative endoscopic insufflation can cause bowel distention, which reduces the operating space for LC and causes difficulty with cannulation. Hence, several technical solutions have been presented to ease these difficulties, including changing to the left lateral position and using a bowel desufflator or an atraumatic laparoscopic clamp to avoid bowel distention [40]. Additionally, some aspects of the LERV technique were modified during our study. We first changed the patient’s position from supine to left lateral. In the left lateral position, it was easy to grasp the guide wire and cannulate the ampulla of Vater when the endoscope passes into the descending duodenum. Subsequently, to prevent problems arising from bowel loop distention induced by endoscopic insufflations, Calot’s triangle was completely dissected before ERCP. These experiences improved the success rate of the LERV procedure in patients with cholecysto-choledocholithiasis.
In conclusion, our data further confirmed that one-stage management is a safe and effective approach for patients with cholecysto-choledocholithiasis. In comparison with conventional two-stage procedures, it could lead to a shorter median hospital stay, lower costs, a lower incidence of pancreatitis, and fewer late biliary complications. However, a limitation of the current research was the fact that it was a single-center retrospective study with small sample sizes. Selection bias may have been introduced by the retrospective nature of the study. Further prospective investigations should be conducted to determine the best treatment option for cholecysto-choledocholithiasis.
References
Dasari BV, Tan CJ, Gurusamy KS, Bobby VMD, Chuan JT, Kurinchi SG, David JM, Gareth K, Lloyd MK, Tom D, Mark AT (2013) Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev 8:CD003327
Prasson P, Bai X, Zhang Q, Liang T (2016) One-stage laproendoscopic procedure versus two-stage procedure in the management for gallstone disease and biliary duct calculi: a systemic review and meta-analysis. Surg Endosc 30:3582–3590
European Association for the Study of the Liver (EASL) (2016) EASL clinical practice guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol 65:146–181
Mine T, Morizane T, Kawaguchi Y, Akashi R, Hanada K, Ito T, Kanno A, Kida M, Miyagawa H, Yamaguchi T, Mayumi T, Takeyama Y, Shimosegawa T (2017) Clinical practice guideline for post-ERCP pancreatitis. J Gastroenterol 52:1013–1022
Nalankilli K, Kannuthurai S, Moss A (2016) A modern approach to ERCP: maintaining efficacy while optimising safety. Dig Endosc 28(Suppl 1):70–76
Enochsson L, Lindberg B, Swahn F, Arnelo U (2004) Intraoperative endoscopic retrograde cholangiopancreatography (ERCP) to remove common bile duct stones during routine laparoscopic cholecystectomy does not prolong hospitalization: a 2-year experience. Surg Endosc 18:367–371
Feretis C, Kalliakmanis B, Benakis P, Apostolids N (1994) Laparoscopic transcystic papillotomy under endoscopic control for bile duct stones. Endoscopy 26:697–700
Rábago LR, Vicente C, Soler F, Delgado M, Moral I, Guerra I, Castro JL, Quintanilla E, Romeo J, Llorente R, Vázquez Echarri J, Martínez-Veiga JL, Gea F (2006) Two-stage treatment with preoperative endoscopic retrograde cholangiopancreatography (ERCP) compared with single-stage treatment with intraoperative ERCP for patients with symptomatic cholelithiasis with possible choledocholithiasis. Endoscopy 38:779–786
Liverani A, Muroni M, Santi F, Neri T, Anastasio G, Moretti M, Favi F, Solinas L (2013) One-step laparoscopic and endoscopic treatment of gallbladder and common bile duct stones: our experience of the last 9 years in a retrospective study. Am Surg 79:1243–1247
Ricci C, Pagano N, Taffurelli G, Pacilio CA, Migliori M, Bazzoli F, Casadei R, Minni F (2018) Comparison of efficacy and safety of 4 combinations of laparoscopic and intraoperative techniques for management of gallstone disease with biliary duct calculi: a systematic review and network meta-analysis. JAMA Surg 1539:e181167
Vettoretto N, Arezzo A, Famiglietti F, Cirocchi R, Moja L, Morino M (2018) Laparoscopic-endoscopic rendezvous versus preoperative endoscopic sphincterotomy in people undergoing laparoscopic cholecystectomy for stones in the gallbladder and bile duct. Cochrane Database Syst Rev 4:CD010507
La BG, Gardini A, Cavargini E, Casadei A, Morgagni P, Bazzocchi F, D’Acapito F, Cavaliere D, Curti R, Tringali D, Cucchetti A, Ercolani G (2018) Laparoendoscopic rendezvous in the treatment of cholecysto-choledocholitiasis: a single series of 200 patients. Surg Endosc 32:3868–3873
Staritz M, Ewe K, Meyer BKH (1982) Endoscopic papillary dilatation, a possible alternative to endoscopic papillotomy. Lancet 1:1306–1307
Ding J, Li F, Zhu HY, Zhang XW (2015) Endoscopic treatment of difficult extrahepatic bile duct stones, EPBD or EST: an anatomic view. World J Gastrointest Endosc 7:274–277
Miscusi G, Gasparrini M, Petruzziello L, Taglienti D, Onorato M, Otti M, Montori J (1997) Endolaparoscopic ‘‘Rendez-vous’’ in the treatment of cholecystocholedochal calculosis. G Chir 18:655–657
Tzovaras G, Baloyiannis I, Zachari E, Symeonidis D, Zacharoulis D, Kapsoritakis A, Paroutoglou G, Potamianos S (2012) Laparoendoscopic rendezvous versus preoperative ERCP and laparoscopic cholecystectomy for the management of cholecysto-choledocholithiasis: interim analysis of a controlled randomized trial. Ann Surg 255:435–439
Gaetano LG, Francesco B, Maria S, Saverio L (2010) Simultaneous laparoendoscopic rendezvous for the treatment of cholecystocholedocholithiasis. Surg Endosc 24:769–780
Feng Q, Huang Y, Wang K, Yuan R, Xiong X, Wu L (2016) Laparoscopic transcystic common bile duct exploration: advantages over laparoscopic choledochotomy. PLoS ONE 11:e0162885
Gupta N (2016) Role of laparoscopic common bile duct exploration in the management of choledocholithiasis. World J Gastrointest Surg 8:376–381
Lu J, Cheng Y, Xiong XZ, Lin YX, Wu SJ, Cheng NS (2012) Two-stage vs single-stage management for concomitant gallstones and common bile duct stones. World J Gastroenterol 18:3156–3166
Martin DJ, Vernon DR, Toouli J (2006) Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev 2:CD003327
El-Geidie AA (2011) Laparoendoscopic management of concomitant gallbladder stones and common bile duct stones: what is the best technique? Surg Laparosc Endosc Percutan Tech 21:282–287
Cavina E, Franceschi M, Sidoti F, Goletti O, Buccianti P, Chiarugi M (1998) Laparo-endoscopic “rendezvous”: a new technique in the choledocholithiasis treatment. Hepatogastroenterology 45:1430–1435
Basso N, Pizzuto G, Surgo D, Materia A, Silecchia G, Fantini A, Fiocca F, Trentino P (1999) Laparoscopic cholecystectomy and intraoperative endoscopic sphincterotomy in the treatment of cholecysto-choledocholithiasis. Gastrointest Endosc 50:532–535
Pezzilli R, Romboli E, Campana D, Corinaldesi R (2002) Mechanisms involved in the onset of post-ERCP pancreatitis. JOP 3:162–168
Testoni PA (2002) Why the incidence of post-ERCP pancreatitis varies considerably? Factors affecting the diagnosis and the incidence of this complication. JOP 3:195–201
Testoni PA, Mariani A, Giussani A, Vailati C, Masci E, Macarri G, Ghezzo L, Familiari L, Giardullo N, Mutignani M, Lombardi G, Talamini G, Spadaccini A, Briglia R, Piazzi L; SEIFRED Group (2010) Risk factors for post-ERCP pancreatitis in high- and low-volume centers and among expert and non-expert operators: a prospective multicenter study. Am J Gastroenterol 105:1753–1761
Sugiyama M, Atomi Y (2002) Risk factors predictive of late complications after endoscopic sphincterotomy for bile duct stones: long-term (more than 10 years) follow-up study. Am J Gastroenterol 97:2763–2767
Bostanci EB, Ercan M, Ozer I, Teke Z, Parlak E, Akoglu M (2010) Timing of elective laparoscopic cholecystectomy after endoscopic retrograde cholangiopancreaticography with sphincterotomy: a prospective observational study of 308 patients. Langenbecks Arch Surg 395:661–666
Salman B, Yilmaz U, Kerem M, Bedirli A, Sare M, Sakrak O, Tatlicioglu E (2009) The timing of laparoscopic cholecystectomy after endoscopic retrograde cholangiopancreaticography in cholelithiasis coexisting with choledocholithiasis. J Hepatobiliary Pancreat Surg 16:832–836
Bove A, Di Renzo RM, Palone G, Testa D, Malerba V, Bongarzoni G (2018) Single-stage procedure for the treatment of cholecysto-choledocolithiasis: a surgical procedures review. Ther Clin Risk Manag 14:305–312
ElGeidie AA (2014) Single-session minimally invasive management of common bile duct stones. World J Gastroenterol 20:15144–15152
Odabasi M, Yildiz MK, Abuoglu HH, Eris C, Ozkan E, Gunay E, Aktekin A, Muftuoglu MT (2013) A modified Rendezvous ERCP technique in duodenal diverticulum. World J Gastrointest Endosc 5:568–573
Garbarini A, Reggio D, Arolfo S, Bruno M, Passera R, Catalano G, Barletti C, Salizzoni M, Morino M, Petruzzelli L, Arezzo A (2017) Cost analysis of laparoendoscopic rendezvous versus preoperative ERCP and laparoscopic cholecystectomy in the management of cholecystocholedocholithiasis. Surg Endosc 31:3291–3296
La GG, Pesce A, Vitale M, Mannino M, Di MF, Di BM, Lombardo R, Puleo S, Russello D, Latteri S (2017) Efficacy of the laparoendoscopic “rendezvous” to treat cholecystocholedocholithiasis in 210 consecutive patients: a single center experience. Surg Laparosc Endosc Percutan Tech 27:e48–e52
Erickson RA, Carlson B (1995) The role of endoscopic retrograde cholangiopancreatography in patients with laparoscopic cholecystectomies. Gastroenterology 109:252–263
Rogers SJ, Cello JP, Horn JK, Siperstein AE, Schecter WP, Campbell AR, Mackersie RC, Rodas A, Kreuwel HT, Harris HW (2010) Prospective randomized trial of LC + LCBDE vs ERCP/S + LC for common bile duct stone disease. Arch Surg 145:28–33
Lella F, Bagnolo F, Rebuffat C, Scalambra M, Bonassi U, Colombo E (2006) Use of the laparoscopic-endoscopic approach, the so-called “rendezvous” technique, in cholecystocholedocholithiasis: a valid method in cases with patient-related risk factors for post-ERCP pancreatitis. Surg Endosc 20:419–423
Gagner M (2010) Intra-operative sphincterotomy and ERCP for choledocholithiasis during laparoscopic cholecystectomy. Surgery 147:463
Mario M, Filippo B, Claudio M, Niccolò F, Riccardo R, Aldo G (2006) Preoperative endoscopic sphincterotomy versus laparoendoscopic rendezvous in patients with gallbladder and bile duct stones. Ann Surg 244:889–893
Acknowledgements
The authors thank Quanyan Liu, MD, and Dingyu Pan, MD, from the Department of Hepato-Biliary Pancreatic Surgery, Zhongnan Hospital of Wuhan University, for their language and technical help and they also thank Hongling Wang, MD, from the Department of Gastroenterology, Zhongnan Hospital of Wuhan University, for preoperative ERCP.
Funding
This study was supported by grants from the National Natural Science Foundation of China (Grant No. 81802442).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Yawei Qian, Jianglin Xie, Ping Jiang, Yuchun Yin, and Quan Sun have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Qian, Y., Xie, J., Jiang, P. et al. Laparoendoscopic rendezvous versus ERCP followed by laparoscopic cholecystectomy for the management of cholecysto-choledocholithiasis: a retrospectively cohort study. Surg Endosc 34, 2483–2489 (2020). https://doi.org/10.1007/s00464-019-07051-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07051-y