Abstract
Background
An accepted treatment strategy for cholelithiasis with secondary choledocholithiasis is the laparoscopic cholecystectomy (LC) following endoscopic retrograde cholangiopancreaticography (ERCP). Although early cholecystectomy is advised, there is no consensus about the time interval between LC and ERCP. The aim of this study is to evaluate the effects of the time interval between ERCP and ERCP on operation outcomes.
Methods
Patients with cholelithiasis and a risk of choledocholithiasis underwent ERCP. Patients were grouped as those operated on between 24 and 72 h after ERCP (group 1) and those operated on more than 72 h after ERCP (group 2). Patients’ age, gender, body mass index, American Society of Anesthesiologists Physical Status, abdominal ultrasonography findings, white blood cell count, total serum bilirubin, ALP, amylase, ALT, AST, GGT levels, ERCP findings, time interval between ERCP and LC, conversion rate, median postoperative hospital stay, median operation time, intraoperative complication and postoperative complication rates were collected.
Results
There was no significant difference between the demographics of the patients in both groups. The median operation time, median postoperative hospital stay and conversion rate in group 2 were significantly higher than those of group 1. More postoperative complications were seen in group 2.
Conclusion
Early cholecystectomy after ERCP, within 72 h, has better outcomes, probably due to the inflammatory processes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In western countries, 7–33% of all patients with gallstones also have coexisting common bile duct stones (CBDS) [1–4]. In these patients, cholecystectomy alone is not adequate for treating the coexisting CBDS, because of associated severe complications such as pancreatitis and cholangitis. Nearly 55% of patients with CBDS have symptoms and half of them have complications [5]. Recommended treatment strategies for CBDS are cholecystectomy with intraoperative cholangiography, intraoperative endoscopic retrograde cholangiopancreaticography (ERCP), surgical removal of the stones, preoperative ERCP and postoperative ERCP [6–8]. Due to experience and technical availability, preoperative ERCP and laparoscopic cholecystectomy (LC) is most-often preferred [9, 10]. The time interval between ERCP and LC is usually a few days, depending on the surgeon's availability [11]. The time varies from 1 day to 6 weeks in different studies [1, 2, 12]. It is widely accepted to operate early, within a short time following ERCP, but exactly how much time is not mentioned [2, 13]. The term “early” is not clear. It is thought that during ERCP bile duct cannulation, contrast agent infusion, sphincterotomy or other minimally-invasive procedures can trigger inflammation. Possible inflammatory effects of ERCP on LC are not clearly known. We do not know enough about the effects of the time elapsed between ERCP and LC on operation and operation outcomes.
In this study, we aimed to evaluate the effects of time between ERCP and LC on operation and operation outcomes.
Materials and methods
The prospective randomized trial was approved by the Ethics of Human Research Committee of Gazi University Medical School. Patients who had been admitted to our department for cholelithiasis were evaluated for the risk of CBDS. The indications for ERCP were one or more of the following: elevated serum bilirubin level (≥2 × upper limit of normal), elevated alkaline phosphatase (ALP, normal range 25–130 U/L), γ-glutamyl transpeptidase (GGT, normal range ≤65 U/L); dilated common bile duct (≥8 mm) and/or stones in common bile duct at ultrasonographic (US) examination. These findings are accepted as predictors of CBDS and give 90–100% predictive value for CBDS [14]. Patients with findings of cholecystitis, pancreatitis, cholangitis and patients with contrast agent allergies or known inflammatory disease were excluded from the study, as inflammation can interfere with the study. Patients who had an abdominal operation, history of peritonitis or history of ERCP were excluded from the study because of intraabdominal adhesion risks. After these exclusions, the patients underwent an ERCP examination. The inability to cannulate the CBD was considered to be a failed procedure; failed ERCP procedures were excluded from the study. In order to achieve a homogenous group, patients with negative ERCP, which means no CBDS found during ERCP, were also excluded from the study. There were 14 negative ERCPs. After this exclusion, the remaining patients were numbered. Patients with even numbers were assigned to group 1, odd numbers to group 2. Patients underwent ERCP for suspected CBDS prior to LC. Group 1 underwent LC between 24 and 72 h after ERCP; group 2 underwent LC at least 72 h to 7 days after ERCP.
Between 2005 and 2008, ta otal of 79 patients were included in the study, which was performed in Gazi University School of Medicine General Surgery Department. One designated endoscopist carried out the procedure using an Olympus JF-240 electronic sideviewing doudenoscope (Olympus Optical Co., Ltd, Tokyo, Japan). Cannulation and sphincterotomy were performed. The sphincterotome contained a Teflon catheter with a cautery wire exposed for a length of 20–30 mm near the tip. After deep bile duct cannulation, the sphincterotome was retracted until one half to two-thirds of the wire length was exposed outside the papilla. The length of the incision ranged from 0.5 to 1 cm. Then a guide wire was inserted through the cannula by which a balloon catheter was positioned. The stones were extracted by stroking the catheter. Other methods, such as mechanical lithotripsy, shock wave lithotripsy and endoprosthesis, were not used because of possible additive inflammatory effects. Three patients in which biliary stents were placed were not included to the study because their presence would affect inflammation. Radiologic images were taken using a C-arm X-ray device (Philips, BV 300, Philips Medical Systems, Best, The Netherlands). Antibiotic prophylaxis with Cephazolin Sodium was started for all patients undergoing ERCP. After an overnight fast, all patients were sedated with 10 mg i.v. dormicum. Endoscopic sphincterotomy (ES) and stone extraction were carried out in the same session. All operations were performed by the same operation team. Preoperative evaluation included patients’ age, gender, body mass index (BMI), American Society of Anesthesiologists Physical Status (ASA), abdominal ultrasonography findings, white blood cell count, total serum bilirubin, ALP, amylase, ALT, AST and GGT levels. Also ERCP findings, time interval between ERCP and LC, conversion rate, median postoperative hospital stay, median operation time, intraoperative complication, and postoperative complication rates were collected. In this way, the effects of early LC after ERCP could be searched using any of several factors as a primary endpoint, while our ERCP, LC results and criteria for CBDS for could be used as a secondary endpoint.
Statistical analysis
The chi square test and Mann–Whitney U test were used for comparisons of the two groups. A p value <0.05 was regarded as indicating a significant difference.
Results
The groups were found to be similar with respect to age, gender, BMI and ASA grade (Table 1). In evaluating the choledocholithiasis, the predictive results were similar in both groups (Table 2). Median time for LC after ERCP for the patients in group 1 (n = 39) was 29.2 ± 2.32 h after ERCP, median time for LC after ERCP for patients in group 2 (n = 40) was 114.2 ± 5.82 h after ERCP. No complications due to ERCP, such as severe pancreatitis, bleeding or perforation, were seen in either of the groups. Duct stones were extracted after sphincterotomy. A bile duct clearance rate of 100% was achieved. The median ERCP time for stone extraction in groups 1 and 2 were 46.2 ± 9.7 and 48.6 ± 10.2, respectively (p = 0.02).
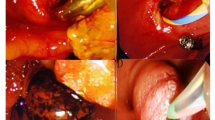
In group 1, LC was attempted in 39 patients, 38 (97.5%) of which were successfully accomplished; only one (2.5%) was converted to open cholecystectomy because of uncertain anatomy of the biliary tree, not changes due to inflammation. In group 2, LC was attempted in 40 patients, of which 33 (82.5%) were successfully accomplished and 7 (17.5%) were converted to open cholecystectomy due to gallbladder bed bleeding (2 patients) or dense adhesions in Callot’s triangle (5 patients). There were statistical differences between the groups with respect to the postoperative hospital stay time and conversion rate (p = 0.02) (Table 3). The median operation time in group 1 was 38.3 ± 7.8 min. In group 2 the median operative time was 68.4 ± 5.96 min (p = 0.03). The median postoperative hospital stay in groups 1 and 2 were 1.96 ± 0.81 and 3.62 ± 2.33 days, respectively (p = 0.03).
Postoperative complications were one pulmonary atelectasis in group 1 and two wound infections and two pulmonary atelectasis in group 2. Wound infections were seen in patients whose operations were converted to open cholecystectomy. All patients were treated and no mortality was seen. There were no intraoperative complications in either of the groups. In the long term follow-up (3 months–3 years) there were no patients with symptoms of retained stones in the common bile duct or delayed complications due to ERCP.
Discussion
Contemporary management of cholelithiasis with secondary choledocholithiasis should include the clearance of CBDS and eliminating the source of gallstones without negating the advantages of LC. Approaches vary with experience and expertise and include laparoscopic CBD exploration, conversion to open CBD exploration and various sequences of LC and ERCP. A number of methods have been used for the diagnosis of CBDS, including ERCP, radiological and laboratory studies. However, some of them are invasive, expensive and require special equipment. The positive predictive value of laboratory data for CBDS was found to be 60–87% in various studies [2, 15]. In our study the five predictive factors for CBD were used. All the patients with CBD has at least one positive value. Elevated serum GGT and ALP levels are more valuable for diagnosis of CBD with values of 79.7 and 68.3%, respectively. The ratios of factors are in accordance with the literature [14]. The mean levels of laboratory results were as high as the levels in the literature, too [16]. Traditional US is less sensitive (20–30%) in detection of ductal stones, but gives important information about dilated bile ducts [2]. Also magnetic resonance cholangiopancreatography (MRCP) and endoscopic US could approach the diagnostic value of ERCP without complications [17]. However, ERCP performed on selected/restricted indications have higher diagnostic and therapeutic advantages [1, 18]. In order to predict CBDS risk, the American Society for Gastrointestinal Endoscopy (ASGE) guidelines mention CBDS risk categories and treatment modalities: in high risk patients, ERCP is the first intervention; in the median risk group endosonography US and MRCP are recommended or, if not available, ERCP is again recommended [19]. Due to financing reasons and availability, the choice depends on local availability and local expertise according to The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) guidelines [20]. The NIH (National Institute of Health) consensus statement, recommends preoperative ERCP or intraoperative transhepatic cholangiography for all patients with clinical suspicion for CBDS. This leads to a high number of therapeutic and nontherapeutic ERCPs [21]. High success rates are mentioned in the literature for ERCP [18–21]. Postoperative ERCP appears to be an excellent option in order to get rid of unnecessary ERCPs, but if ES stone extraction fails or complication occurs (4% complication rate), it leads to a second surgical procedure. Intraoperative ERCP is a single stage procedure, so may be a better choice than the others, but it is a technology-dependent procedure and needs special equipment in the operating room. In our department, because of availability and experience, we perform preoperative ERCP for CBDS. Selective preoperative ERCP and ES are attractive options for the management of CBDS prior to LC.
Although widely accepted, there are some drawbacks to ERCP prior to LC. First is the unnecessary ERCP rate of 38–57% [21]. This rate is can be reduced by risk categories or other interventions. It must be noted that ERCP can also help us in other kinds of diagnoses, sucha s benign papillary stenosis, biliary tract anomalies, cancer, diverticules and so forth. Secondly, failure rate is about 5% [22]. Another criticism of ERCP prior to LC is the long hospital stay when compared with intraoperative ERCP with LC or LC with laparoscopic common bile duct exploration [22], but these procedures need special equipment and expertise.
During the ERCP, several methods can be used for stone extraction. After endoscopic sphincterotomy, stone extraction is performed by Dormia basket or balloon catheter in 85–90% of cases, according to the experience of the endoscopist [23]. Balloon sphincteroplasty is not used because it presents ten times the risk of postdilatation pancreatitis and delayed papillary stenosis [23]. Presence of an endoprosthesis may have a continued inflammatory effect which could be an obstacle for our study, and so such cases were not included in our study. Due to our experience with the balloon catheter, we used it for extraction.
Although ERCP prior to LC is a widely-accepted procedure, there are few studies about the time interval between ERCP and LC in literature. After ERCP, LC is performed between 24 and 72 h in some studies, but there are also some studies in which LC was performed later than this [20, 24]. In this study we evaluated the difference between patients who underwent LC between 24 and 72 h after ERCP and those who underwent LC more than 72 h after ERCP. The 72 h time point was selected because of the start of the subacute phase of inflammation. The reason for the minimum time period of 24 h in group 1 is to allow time to evaluate patients for pancreatitis due to ERCP. Patients in group 1 had shorter operation times, shorter hospital stays and lower conversion rates. In recent studies it was seen that delayed LC is associated with high conversion rate [25, 26]. For this reason early LC is advised after ERCP. Our results show it is best to perform the operation between 24 and 72 h after ERCP. Also, as time passes, the risk of new CBDS from the gallbladder source and related complications increases. Although some authors mentioned a “wait and see” policy in elderly patients, delayed LC leads to high conversion rates [22]. Some authors showed similar rates between elderly and young populations in early LC after ERCP [25]. Elective operation preparations can take longer in the elderly population for the coexisting diseases, but the operation outcome worsens by the delay [27]. Because we did not include an elderly population in our study, we cannot comment on these results; this may be a subject of another study.
The difference between the two groups comes from the difficulty in the operation. There were more Callot triangle adhesions, which is a sign of inflammation, in group 2. Interestingly, during the operation it was seen that the duodenum was adherent to the common bile duct with loose adhesions. This is probably due to inflammation occurring in contrast agent infusion and ES during ERCP. Kilciler et al. [28] and Chen et al. [29] showed there is an early increase (within 24 h) in the serum interleukin (IL)-2, IL-4, tumor necrosis factor (TNF)α, and IL-6 levels with the development of post-ERCP pancreatitis or without pancreatitis. These findings showed that an acute inflammation process starts early after ERCP. The results support our hypothesis which advises early LC after ERCP.
There is a significant difference in median postoperative hospital stay between the two groups due to the patients who underwent open cholecystectomy. There were more patients who had open cholecystectomy and more postoperative complications, such as wound infections and pulmonary atelectasis, in group 2 patients due to open cholecystectomy.
Among all patients, no severe intraoperative complication was seen. This is probably due to the small number of patients included in our study, the reason for which was the expanded exclusion criteria designed to eliminate inflammation effects. The strict exclusion criteria achieved a more homogenous group but limited the study number. In this way we hoped to eliminate the factors that might affect inflammation.
In conclusion, inflammation after 72 h makes the operation more difficult in patients who undergo preoperative ERCP. We recommend performing LC 24–72-h after ERCP,. We recomment that study series incorporating a larger number of subjects are needed.
References
Sarli L, Iusco DR, Roncoroni L. Preoperative endoscopic sphincterotomy and laparoscopic cholecystectomy for the management of cholecystocholedocholithiasis: 10-year experience. World J Surg. 2003;27:180–6.
Lakatos L, Mester G, Reti G, Nagy A, Lakatos PL. Selection criteria for preoperative endoscopic retrograde cholangiopancreatography before laparoscopic cholecystectomy and endoscopic treatment of bile duct stones: results of a retrospective, single center study between 1996–2002. World J Gastroenterol. 2004;10:3495–9.
Ko CW, Lee SP. Epidemiology and natural history of common bile duct stones and prediction of disease. The NIH State-of-the Science Conference: ERCP for diagnosis and therapy. Gastrointest Endosc. 2002;56:165–9.
Kim KH, Kim W, Lee HI, Sung CK. Prediction of common bile duct stones: its validation in laparoscopic cholecystectomy. Hepatogastroenterology. 1997;44:1574–9.
Fink AS. Current dilemmas in management of common bile duct stones. Surg Endosc. 1993;7:285.
Geron N, Reshef R, Shiller M. The role of endoscopic retrograde cholangiopancreatography in the laparoscopic era. Surg Endosc. 1999;13:452–6.
Cushieri A, Lezoche E, Morino M, Croce E, Lacy A, Toouli J, et al. Multicenter prospective randomized trial comparing two-stage vs single-stage management of patients with gallstone disease and ductal calculi. Surg Endosc. 1999;13:952–7.
Rhodes M, Susman L, Cohen L, Lewis MP. Randomised trial of laparoscopic exploration of common bile duct versus postoperative endoscopic retrograde cholangiography for common bile duct stones. Lancet. 1998;351:159–61.
European Association for Endoscopic Surgery Committee. Diagnosis and treatment of common bile duct stones. Surg Endosc. 1998;12:856–64.
Taylor EW, Rajgopal U, Festekjian J. The efficacy of preoperative endoscopic retrograde cholangiopancreatography in the detection and cleearence of choledocholithiasis. J Soc Laparosc Surg. 2000;4:109–16.
Yamashita Y, Takada T, Kawarada Y, Nimura Y, Hirota M, Miura F, et al. Surgical treatment of patients with acute cholecystitis: Tokyo guidelines. J Hepatobiliary Pancreat Surg. 2007;14:91–7.
Förster S, Klar E. Common bile duct stones. Diagnostic and therapeutic management (in German with English abstract). Chirurg. 2008;79:881–9.
Sarli L, Pietra N, Franze A, Colla G, Costi R, Gobbi S, et al. Routine intravenous cholangiography, selective ERCP, and endoscopic treatment of bile duct stones before laparoscopic cholecystectomy. Gastrointest Endosc. 1999;50:200–8.
Barkun AN, Barkun JS, Fried GM, Ghitulescu G, Steinmetz O, Pham C, et al. Useful predictors of bile duct stones in patients undergoing laparoscopic cholecystectomy. Ann Surg. 1994;220:32–9.
Onken JE, Brazer SR, Eisen GM, Williams DM, et al. Predicting the presence of choledocholithiasis in patients with symptomatic cholelithiasis. Am J Gastreoenterol. 1996;91:762–7.
Barr LL, Frame BC, Coulanjon A. Proposed criteria for preoperative endoscopic retrograte cholangiography in candidates for laparoscopic cholecystectomy. Surg Endosc. 1999;13:778–81.
Hintze RE, Adler A, Veltzke W, Abou-Rebyeh H, Hammerstingl R, Vogl T, et al. Clinical significance of magnetic resonance cholangiopancreatography (MRCP) compared to endoscopic retrograde cholangiopancreatography (ERCP). Endoscopy. 1997;29:182–7.
Sharma SK, Larson KA, Adler Z, Goldfarb MA. Role of cholangiopancreatography in the management of suspected choledocholithiasis. Surg Endosc. 2003;17:868–71.
Eisen GM, Dominitz JA, Faigel DO, Goldstein JL, Kalloo AN, Petersen BT, et al. Standards of practice committee. An annotated algorithm for the evaluation of choledocholithiasis. Gastrointest Endosc. 2001;53:864–6.
Romano F, Franciosi C, Caprotti R, De Fina S, Lomazzi A, Colombo G, et al. Preoperative selective endoscopic retrograde cholangiopancreatography and laparoscopic cholecystectomy without cholangiography. Surg Laparosc Endosc Percutan Tech. 2002;12:408–11.
National Institutes of Health. Consensus development conference statement on gallstones and laparoscopic cholecystectomy. Am J Surg. 1993;165:390–8.
Bergamaschi R, Tuech JJ, Braconier L, Walsøe HK, Mårvik R, Boyet J, et al. Selective endoscopic retrograde cholangiography prior to laparoscopic cholecystectomy for gallstones. Am J Surg. 1999;178:46–9.
Binmoeller KF, Schafer TW. Endoscopic management of bile duct stones. J Clin Gastroenterol. 2001;32(2):106–18.
Costi R, DiMauro D, Mazzeo A, Boselli AS, Contini S, Violi V, et al. Routine laparoscopic cholecystectomy after endoscopic sphincterotomy for choledocholithiasis in octogenarians: is it worth the risk? Surg Endosc. 2007;21(1):41–7.
Boerma D, Rauws EA, Keulemans YC, Janssen IM, Bolwerk CJ, Timmer R, et al. Wait-and-see policy or laparoscopic cholecystectomy after endoscopic sphincterotomy for bile-duct stones: a randomised trial. Lancet. 2002;360:761–5.
Lau JY, Leow CK, Fung TM, Suen BY, Yu LM, Lai PB, et al. Cholecystectomy or gallbladder in situ after endoscopic sphincterotomy and bile duct stone removal in Chinese patients. Gastroenterology. 2006;130:96–103.
Hazan D, Geron N, Golijanin D, Reissman P, Shiloni E. Laparoscopic cholecystectomy in octogenarians. Surg Endosc. 2003;17:773–6.
Kilciler G, Musabak U, Bagci S, Yesilova Z, Tuzun A, Uygun A, et al. Do the changes in the serum levels of IL-2, IL-4, TNFα, and IL-6 reflect the inflammatory activity in the patients with post-ERCP pancreatitis? Clin Dev Immunol. 2008;2008:481560.
Chen CC, Wang SS, Lu RH, Lu CC, Chang FY, Lee SD. Early changes of serum proinflammatory and anti-inflammatory cytokines after endoscopic retrograde cholangiopancreatography. Pancreas. 2003;26:375–80.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Salman, B., Yılmaz, U., Kerem, M. et al. The timing of laparoscopic cholecystectomy after endoscopic retrograde cholangiopancreaticography in cholelithiasis coexisting with choledocholithiasis. J Hepatobiliary Pancreat Surg 16, 832–836 (2009). https://doi.org/10.1007/s00534-009-0169-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00534-009-0169-4