Abstract
Background
Different approaches are available for the treatment of combined cholecystocholedocholithiasis including totally laparoscopic (TL) treatment, simultaneous laparoendoscopic treatment, and sequential treatments (ST) combining endoscopic retrograde cholangiopancreatography (ERCP) and endoscopic sphincterotomy (ES) with cholecystectomy. This review aimed to clarify the issue of the simultaneous laparoendoscopic rendezvous (RV).
Methods
A careful analysis of papers was performed to determine the results, technical differences, limits, disadvantages, and advantages of RV compared with other options.
Results
Data were collected from 27 papers concerning 795 patients. The overall effectiveness of RV was 92.3%. The morbidity rate was 5.1%, and the mortality rate was 0.37%. Almost all the authors were satisfied with the procedure. The authors’ comparison to ST and TL showed that the advantages outweigh the disadvantages mostly related to logistical problems.
Conclusions
There is confusion concerning the definitions and techniques of RV due to differences in combining surgical and endoscopic steps of the procedure. The results are at least comparable with those of the other available approaches. The effectiveness of RV is greater with reciprocal implementation of surgical and endoscopic procedures. The morbidity and the risk of iatrogenic damage seem lower than with ERCP-ES and the risk of residual stones lower than with TL treatment. The RV procedure is safe and can sometimes be the preferable option, but collaboration between surgeon and endoscopist is mandatory.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Gallstones are a very common disease whose treatment involves general practitioners, gastroenterologists, anesthesiologists, surgeons, and endoscopists. The management of patients affected by gallstones complicated by diagnosed or suspected common bile duct (CBD) stones frequently is related to problems at the papilla of Vater. These problems are the possible cause of severe complications such as acute biliary pancreatitis, jaundice and cholangitis. The “gold standard” treatment for cholecystolithiasis is laparoscopic cholecystectomy (LC), whereas the “gold standard” treatment for isolated CBD stones, especially in cholecystectomized patients, is endoscopic clearance. On the contrary, when an association exists between cholecystolithiasis and CBD stones, the treatment still is a challenge, and a consensus has not been found to date because different possible approaches are used, all effective, such as open surgery, laparoscopy, and laparoendoscopic treatments, either sequential or simultaneous.
Before the development of minimally invasive surgery, when the surgical approach to CBD stones consisted of choledocholithotomy by open surgery, the morbidity was relevant and the mortality not inappreciable. The development of endoscopic procedures, especially sphincterotomy in 1974 [1, 2], appeared to be extremely important for surgeons as a way to limit major biliary surgery for stones.
Currently, in the era of minimally invasive surgery, it seems clear that all efforts must be made to avoid conversion to open surgery for choledocotomy with its risk of complications [3–5]. Therefore, refined endoscopic procedures have regained clinical favor in the management of CBD stones [6]. Certainly, the possible complications of endoscopic retrograde cholangiopancreatography (ERCP) with endoscopic sphincterotomy (ES) and the nonsimultaneous treatment of the gallbladder and CBD stones were the main factors that led Deslandres et al. [7] in 1993, first to report this new combined laparoendoscopic treatment for three patients. In the same year, Mayrhofer et al. [8] also reported this combined approach for 32 open cholecystectomies and 1 LC.
The procedure described by Deslandres et al. [7] consisted of an intraoperative ERCP performed by the endoscopist after transcystic insertion of a guidewire to reach the Vater ‘s papilla and render the cannulation of the papilla easier, with eventual sphincterotomy and endoscopic clearance of the CBD by a balloon or a basket. The procedure was completed with LC. Feretis et al. [9] in 1994 were the only ones to publish the results of laparoscopic transcystic anterograde sphincterotomy with a hydrophilic guidewire for 12 patients using the endoscope alone to control the sphincterotomy. In 1996, Nakajima et al. [10] published a technical note pointing out the importance of the transcystic guidewire but reporting also their unsatisfactory experience with the anterograde transcystic sphincterotomy.
These combined approaches did not gain immediate interest. Slowly and independently, many authors initially attempted these techniques in the clinical routine. Miscusi et al. [11] in 1997 was the first to use the term “rendezvous” for this simultaneous laparoendoscopic treatment. Although more then 2,000 papers have been published concerning the other two main therapeutic options for combined gallstones and CBD stones, only a few of these papers concern the combined simultaneous laparoendoscopic procedure (RV). This report indeed is the first and only review of this issue, describing the results as well as the opinions of the authors and also comparing the RV treatment with the other two main available treatment options.
Methods
We conducted a careful search of the Pub Med databases using the following keywords: “laparoendoscopic rendezvous,” “laparoendoscopic procedure,” “ERCP,” “intraoperative cholangiography,” “intraoperative endoscopic sphincterotomy,” “cholecystolithiasis,” “choledocolithiasis,” “gallstones,” and “common bile duct stones.” The titles and abstracts that matched with our search were assessed and the relevant articles acquired.
To assess the largest samples of available information, we also checked the references of the acquired articles, trying to avoid missing pertinent papers. The data were collected and analyzed in terms of definitions, technical features, and their differences, as well as the possible relationship between a technique’s variation and the results. The duration of the endoscopic procedures alone was acquired and analyzed as well as the duration of the entire procedures, the hospital stay, the conversion rate, the morbidity rate, and the mortality rate. Besides the analysis of the clinical data, all the main evaluations and considerations concerning the limits, advantages, and disadvantages of the RV procedure, if clearly expressed by the authors in their papers, were recorded. Special consideration was given to comparison of RV with the other available options.
All these opinions were arranged in tables. To complete the review, a comparison with the results described in the most relevant recent papers concerning the other two main treatment options was performed.
Results
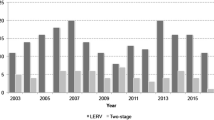
The published papers describing patients treated with a single-stage laparoendoscopic treatment of gallstones and CBD stones are shown in Table 1 [7, 13–30]. The data were collected from 20 original papers reporting studies involving 8 [11] to 93 [26] patients. In addition, another 7 reports of one or a few cases were considered [7, 8, 10, 31–34], which collected another 12 patients, allowing us to consider a total of 799 patients. Four patients were excluded by the authors before they attempted the combined treatment, leaving 795 patients [28].
The 12 case reports all described successful treatment, with an overall effectiveness of 100% and no reported negative aspects. The reported effectiveness of CBD stone clearance varied in a wide range, from 69.2% [19] to 100% [11, 12, 30], but unfortunately, the criteria for the selection of patients for this treatment were mostly unclear or not available. These results concerning the effectiveness seemed unrelated to the experience, the number of patients treated, or the time of the studies. However, all the series reported after 2004 show an effectiveness greater than 91.4% [26]. Only the limited series reported in 2002 by William and Vellacott [19] registered a low success rate of 69.2%, and only four other series reported a success rate lower than 90% [13, 17, 22, 23].
Using the data in Table 1, we calculated that the real overall effectiveness of RV was 92.3% (734/795 patients). The duration for the endoscopic part of the RV procedure, when reported, ranged from 9 to 82 min (mean, 35 min). The time for the whole RV procedure was 40 to 360 min (mean, 104 min). The hospital stay was 2 to 51 days (mean, 3.9 days). The conversion rates to open surgery varied largely from 0% reported by 7 authors [11–13, 18, 21, 24, 30] to 14% [22], for an overall conversion rate of 4.7%. Of 27 papers, 24 (88.8%) did not report mortality. Consequently, the three isolated exceptions produced a range of 1.9% [13] to 7.8% [19], but each of the three papers reported a single death each, for an overall calculated mortality rate of 0.37%. The reported morbidity rate ranged from 0% [8, 16–18] to 19% [19], but the calculated mean morbidity rate was 5.1%.
In Table 2 we summarize the main data only of papers precisely reporting complications. Bleeding from the sphincterotomy (1.6–6%) [14, 23, 25, 28–30] and acute pancreatitis (1.7–7.6%) [14, 20, 23, 26–28] were the main complications, variously reported in 54.5% of the papers. Retroperitoneal perforation, retained stones, and postoperative pneumonia were reported by 22% of the papers, with cholangitis and CBD perforation reported by 11%.
We also analyzed the main limitations of this procedure encountered by the authors as an indication of its feasibility. Prepapillary giant impacted stones were reported by six authors (range, 1.5–7%) [18, 20, 22, 24, 27, 29] and preampullary diverticula by three authors (range, 1.9–7.6%) [18–20]. Other isolated limitations registered were Mirizzi syndrome or adhesions [25] and stenosant papillitis or cancer of the duodenum [22].
Table 3 presents all the opinions of the authors concerning all the disadvantages of RV compared with both sequential treatments (ST) and totally laparoscopic (TL) treatment. Six papers suggest that the disadvantages of the RV approach compared with the TL procedure [11, 19–21, 23, 30] seem to be mostly the logistic and organizational difficulty of an operation needing the simultaneous presence of a surgeon and an endoscopist [11, 19, 20, 30]. Higher rates of conversion and morbidity are reported only by one author [23] and increased costs by two authors [21, 23]. Ten papers report disadvantages of the RV approach compared with ST, and 80% of these authors report logistic problems with organization of the procedure [19–22, 24, 25, 27, 29, 30]. For 70%, the longer operation time for cholecystectomy was also an issue [18, 20–22, 24, 25, 29]. Other disadvantages suggested by a few papers are the need to change the intraoperative patient’s position during surgery [22], technical difficulties [22, 27], and increased costs [21].
The suggested advantages of RV clearly outnumber the reported disadvantages, so that they could not be summarized in one single table. The advantages of the RV approach compared with TL summarized on Table 4 are suggested by 11 papers, with each author suggesting two or more advantages. Among the most cited are the reduced operation time, reported by 72.7% [7, 14, 15, 18–20, 23–26, 30], and lower technical difficulties, reported by 63.6% [7, 15, 18, 20, 24–26]. Reduced cost and complexity of the equipment required also are reported advantages [11, 20, 24, 28]. Other relevant advantages such as higher effectiveness in particular cases and better feasibility in the case of prepapillary or impacted stones are registered [7, 18, 23, 24, 30].
The advantages of the RV procedure suggested by the authors compared with the two possible pathways of ST (pre- or postoperative ERCP-ES) are summarized on Table 5. In the 16 papers reporting these advantages, they appear to be conceptual, logistic, or clinical. For 75% of the authors, RV avoids unnecessary preoperative ERCP [13, 15, 18–22, 24, 25, 28–30]. For 68.7%, it has all the advantages of a single procedure [20, 22, 24, 25, 27, 28, 30] compared with the discomfort of a sequential treatment [7, 13–15, 17, 19, 24, 25, 27]. It reduces the risk of reoperation [13, 15, 18–20, 22, 24, 25, 27, 28, 30] according to 62.5% of the authors. For 43.7% of the authors, it requires a single anesthesia [7, 14, 17, 19–21, 25–27, 30], and for 62.5%, RV facilitates the endoscopic procedure [13, 15, 20, 22, 25–30], also reducing the endoscopic time [14, 30].
The main clinical advantages are a reduced incidence of complications reported by 56.2% of the authors [7, 13, 18, 19, 22, 24, 28–30], a higher success rate reported by 31.2% [17, 27–30], a shorter hospital stay reported by 56.2% [13, 17–20, 22, 24, 27, 29, 30], and reduced costs reported by 31.2% [17, 18, 25, 27, 28].
Discussion
We underscore that there certainly is relevant confusion concerning the definition of the combined approach because of conceptual and technical differences. A common standard ERCP-ES can be performed during, immediately before, or even after LC, and these can be considered combined laparoendoscopic approaches, but they are not really RV procedures. Improperly, many consider the RV approach only as the addition of two different procedures performed separately during the same anesthesia. On the other hand, others have tried to improve the outcome for each patient by implementing the positive aspects of some steps from both parts of the procedure in one “optimized” procedure.
The two most important conceptual factors of the RV approach seem to be the aim to avoid the main risk factors of iatrogenic damage caused by the retrograde ERCP-ES and the attempt to render both the endoscopic and laparoscopic procedures easier. The main well-known negative factors of standard ERCP to be avoided are principally three: the retrograde injection of contrast medium, the retrograde insertion of the guidewire, and the prolonged manipulation of the papilla [35, 36]. An RV also can be performed in delayed time, leaving the guidewire passed during LC inside the bile duct and duodenum with the aim of facilitating the cannulation of the papilla a few days later [37, 38].
This review also concerned all the relevant technical aspects suggested by the different authors. Basso et al. [13] and others [27, 30] consider it very important to perform a total dissection of the gallbladder before performing the cysticotomy and cholangiography and before the beginning of the endoscopic procedure. This is important to avoid bowel distension due to endoscopic air inflation, which would make it more difficult to complete the LC. To overcome this bowel distension, Morino et al. [27] suggest using a laparoscopic bowel clamp applied on the first jejunal loop. Others more simply suggest minimizing the inflation and prolonging the aspiration before extracting the endoscope [17]. As pointed out earlier, the main crucial point of RV is the insertion of the guidewire to assist in cannulation of the papilla, which should be performed routinely, as suggested first by Miscusi et al. [11] and also by many others [12, 18, 22, 24, 25, 27].
On the contrary, in the attempt to minimize the trauma of manipulation to the papilla of Vater, others consider a more tailored approach to be better. They limit the guidewire insertion only to the cases in which the endoscopist is not able to cannulate the papilla without help [13, 16, 25, 30].
The transcystic injection of saline is a useful maneuver facilitating endoscopic localization and cannulation of the papilla [30]. The surgeon’s aid is a clear advantage in this procedure because an endoscopic retrograde cannulation failure can be related to an unsuccessful ERCP in 14% to 23% of cases [19, 22]. Sometimes the surgeon also is an experienced endoscopist, and this is the best situation for overcoming many logistical problems [19]. When a standard ERCP-ES immediately before or after LC is performed instead of an RV, the simple need to change the patient’s position on the operating table from supine to lateral will render the procedure longer and more complex, missing a positive factor of the combined optimized RV procedure. In addition, during isolated postoperative ERCP, the surgeon’s help is excluded, and the contrast medium must be injected again, but retrogradely by the endoscopist, unnecessarily repeating X-ray exposure and adding the iatrogenic risk of retrograde Wirsung injection and acute pancreatitis [25, 27, 29, 30].
Positive experiences with RV also are described for children with recurrent acute biliary pancreatitis [34]. Critically analyzing the data of Table 1 with the aim of finding differences related to technical variation, we found that one crucial point is represented by the use of the guidewire. The overall calculated mean effectiveness shown by Table 1 is 92.3%. However, in the nine papers [13–15, 18–21, 23, 26] not reporting use of the guidewire to help cannulation, the effectiveness ranges from 69.2% [19] to 93.9% [14], with an overall mean of 90.2% (371/411). On the contrary, in the remaining collected group using the guidewire, the effectiveness increases, ranging from 85.7% [17] to 100% [11, 12, 30], with an overall effectiveness of 94.5% (363/384 patients). Therefore the mean effectiveness is 4.3% higher with usage of a guidewire, confirming the importance of reciprocal implementation between surgeon and endoscopist [7, 12, 22, 23].
To complete this review, we also performed a short comparison with the other available treatment options. In comparing RV with TL CBD exploration, only the study by Hong et al. [26] was randomized, but a relevant difference for 34% of the groups and intraoperative diagnosis reduced the validity of the randomization and the results. The other comparison, by Wei et al. [23], was retrospectively performed. The success rate for the laparoendoscopic treatment was higher in both studies (91.4%, 89%) than that registered for the TL treatment (89.3%, 88%), but guidewire help was not mentioned. In both studies [23, 26], the incidence of retained stones with the laparoendoscopic treatment was one-half that with TL (1.1% and 1.8% vs. 2.3% and 5%, respectively). Moreover, a salvage procedure such as intra- or postoperative ERCP-ES or trans T-tube treatment was not infrequently needed to resolve retained stones in the case of TL treatment, whereas they were never reported for RV. It therefore seems clear that RV often solves coexisting problems involving the papilla of Vater, which cannot always be definitively solved by TL CBD exploration. These problems at the papilla are recognized as the well-known main causes of retained stones and recurrence.
Another relevant question concerns the difficult choice of the best treatment when the surgeon must deal with an unclear intraoperative cholangiography, with uncertain images of stones or a relevant delay in the passage of the contrast medium in the duodenum. In these situations, neither transcystic nor transcholedochotomic TL exploration is the most rational solution, and only intraoperative ES can be the definitive solution for bile flow obstruction due to dense biliary sludge or stenosis of the papilla or sphincter of Oddi’s dysfunction.
The TL CBD exploration consists of major biliary surgery that needs higher laparoscopic skills and prolongs the entire operation, also increasing the overall risk for the patient even with very experienced teams [37, 38]. The calculated mean prolongation of the time for RV with respect to a simple LC is 33 min, much shorter than that reported for laparoscopic CBD exploration, in which the surgeon must dissect, open, and inspect the CBD to extract the stones, insert the drain, and finally, precisely suture the bile duct to avoid leaks and strictures [39–41].
A recent review concerning laparoscopic CBD exploration shows an overall conversion rate of 2% to 8% and a failure rate of 3.1%. Consequently, these patients often must be treated again by the endoscopist in a sequential manner, also with the risk of ineffectiveness [38]. The incidence of retained stones (≤8%) and the need for biliary drainage after surgical transverse choledocotomy (≤94%) raise the need for repeated controls, prolonged hospitalization, and readmissions [39]. Particular but not rare situations such as large or multiple stones or a thin CBD do not seem to contraindicate performing the laparoendoscopic RV differently from the TL clearance, although these could complicate the treatment and increase the risk of early and late morbidity and recurrence of stones [7, 12, 15, 16, 18, 30].
The success rate for TL exploration in a review of 28 papers [38] was 81% to 98% (mean, 88.4%), with a rate of 0% to 19% for retained stones, and a conversion rate reaching 10%. The large randomized multicentric European Association of Endoscopic Surgery (EAES) trial by Cuschieri et al. [42] comparing endoscopic and surgical treatment of CBD stones showed a therapeutic success rate of 84% for the ERCP-ES and a success rate of 83% for the laparoscopic exploration, both lower than the overall rate of 92.3% for the laparoendoscopic treatment calculated in this review.
A recent multicentric retrospective analysis of the Association Francaise de Chirurgie published by Berthou et al. [43] and involving 505 patients reported that the laparoscopic approach to CBD stones had an overall morbidity rate of 7.9% (general complication rate of 3.1%) and a mortality rate of 1%. Both parameters were higher than those calculated in this review for laparoendoscopic treatment. The large precise analysis of Cuschieri et al. [42] showed also that the patients matched for simple cholecystectomy reported a significantly lower morbidity than that for laparoscopic CBD treatment because biliary complications can involve 16% of the patients and are mostly attributable to the need for biliary drains. With the laparoendoscopic treatment, these risks related to CBD surgery are avoided.
In comparing the laparoendoscopic approach with the sequential approach, it should be underscored that ERCP, whenever possible, should be limited as suggested by experienced endoscopists stating “The only sure way to avoid post-ERCP complications is to avoid ERCP itself” [44]. The aim of the RV procedure also is to avoid or minimize the negative aspects and risks of a standard ERCP. The old but still existing fear of ES and its late complications could be minimized currently because more than 90% of patients who undergo ERCP-ES are free of biliary symptoms after more than 14.2 years, and the majority of patients will have no further biliary events during the remainder of their lives [45]. Currently, a single-stage therapy certainly should be preferred for several reasons, such as the reduction of anesthetic procedures and the hospital stay [7, 14, 17, 19–21, 25–27, 30, 42].
Some authors [46, 47] consider TL treatment the best option for CBD stones, forgetting that for a long time the sequential approach was considered as preferable [48–50] and that many gastroenterologists, endoscopists, and surgeons still prefer it [50–52]. Thus, the best practice has never been clearly defined [53]. A recent National Institutes of Health (NIH) state-of-the-science statement on ERCP [54] and a Cochrane Database review [55] showed that both ERCP and laparoscopic CBD clearance are safe and reliable for clearing stones. Therefore, the combination of laparoscopy and ERCP-ES should be considered equally safe and reliable, and the RV approach should be considered preferable, especially for the patient. The RV approach eliminates the problem of optimal timing between ERCP and LC [56], as suggested by many authors [13, 15, 18–22, 24, 25, 28–30], and decreases the risks of ineffective ERCP and reoperation related to both pathways of the sequential approach and directly to the lack of synchronization between cholangiographic diagnosis of CBD stones and its treatment [13, 15, 18–20, 22, 24, 25, 27, 28, 30] because only during the RV procedure does the intraoperative cholangiogram show the “real-time” picture of the CBD and the pathophysiology of the papilla. On the contrary, with both pathways of the sequential ERCP-ES, a passage of stones to the CBD may occur in the period between the two procedures so that ERCP-ES can be unnecessary if performed after LC because stones can spontaneously pass the papilla, or it can be useless and needing to be repeated if performed before LC because other stones can pass in the CBD after ERCP or during LC [57].
A recent study analyzing the management of suspected CBD stones in children [58] showed clearly the poor results and pitfalls of the two common sequential pathways of ERCP-ES. If performed before LC, 71% of ERCPs were unnecessary, and 7% failed. If performed after LC, 50% of ERCP were unnecessary because stones were no longer found. Therefore, a large number of unnecessary X-ray administrations and invasive procedures all related to iatrogenic risks still are performed. The only two prospective randomized comparisons of sequential ERCP-ES with laparoendoscopic RV, by Morino et al. [27] and Rabago et al. [28], confirm these aspects. The first comparison shows that the risk of incomplete duct clearance with ERCP-ES is 20% and that in 77.7% of the cases, the cause is inability to cannulate the papilla. In 88% of these ineffective preoperative ERCP-ES procedures, the intraoperative ERCP-ES during the RV procedure was effective. This confirms the main advantage of RV for the endoscopist, namely, help for the surgeon in passing the guidewire, which increases feasibility and effectiveness in cannulation and clearing of the CBD.
To underscore the importance of collaboration, radiologic–endoscopic rendezvouses also have been published [53, 59–61]. Rabago et al. [28] showed that, interestingly, the morbidity rate clearly was higher in the sequential approach than in the RV pathway (23% vs. 8.5%). Especially after ERCP, the pancreatitis rate was significantly higher (12.7% vs. 1.7%). Moreover, after ERCP, the cholecystitis rate was 4.8%, whereas it was impossible after RV. The rates for both papillotomy (79.7 vs. 33.9%) and precut papillotomy (15.6% vs. 1.7%) were significantly higher after ERCP-ES than after RV. The need of postprocedural repeated ERCP in the sequential group (10.2%) was double that in the RV group (5.2%). Therefore, the authors concluded that despite comparable effectiveness, the intraoperative ERCP carries a significantly lower morbidity rate, a shorter hospital stay, and reduced costs.
The incidence of morbidity among this collected group of 795 patients in our review was 5.1%, lower than the 9.8% reported in one of the largest prospective multicentric studies on endoscopic sphincterotomy involving 2,397 patients [62]. On the other hand, it also is important to note that all the surgeons using the RV have been consistently satisfied with this procedure, never reporting results or aspects that led them to abandon it [7, 11, 13–17, 20–23, 25, 27–30].
Concluding this analysis, it is necessary to underscore that the laparoendoscopic RV approach to cholelithiasis and CBD stones is not always preferable. The cases in which the CBD stones are easily extractable through the cystic duct by a skilled laparoscopic surgeon should be clearly excluded from this discussion. Unfortunately, however, this evaluation is never possible before surgery, so an algorithm of treatment options is mandatory for each patient. For patients with only a few small stones in the CBD, laparoscopic transcystic clearance remains the best option. Otherwise, the RV procedure could be a good option intraoperatively, often the preferable choice for both the patient and the managing team, especially in complicated cases of large, multiple, and friable CBD stones as well as a normal or thin CBD, especially when combined with sphincter of Oddi dysfunction or stenosis of the papilla.
In both the 1999 and 2006 guidelines published by the EAES [63, 64], the suggestions concerning the best treatment for combined cholecystocholedocholithiasis were extremely uncertain, as reflected in the conclusions of the 18 panelists in 1998 [63], “There is no standard treatment today,” and in 2006, “The best therapeutic strategies remain uncertain” [64]. The combined laparoendoscopic RV approach was only mentioned in 2006 as follows: “Most frequently, the also minimally invasive treatment option combining laparoscopy and conventional interventional endoscopy is applied, …” and “possible reasons are that laparoscopic CBD surgery requires demanding technical skills” … and “therefore an interdisciplinary team approach is important … and success depends on the strength of the team” [64].
Certainly the limited data concerning the effectiveness of this combined approach have caused its underevaluation by surgeons. Large randomized trials of this approach certainly are needed, starting with a precise definition of the type and steps of the best possible RV procedure, because relevant technical and conceptual differences still exist. This review aims to clarify this issue of combined laparoendoscopic treatment, and we can conclude that despite the limited experiences, the results in terms of effectiveness in stone clearance and reduction of incomplete clearance seem comparable with or better than the results achieved with the other two available options.
The safety of the RV procedure in terms of reduced morbidity and minimal mortality is higher than with both of the other two available options. We believe that the reciprocal control of both the endoscopist and surgeon could itself be a factor favoring a good outcome. All the published reports also are favorable if written mostly by experienced endoscopists or skilled laparoscopic surgeons who still consider this combined approach as the least invasive for treating combined cholecystocholedocholithiasis [65] 15 years after the proposal of this procedure [7] despite general improvement of skills. This approach unfortunately limits the opportunities to gain surgical expertise and training with laparoscopic CBD exploration.
The suggested advantages of the laparoendoscopic RV procedure over ST and TL treatment are greater than the disadvantages. Moreover, the advantages are conceptual, technical, and clinical, whereas the disadvantages are mostly only logistic, underscoring the well-known individualism of surgeons and endoscopists that often limits the possibility of collaboration for the best implementation of the procedure in the patient’s best interest. The reluctance for mandatory collaboration still seems the main factor that limits the diffusion of this simple, effective, and safe procedure.
References
Kawai K, Akasaka Y, Murakami K, Tada M, Koli Y (1974) Endoscopic sphincterotomy of the ampulla of Vater. Gastrointest Endosc 20:148–151
Ponsky JL (2006) Endoluminal surgery: past, present, and future. Surg Endosc 20(Suppl 2):500–502
Frazee RC, Roberts J, Symmonds R, Hendricks JC, Snyder S, Smith R, Custer MD, Stoltenberg P, Avots A (1993) Combined laparoscopic and endoscopic management of cholelithiasis and choledocholithiasis. Am J Surg 166:702–705
Arregui ME, Davis CJ, Arkush AM, Nagan RF (1992) Laparoscopic cholecystectomy combined with endoscopic sphincterotomy and stone extraction or laparoscopic choledochoscopy and electrohydraulic lithotripsy for management of cholelithiasis with choledocholithiasis. Surg Endosc 6:10–15
Paganini AM, Guerrieri M, Sarnari J, De Sanctis A, D’Ambrosio G, Lezoche G, Lezoche E (2005) Long-term results after laparoscopic transverse choledochotomy for common bile duct stones. Surg Endosc 19:705–709
Neoptolemos JP, Carr-Locke DL, Fraser I, Fossard DP (1984) The management of common bile duct calculi by endoscopic sphincterotomy in patients with gallbladders in situ. Br J Surg 71:69–71
Deslandres E, Gagner M, Pomp A, Rheault M, Leduc R, Clermont R, Gratton J, Bernard EJ (1993) Intraoperative endoscopic sphincterotomy for common bile duct stones during laparoscopic cholecystectomy. Gastrointest Endosc 39:54–58
Mayrhofer T, Schmiedered R, Razek P (1993) Intraoperative endoscopic papillotomy and stone removal. Endosc Surg Allied Technol 1:144–149
Feretis C, Kalliakmanis B, Benakis P, Apostolidis N (1994) Laparoscopic transcystic papillotomy under endoscopic control for bile duct stones. Endoscopy 26:697–700
Nakajima H, Okubo H, Masuko Y, Osawa S, Ogasawara K, Kambayashi M, Hata Y, Oku T, Takahashi (1996) Intraoperative endoscopic sphincterotomy during laparoscopic cholecystectomy. Endoscopy 28:264
Miscusi G, Gasparrini M, Petruzziello L, Taglienti D, Onorato M, Otti M, Montori J (1997) Endolaparoscopic “Rendez-vous” in the treatment of cholecystocholedochal calculosis. G Chir 18:655–657
Cavina E, Franceschi M, Sidoti F, Goletti O, Buccianti P, Chiarugi M (1998) Laparoendoscopic “rendezvous”: a new technique in the choledocholithiasis treatment. Hepatogastroenterology 45:1430–1435
Basso N, Pizzuto G, Surgo D, Materia A, Silecchia G, Fantini A, Fiocca F, Trentino P (1999) Laparoscopic cholecystectomy and intraoperative endoscopic sphincterotomy in the treatment of cholecysto-choledocholithiasis. Gastrointest Endosc 50:532–535
Cemachovic I, Letard JC, Begin GF, Rousseau D, Nivet JM (2000) Intraoperative endoscopic sphincterotomy is a reasonable option for complete single-stage minimally invasive biliary stones treatment: short-term experience with 57 patients. Endoscopy 32:956–962
Kalimi R, Cosgrove JM, Marini C, Stark B, Gecelter GR (2000) Combined intraoperative laparoscopic cholecystectomy and endoscopic retrograde cholangiopancreatography: lessons from 29 cases. Surg Endosc 14:232–234
Tatulli F, Cuttitta A (2000) Laparoendoscopic approach to treatment of common bile duct stones. J Laparoendosc Adv Surg Tech A 10:315–317
Filauro M, Comes P, De Conca V, Coccia G, Prandi M, Bagarolo C, Marini P, Anfossi A (2000) Combined laparoendoscopic approach for biliary lithiasis treatment. Hepatogastroenterology l47:922–926
Iodice G, Giardiello C, Francica G, Sarrantonio G, Angelone G, Cristiano S, Finelli R, Tramontano G (2001) Single-step treatment of gallbladder and bile duct stones: a combined endoscopic–laparoscopic technique. Gastrointest Endosc 53:336–338
Williams GL, Vellacott KD (2002) Selective operative cholangiography and perioperative endoscopic retrograde cholangiopancreatography (ERCP) during laparoscopic cholecystectomy: a viable option for choledocholithiasis. Surg Endosc 16:465–467
Meyer C, Le JV, Rohr S, Duclos B, Duclos B, Reimund JM, Baumann R (2002) Management of common bile duct stones in a single operation combining laparoscopic cholecystectomy and peroperative endoscopic sphincterotomy. J Hepatobiliary Pancreat Surg 9:196–200
Wright BE, Freeman ML, Cumming JK, Quickel RR, Mandal AK (2002) Current management of common bile duct stones: is there a role for laparoscopic cholecystectomy and intraoperative endoscopic retrograde cholangiopancreatography as a single-stage procedure? Surgery 132:729–735
Tricarico A, Cione G, Sozio M, Di Palo P, Bottino V, Tricarico T, Tartaglia A, Iazzetta I, Sessa E, Mosca S, De Nucci C, Falco P (2002) Endolaparoscopic rendezvous treatment: a satisfying therapeutic choice for cholecystocholedocolithiasis. Surg Endosc 16:585–588
Wei Q, Wang JG, Li LB, Li JD (2003) Management of choledocholithiasis: comparison between laparoscopic common bile duct exploration and intraoperative endoscopic sphincterotomy. World J Gastroenterol 9:2856–2858
Enochsson L, Lindberg B, Swahn F, Arnelo U (2004) Intraoperative endoscopic retrograde cholangiopancreatography (ERCP) to remove common bile duct stones during routine laparoscopic cholecystectomy does not prolong hospitalization: a 2-year experience. Surg Endosc 18:367–371
Saccomani G, Durante V, Magnolia MR, Ghezzo L, Lombezzi R, Esercizio L, Stella M, Arezzo A (2005) Combined endoscopic treatment for cholelithiasis associated with choledocholithiasis. Surg Endosc 19:910–914
Hong DF, Xin Y, Chen DW (2006) Comparison of laparoscopic cholecystectomy combined with intraoperative endoscopic sphincterotomy and laparoscopic exploration of the common bile duct for cholecystocholedocholithiasis. Surg Endosc 20:424–427
Morino M, Baracchi F, Miglietta C, Furlan N, Ragona R, Garbarini A (2006) Preoperative endoscopic sphincterotomy versus laparoendoscopic rendezvous in patients with gallbladder and bile duct stones. Ann Surg 244:889–893
Rabago LR, Vicente C, Soler F, Delgado M, Moral I, Guerra I, Castro JL, Quintanilla E, Romeo J, Llorente R, Vázquez Echarri J, Martínez-Veiga JL, Gea F (2006) Two-stage treatment with preoperative endoscopic retrograde cholangiopancreatography (ERCP) compared with single-stage treatment with intraoperative ERCP for patients with symptomatic cholelithiasis with possible choledocholithiasis. Endoscopy 38:779–786
Lella F, Bagnolo F, Rebuffat C, Scalambra M, Bonassi U, Colombo E (2006) Use of the laparoscopic–endoscopic approach, the so-called “rendezvous” technique, in cholecystocholedocholithiasis: a valid method in cases with patient-related risk factors for post-ERCP pancreatitis. Surg Endosc 20:419–423
La Greca G, Barbagallo F, Di Blasi M, Di Stefano M, Castello G, Gagliardo S, Latteri S, Russello D (2007) Rendezvous technique versus endoscopic retrograde cholangiopancreatography to treat bile duct stones reduces endoscopic time and pancreatic damage. J Laparoendosc Adv Surg Tech A 17:167–171
Sarli L, Sabadini G, Pietra N, Longinotti E, Carreras F, Peracchia A (1995) Laparoscopic cholecystectomy and endoscopic sphincterotomy under a single anesthetic: a case report. Surg Laparosc Endosc 5:68–71
Turcu F (2000) The laparoscopic approach to cholecystocholedocholithiasis. The “rendezvous” technique. Chirurgia 95:463–467
Dell’Abate P, Del Rio P, Soliani P, Arcuri M, Sianesi M (2003) Use of the transcystic guidewire in single-intervention treatment for cholecystocholedocholithiasis: a case report and technical notes. Chir Ital 55:309–312
La Greca G, Di Blasi M, Barbagallo F, Di Stefano M, Latteri S, Russello D (2006) Acute biliary pancreatitis and cholecystolithiasis in a child: one time treatment with laparoendoscopic “rendezvous” procedure. World J Gastroenterol 21:1782–1785
De Palma GD, Angrisani L, Lorenzo M, Di Matteo E, Catanzano C, Persico G, Tesauro B (1996) Laparoscopic cholecystectomy (LC), intraoperative endoscopic sphincterotomy (ES), and common bile duct stones (CBDS) extraction for management of patients with cholecystocholedocholithiasis. Surg Endosc 10:649–652
Moroni J, Haurie JP, Judchak I, Fuster S (1999) Single-stage laparoscopic and endoscopic treatment for choledocholithiasis: a novel approach. J Laparoendosc Adv Surg Tech A 9:69–74
Paganini AM, Guerrieri M, Sarnari J, De Sanctis A, D’Ambrosio G, Lezoche G, Perretta S, Lezoche E (2007) Thirteen years’ experience with laparoscopic transcystic common bile duct exploration for stones: effectiveness and long-term results. Surg Endosc 21:34–40
Thompson MH, Tranter SE (2002) All-comers policy for laparoscopic exploration of the common bile duct. Br J Surg 89:1608–1612
Tranter SE, Thompson MH (2002) Comparison of endoscopic sphincterotomy and laparoscopic exploration of the common bile duct. Br J Surg 89:1495–1504
Tokumura H, Umezawa A, Cao H, Sakamoto N, Imaoka Y, Ouchi A, Yamamoto K (2002) Laparoscopic management of common bile duct stones: transcystic approach and choledochotomy. J Hepatobiliary Pancreat Surg 9:206–212
Nathanson LK, O’Rourke NA, Martin IJ, Fielding GA, Cowen AE, Roberts RK, Kendall BJ, Kerlin P, Devereux BM (2005) Postoperative ERCP versus laparoscopic choledochotomy for clearance of selected bile duct calculi. Ann Surg 242:188–192
Cuschieri A, Lezoche E, Morino M, Croce E, Lacy A, Toouli J, Faggioni A, Ribeiro VM, Jakimowicz J, Visa J, Hanna GB (1999) E.A.E.S. multicenter prospective randomized trial comparing two-stage vs. single-stage management of patients with gallstone disease and ductal calculi. Surg Endosc 13:952–957
Berthou JCh, Dron B, Charbonneau P, Moussalier K, Pellissier L (2007) Evaluation of laparoscopic treatment of common bile duct stones in a prospective series of 505 patients: indications and results. Surg Endosc 21:1970–1974
Fogel EL (2003) Endoscopic retrograde cholangiopancreatography topics. Endoscopy 35:913–919
Cheon YK, Lehman GA (2006) Identification of risk factors for stone recurrence after endoscopic treatment of bile duct stones. Eur J Gastroenterol Hepatol 18:461–464
Lauter DM, Froines EJ (2000) Laparoscopic common duct exploration in the management of choledocholithiasis. Am J Surg 179:372–449
Lezoche E, Paganini AM (2000) Technical considerations and laparoscopic bile duct exploration: transcystic and choledochotomy. Semin Laparosc Surg 7:262–278
Cisek PL, Greaney GC (1994) The role of endoscopic retrograde cholangiopancreatography with laparoscopic cholecystectomy in the management of choledocholithiasis. Am Surg 60:772–776
Davis WZ, Cotton PB, Arias R, Williams D, Onken JE (1997) ERCP and sphincterotomy in the context of laparoscopic cholecystectomy: academic and community practice patterns and results. Am J Gastroenterol 92:597–601
Pereira-Lima JC, Rynkowski CB, Rhoden EL (2001) Endoscopic treatment of choledocholithiasis in the era of laparoscopic cholecystectomy: prospective analysis of 386 patients. Hepatogastroenterology 48:1271–1274
Park AE, Mastrangelo MJ Jr (2000) Endoscopic retrograde cholangiopancreatography in the management of choledocholithiasis. Surg Endosc 14:219–226
Soehendra NH (1995) Common areas of interest between interventional biliary radiology and endoscopy. Joachim Burhenne Lecture. AJR Am J Roentgenol 164:547–551
Poulose BK, Speroff T, Holzman MD (2007) Optimizing choledocholithiasis management: a cost-effectiveness analysis. Arch Surg 142:43–48
NIH state-of-the-science statement on endoscopic retrograde cholangiopancreatography (ERCP) for diagnosis and therapy (2002) NIH Consens State Sci Statements 19:1–26. http://consensus.nih.gov
Martin DJ, Vernon DR, Toouli J (2006) Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev 19:CD003327
Esber EJ, Sherman S (2002) The interface of endoscopic retrograde cholangiopancreatography and laparoscopic cholecystectomy. Ann Surg 236:696–697
Gigot JF (1998) Current diagnostic and therapeutic approach to common bile duct calculi: a rapidly evolving field. Ann Chir 52:161–165
Mah D, Wales P, Njere I, Kortan P, Masiakos P, Kim PC (2004) Management of suspected bile duct stones in children: role of selective intraoperative cholangiogram and endoscopic retrograde cholangiopancreatography. J Pediatr Surg 39:808–812
Maetani I, Hoshi H, Ohashi S, Yoshioka H, Sakai Y (1993) Cholangioscopic extraction of intrahepatic stones associated with biliary strictures using a rendezvous technique. Endoscopy 25:303–306
Huntington TR, Bohlman TW (1997) Laparoscopic biliary guidewire: a simplified approach to choledocholithiasis. Gastrointest Endosc 45:295–297
Calvo MM, Bujanda L, Heras I, Cabriada JL, Bernal A, Orive V, Miguelez J (2001) The rendezvous technique for the treatment of choledocholithiasis. Gastrointest Endosc 54:511–513
Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ, Lande JD, Pheley AM (1996) Complications of endoscopic biliary sphincterotomy. N Engl J Med 335:909–918
Paul A, Millat B, Holthausen U, Sauerland S, Neugebauer EA, Berthou JC, Brambs H, Dominguez-Munoz JE, Goh P, Hammerstrom LE, Lezoche E, Perissat J, Rossi P, Rothlin MA, Russell RC, Spinelli P, Tekant Y (2006) The EAES Clinical Practice Guidelines on diagnosis and treatment of Common Bile Duct Stones (1998). In: Neugebauer E, Sauerland S, Fingerhut A, Millat B, Buess G (eds) EAES Guidelines for Endoscopic Surgery–Twelve Years Evidence-Based Surgery in Europe. Springer, Berlin, pp 311–328
Treckman J, Sauerland S, Frilling A, Paul A (2006) Common bile duct stones–Update 2006. In: Neugebauer E, Sauerland S, Fingerhut A, Millat B, Buess G (eds) EAES Guidelines for Endoscopic Surgery–Twelve Years Evidence-based Surgery in Europe. Springer, Berlin, pp 329–333
Gagner M (2008) Rendezvous technique versus endoscopic retrograde cholangiopancreatography to treat bile duct stones reduces endoscopic time and pancreatic damage. J Laparoendosc Adv Surg Tech A 18:113
Disclosure
Drs. Gaetano La Greca, Francesco Barbagallo, Maria Sofia, Saverio Latteri, and Domenico Russello have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
La Greca, G., Barbagallo, F., Sofia, M. et al. Simultaneous laparoendoscopic rendezvous for the treatment of cholecystocholedocholithiasis. Surg Endosc 24, 769–780 (2010). https://doi.org/10.1007/s00464-009-0680-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-009-0680-3