Abstract
Background
Mini gastric bypass (MGB) is a promising and attractive alternative bariatric procedure. In 2011, we introduced MGB in our high-volume bariatric unit. Subsequently, we evaluated short- and midterm results of this procedure.
Methods
A prospective cohort of patients who underwent MGB between 2012 and 2013 was retrospectively evaluated.
Results
From 2012 to 2013, primary MGB was performed in 287 patients with a mean BMI of 42 kg/m2 (range 32–76 kg/m2). The mean operation time was 50 min (range 25–120 min). The mortality rate was 0%. Serious complications, such as leakage, pulmonary embolism, or bleeding, occurred in 3.1% of patients; anastomotic leaks occurred in 1.4% of patients. Conversion to Roux-en-Y gastric bypass for biliary reflux or other indications occurred in six patients (2%). During our initial learning phase, biliary reflux rates were higher due to an overly short pouch. Surgical revision for malnutrition was performed in one patient. Percent excess weight loss and percent total body weight loss were 85 and 35%, respectively, after 1 year; 88 and 36.6%, respectively, after 2 years; and 83 and 34.3%, respectively, after 3 years. Follow-up rates after 1, 2, and 3 years were 96% (277/287), 72% (208/287), and 66% (190/287), respectively.
Conclusions
As a primary bariatric procedure, MGB is associated with good early and midterm results. MGB has the potential to become a significant alternative bariatric procedure. Correct technique is of extreme importance when performing MGB; therefore, the appointment of an experienced MGB surgeon as a guide when beginning to utilize this technique is advised.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Obesity is one of the greatest global health problems, with over 600 million obese adults worldwide [1].
For morbid obesity, bariatric surgery remains the most effective treatment; this approach results in significant sustained weight loss, reduced co-morbidity, and improved survival [2,3,4,5,6,7].
Various surgical procedures are currently available and are usually performed laparoscopically by bariatric surgeons around the world. Currently, the most frequently performed procedures appear to be Roux-en-Y gastric bypass (RYGB) and laparoscopic sleeve gastrectomy (LSG) [8].
In the continuous search for improved surgical treatment, with the objective of optimizing safety, efficacy, durability, and quality of life, mini gastric bypass (MGB) and one-anastomosis gastric bypass (OAGB), appear to be attractive alternative procedures that are increasing in popularity [9].
Since MGB for morbid obesity was first described by Rutledge in 2001 [10], this technique has been extremely controversial [11,12,13,14] due to fear of biliary reflux and its potential oncological consequences, despite the fact that this fear does not appear to be supported by evidence-based human studies. In studies of the OAGB technique published by Garcia-Caballero [15, 16], anti-reflux adaptations reduced the incidence of symptomatic biliary reflux to an acceptable, extremely low rate (< 1%).
Moreover, MGB appears to have certain attractive characteristics. Two large studies, including one randomized investigation by Lee et al. [17, 18] and a multicenter study by Musella et al. [19], have shown good results for MGB in terms of effectiveness, safety, operation time, and improvement in co-morbidity.
Mini gastric bypass is a simple, feasible operation with a short operation time [20] that is safe to perform in super obese or elderly patients [21, 22]. Furthermore, MGB is easy to revise and reverse [23] and produces good results as a revision operation after failed primary restrictive bariatric surgery [24, 25].
Given the combination of these different aspects of MGB, we introduced this technique in 2011 in the high-volume unit of our institution, the first bariatric center in the Netherlands. In our learning phase, we encountered issues such as biliary reflux that led to a critical review of our technique. Given our experience with RYGB, we concluded that our pouch was overly short and adapted and improved our technique. This article describes our experience with MGB during the phase beyond our initial learning period.
Methods
Data
Mini gastric bypass was first introduced in December 2010, and we adapted our surgical technique in 2011. From January 2012 to December 2013, all patients who underwent bariatric surgery at the Center for Obesity at the Medical Center Leeuwarden were included in a prospective database. For this study, patients who underwent MGB as a primary procedure were selected and retrospectively analyzed. Records for individual patients were completed via data review.
Ethical approval was waived by the local medical research ethics committee (“De Regionale Toetsingscommissie Patiëntgebonden Onderzoek”), which is chaired by Dr. A. Wolthuis, Ph.D., since our work involved a retrospective investigation (RTPO1014; the other members of this committee are listed at http://www.ccmo.nl/nl/erkende-metc-s/regionale-toetsingscommissie-pati-ntgebonden-onderzoek-leeuwarden).
Patients
In accordance with international IFSO guidelines, all patients were between 18 and 65 years of age when MGB was performed. Preoperative assessments of patient eligibility for bariatric surgery included consultation with an endocrinologist, a dietician, and a psychologist to exclude patients with non-adjusted eating patterns or eating disorders. If detected, these issues were addressed and fully treated before surgery was considered.
General advise was given concerning the choice for which bariatric operation: symptoms of GERD were considered as a contraindication for sleeve gastrectomy, diabetic patients were advised (mini) gastric bypass surgery, patients with pre/operative known diaphragmatic hernia were advised to undergo RYGB.
Baseline characteristics were determined and entered into the database.
Surgical technique and perioperative management
Patients were positioned in a supine French position under general anesthesia. Pneumoperitoneum was achieved with help of a veress needle and the use of an optical trocar. Then, the five ports are placed. The liver-hand retractor is used to retract the liver. First, Treitz ligament is located and from this point a 150–250-cm-long biliopancreatic or—afferent limb is measured and brought up to the antrum level to judge if there is tension to be expected on the gastroenterostomy. Most of the times this is not the case and this loop is temporarily fixed in the left lower quadrant of the abdomen on an instrument. Initially, MGB was implemented based on experience with the RYGB technique described by Lonroth [26], with a slightly longer pouch.
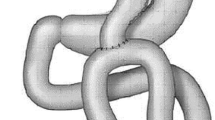
Antecolic–antegastric loop anastomosis or Billroth II gastroenterostomy was performed using a linear stapler. After we performed an interim analysis of our initial results in 2011, our technique was adjusted to create a longer pouch starting at the level of the antrum or crow’s foot, as described by Rutledge [10, 17; Fig. 1]. The linear stapler divides the stomach horizontally at the junction of the corpus and antrum at the level of crow’s foot. An oral calibration tube (34 Fr), is passed by the anesthetist and held against the lesser curvature. The division of the stomach against the tube is completed, with 5–6 lines of staples that seal the gastric pouch. The division of the stomach is parallel to the lesser curvature and up to the angle of His. No short gastric vessels are divided. The jejunal loop is brought up antecolic–antegastric, and the linear stapler is used to anatomose the stomach and the small bowel at this point. The distal end of the gastric tube is anastomosed to the side of the small bowel. The inside of the anastomosis is inspected for bleeding before final closure with a running barbed suture. Finally, a methylene blue leak test is performed to test the anastomosis. Limb length varied from 150 to 250 cm based on the patient’s preoperative BMI. This tailored approach, which was modified from Lee’s recommendations [27], involved a BP limb of 150 cm for patients with BMI < 40, a BP limb of 200 cm for patients with BMI > 40 and < 50, and a BP limb of 250 cm for super obese patients with BMI > 50.
MGB technique [15]
All operations were performed by three experienced bariatric surgeons or occasionally by residents under the strict supervision of an experienced bariatric surgeon.
Postoperative care
All bariatric patients were enrolled in an enhanced recovery program [28] and received 1 year of postoperative PPI therapy to prevent marginal ulcers. Patients were advised to quit smoking prior to undergoing MGB. Preoperative HP analysis was performed using a fecal microbiology test. If this test was positive, eradication treatment was prescribed before surgery. Postoperative daily multivitamin supplements were prescribed.
Patients were put on a fluid diet for 3 weeks beginning on the first postoperative day. Most patients were discharged from the hospital 1–2 days after surgery.
Patients received postoperative counseling by the surgeon at 4 weeks after surgery, at 12 months after surgery, and yearly thereafter. After surgery, all patients were scheduled for a 1.5-year, sequential (monthly) group meeting program that included counseling by a bariatric nurse practitioner, a dietician, a psychologist, and a physiotherapist.
Weight loss
Each patient’s ideal weight was estimated based on a target BMI of 25. Follow-up weight was measured 1 year after surgery. Percent excess weight loss (%EWL) was defined as [(operative weight − follow-up weight)/operative excess weight] × 100.
Co-morbidity
Diabetes remission was defined as the cessation of medication and HbA1c < 42 mmol/mol (6%). Resolution of other co-morbidities was defined as cessation of the use of relevant medications or devices. Improvement was defined as a reduction in the use of relevant medications or devices.
Statistics
All statistical analyses were performed using SPSS (PASW) 18.0 software (SPSS Inc., Chicago, Illinois, USA).
Results
From 2012 to 2013, a cohort of 287 consecutive patients underwent primary MGB.
The median preoperative BMI was 42.7 kg/m2 (± 5.8 kg/m2; range 32–77 kg/m2).
The co-morbidities of diabetes, hypertension, hyperlipidemia, and sleep apnea (treated using a CPAP mask) were preoperatively detected in 67 (23.3%), 119 (41%), 73 (25.4%), and 25 (8.7%) patients, respectively. Other baseline characteristics are shown in Table 1.
There were no significant intraoperative complications. The median operation time for primary MGB was 50 min (range 25–120 min). The median limb length was 200 cm (range 150–250 cm).
No postoperative mortality occurred after surgery. Early complications occurred in 21 patients (6%). Anastomotic leakage occurred in four patients (1.4%); relaparoscopy was needed in two cases involving early leakage, and late leakage was treated conservatively with endoscopic interventions and a feeding tube in two cases. For two patients, relaparoscopy was needed due to bleeding.
Other early complications such as pulmonary embolism and other minor complications are listed in Table 2.
The most common late complication was iron deficiency (16%); oral iron supplements were sufficient treatment for this complication in most cases, but intravenous iron therapy was required in a few cases (4%).
Conversion to RYGB for biliary reflux or other indications was necessary in 14 patients (4.8%) over the course of a 4-year follow-up period.
Conversion due to biliary reflux occurred in six patients (2%). The major other indication for conversion was severe post-prandial abdominal pain, which was believed to be caused by food entering the afferent limb instead of the efferent limb (N = 5).
One patient was converted to RYGB due to insufficient weight loss.
Cholecystectomy was performed in 14 patients (5%). Other late surgical interventions included one reduction of an internal hernia in Petersen’s space and one restoration to normal anatomy due to severe hypoglycemia after MGB.
Furthermore, symptomatic steatorrhea in combination with hypoalbuminemia occurred in 8 (3%) patients; most of these patients were successfully treated with conservative management or pancreatic enzyme replacement therapy (PERT), although one patient required surgical revision. Other late complications are listed in Table 3.
Weight loss
Patients’ median BMI decreased from 42.7 kg/m2 prior to MGB to 27.7 kg/m2 (± 5.1 kg/m2) 1 year after MGB and 27 kg/m2 (± 5 kg/m2) 2 years after MGB but then increased to 28 kg/m2 (± 5.1 kg/m2) 3 years after MGB (Fig. 2). Only one patient required revision for insufficient weight loss.
After 3 years, %EWL was 83.6%, and percent total body weight loss (%TWL) was 34.3%, as shown in Table 4 and Fig. 3.
Follow-up rates after 1, 2 and 3 years were 96% (277/287), 72% (208/287), and 66% (190/287), respectively.
Co-morbidity
Data regarding the development and resolution of co-morbidities are listed in Table 5.
After a median follow-up of 3 years, the resolution of diabetes was seen in 74.6% of patients (50/67), and improvement in diabetes was seen in 24% of patients.
Hypertension was resolved or improved in 70% of patients (83/119); in addition, 3 years after MGB, 64% (16/25) of patients no longer used a CPAP mask or other device for sleep apnea.
Discussion
This article describes our short- and midterm results for implementation of the MGB procedure in a bariatric program. This operation has been rapidly gaining popularity among patients and surgeons since 2012 and is now a commonly performed bariatric operation in our bariatric unit.
One of the key features of this operation is its relative simplicity; due to this simplicity, MGB is a quick procedure, with an average operation time of 50 min for primary operations. Another feature of this procedure is a favorable combination of safety and efficacy. Serious complications or reoperation occurred in approximately 2% of patients, which is comparable to the corresponding rates for other procedures.
When we implemented MGB in 2010, this technique was extremely controversial. This controversy led to a critical review in 2011 of our own results and results reported in the literature. Comparisons of our results with literature findings available at that time revealed a relatively high incidence of biliary reflux after MGB among our patients. This observation led to alterations in our technique (most importantly, the creation of a longer pouch up to the level of the crow’s foot or antrum), which resulted in a lower incidence of biliary reflux. Bile reflux in the gastric pouch is often not symptomatic and should not be harmful. Bile reflux becomes symptomatic when bile acids enter the esophagus, which might occur when the pouch is too short, or occasionally when the patient is in a supine position. We also learned that biliary reflux can be caused by distal obstruction or edema of the gastroenterostomy during the first months after MGB and that avoidance of a supine position during sleep is helpful for treating this temporary complication. The routine use of PPIs does not treat symptoms of biliary reflux but certainly prevents ulcers during the first postoperative year [29] and improves the function of the gastroenterostomy, potentially further decreasing the incidence of biliary reflux.
However, if patients experience ongoing symptoms of unexplained biliary reflux 3 months after their initial diagnosis (with confirmation via upper GI endoscopy) despite conservative management, we advise the conversion of MGB to RYGB or a Braun anastomosis.
After MGB, diarrhea is common but is often not symptomatic. In our cohort, nine patients reported symptomatic, disabling steatorrhea in combination with hypoalbuminemia; most of these patients were treated with conservative management and medications such as PERT. Severe steatorrhea or malnutrition that led to surgical revision only occurred in one patient. These results reflect the safety of our tailored bypass protocol.
In our series, similarly to other large series reported by colleagues who perform MGB [30, 31], excellent weight loss was seen during the first 3 years after surgery, resulting in a satisfactory median BMI of 28 at 3 years after MGB. In addition, satisfactory %EWL and %TWL of 83.6 and 34.3%, respectively, were observed at 3 years after surgery.
During our participation in research by Musella [19], we observed a remission rate for diabetes of 88% during the first year after MGB, based on the American Diabetes Association’s definition of remission [32]. A 74.6% rate of remission of diabetes after a median follow-up of 3 years is promising. Similar results were obtained with respect to the evolution of hypertension and sleep apnea (OSAS).
This study has certain limitations. First, it is a retrospective study of a cohort of patients. Data were retrieved from a prospectively held database, but levels of evidence are nonetheless limited for retrospective studies.
The reported data, with a loss to follow-up rate of 33% after 3 years, are realistic data from a high-volume bariatric practice in the Netherlands.
Although patients from our early experiences with MGB (2010–2011) were excluded from this study, we hope that other surgeons and bariatric teams can learn from our learning curve. Therefore, our advice to all individuals, even experienced bariatric surgeons, who wish to begin implementing this procedure is to use a surgeon with experience with MGB as a guide. For MGB, similar to all other bariatric procedures, the use of appropriate techniques is extremely important for obtaining good results.
Mini gastric bypass and OAGB are extremely potent, promising bariatric procedures that might well be the ideal operations for all morbidly obese patients. At present, indications and patient characteristics associated with MGB being superior to other types of surgery have not been clearly established.
Future randomized clinical trials should focus on this issue and address quality of life and durability.
One of the key features of the MGB procedure is its combination of relative simplicity and efficacy. It also remains an operation that is easy to revise and reverse [33, 34].
Mini gastric bypass has passed beyond being an experimental procedure and has become a serious alternative bariatric procedure [35].
References
World Health Organization (2015) Media centre factsheet N311, obesity and overweight. World Health Organization, Geneva. http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed Jan 2015
Buchwald H, Avidor Y, Braunwald E et al (2004) Bariatric surgery. A systematic review and meta-analysis. JAMA 292:1724–1737
Adams TD, Gress RE, Smith SC et al (2007) Long-term mortality after gastric bypass surgery. N Engl J Med 357:753–761
Sjostrom L, Narbro K, Sjostrom CD et al (2007) Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med 357:741–752
Christou NV, Sampalis JS, Liberman M et al (2004) Surgery decreases long-term mortality, morbidity and health care use in morbidly obese patients. Ann Surg 240:416–424
Flum DR, Dellinger EP (2004) Impact of gastric bypass operation on survival. A population-based analysis. J Am Coll Surg 199:543–555
Pories WJ, Swanson MS, MacDonald KG et al (1995) Who would have thought of it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg 222:339–352
Angrisani L et al (2015) Bariatric surgery worldwide 2013. Obes Surg 25(10):1822–1832. https://doi.org/10.1007/s11695-015-1657-z
Deitel M. Letter (2015) Bariatric surgery worldwide 2013 reveals a rise in mini gastric bypass. Obes Surg 25:2165
Rutledge R (2001) The mini-gastric bypass: experience with first 1,274 cases. Obes Surg 11:276–280
Fisher BL et al (2001) Mini gastric bypass controversy. Obes Surg 11(6):773–777
Mahawar KK, Carr WR, Balupuri S, Small PK (2014) Controversy surrounding ‘mini’ gastric bypass. Obes Surg 24(2):324–333. https://doi.org/10.1007/s11695-013-1090-0 (Review)
Musella M, Milone M (2014) Still “controversies” about the mini gastric bypass? Obes Surg 24:643–644
Mahawar KK, Carr WRJ, Jennings N, Balupuri S, Small PK (2014) Reply to “still controversies after mini gastric bypass”. Obes Surg 24:645–646
Garcia-Caballero M, Carbalo M (2004) One anastomosis gastric bypass: a simple, safe and efficient procedure for treating morbid obesity. Nutr Hosp 19:372–375
Carbajo M, Garcia-Caballero M, Toledano M, Osorio D, Garacia-Lanza C, Carmona JA (2005) One-anastomosis gastric bypass by laparoscopy: results of the first 209 patients. Obes Surg 15:398–404
Lee WJ, Yu PJ, Wang W, Chen TC, Wei PL, Huang MT (2005) Laparoscopic Roux-en-Y versus mini-gastric bypass for the treatment of morbid obesity: a prospective randomized controlled clinical trial. Ann Surg 242:20–28
Lee WJ, Ser KH, Lee YC, Tsou JJ, Chen SC, Chen JC (2012) Laparoscopic Roux-en-Y vs. mini-gastric bypass for the treatment of morbid obesity: a 10-year experience. Obes Surg 22:1827–1834
Musella M, Apers J, Rheinwalt K, Ribeiro R, Manno E, Greco F, Milone M, Di Stefano C, Guler S, Van Lessen IM, Guerra A, Maglio MN, Bonfanti R, Novotna R, Coretti G, Piazza L (2015) Efficacy of bariatric surgery in type 2 diabetes mellitus remission: the role of mini gastric bypass/one anastomosis gastric bypass and sleeve gastrectomy at 1 year of follow-up. A European survey. Obes Surg. https://doi.org/10.1007/s11695-015-1865-6
Rutledge R, Walsh W (2005) Continued excellent results with the mini-gastric bypass: six-year study in 2,410 patients. Obes Surg 15:1304–1308
Peraglie C (2008) Laparoscopic minigastric bypass (LMGB) in the super-super obese: outcomes in 16 patients. Obes Surg 18:1126–1129
Peraglie C (2016) Laparoscopic mini-gastric bypass in patients age 60 and older. Surg Endosc 30:38–43
Lee WJ, Lee YC, Ser KH, Chen SC, Su YH (2011) Revisional surgery for laparoscopic minigastric bypass. Surg Obes Relat Dis 7:486–491
Weiner RA, Theodoridou S, Weiner S (2011) Failure of laparoscopic sleeve gastrectomy—further procedure?. Obes Facts 4(Suppl 1):42–46
Moszkowicz D, Rau C, Guennzi M, Zinzindohoue F, Berger A, Chevallier JM (2013) Laparoscopic omega-loop gastric bypass for the conversion of failed sleeve gastrectomy: early experience. J Vis Surg 150:373–378
Lönroth H (1998) Laparoscopic gastric bypass. Obes Surg 8(6):563–565
Lee WJ, Wang W, Lee YC, Huang MT, Ser KH, Chen JC (2008) Laparoscopic mini-gastric bypass: experience with tailored bypass limb according to body weight. Obes Surg 18:294–299
Bergland A, Gislason H, Raeder J (2008) Fast-track surgery for bariatric laparoscopic gastric bypass with focus on anaesthesia and peri-operative care. Experience with 500 cases. Acta Anaesthesiol Scand 52(10):1394–1399
Coblijn UK, Lagarde SM, de Castro SM, Kuiken SD, van Tets WF, van Wagensveld BA (2016) The influence of prophylactic proton pump inhibitor treatment on the development of symptomatic marginal ulceration in Roux-en-Y gastric bypass patients: a historic cohort study. Surg Obes Relat Dis 12(2):246–252. https://doi.org/10.1016/j.soard.2015.04.022
Kular KS, Manchanda N, Rutledge R (2014) A 6-year experience with 1,054 mini-gastric bypasses—first study from Indian subcontinent. Obes Surg 24:143
Chevallier JM, Arman GA, Guenzi M, Rau C, Bruzzi M, Beaupel N, Zinzindohoué F, Berger A (2015) One thousand single anastomosis (omega loop) gastric bypasses to treat morbid obesity in a 7-year period: outcomes show few complications and good efficacy. Obes Surg 25:951–958
American Diabetes Association (2012) Standards of medical care in diabetes 2012. Diabetes Care 35:S11–S63
Noun R, Skaff J, Riachi E, Daher R, Antoun NA, Nasr M (2012) One thousand consecutive mini-gastric bypass: short and long-term outcome. Obes Surg 22:697–703
Facchiano E, Leuratti L, Veltri M, Lucchese M (2016) Laparoscopic conversion of one anastomosis gastric bypass to Roux-en-Y gastric bypass for chronic bile reflux. Obes Surg. https://doi.org/10.1007/s11695-015-2017-8
Deitel M (2013) Mini-gastric (one-anastomosis) bypass becoming a mainstream operation. In: Bariatr News issue 18, p 13
Acknowledgements
We would like to thank Dr. M. Dunkelgrun for his contributions to this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
J. Apers, R. Wijkmans, M. Emous, and E. Totte have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Apers, J., Wijkmans, R., Totte, E. et al. Implementation of mini gastric bypass in the Netherlands: early and midterm results from a high-volume unit. Surg Endosc 32, 3949–3955 (2018). https://doi.org/10.1007/s00464-018-6136-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6136-x