Abstract
Background
Laparoscopic single anastomosis (mini-)gastric bypass (LSAGB) has been validated as a safe and effective treatment for morbid obesity. However, data of the long-term outcome remain lacking.
Methods
Between October 2001 and December 2015, 1731 morbidly obese patients who received LSAGB as primary bariatric procedure at the Min-Sheng General Hospital were recruited. Surgical outcome, weight loss, resolution of comorbidities, and late complications were followed, then compared with groups of laparoscopic Roux-en-Y gastric bypass (LRYGB) and laparoscopic sleeve gastrectomy (LSG). All data derived from a prospective bariatric database and a retrospective analysis were conducted.
Results
The average patient age was 33.8 ± 10.4 years with a mean body mass index (BMI) of 40.4 ± 7.7 kg/m2. Of them, 70.0% were female while 30.0% were male. Mean operating time, intraoperative blood, and hospital stay of LSAGB were 124.6 ± 38.8 min, 39.5 ± 38.7 ml, and 5.0 ± 4.1 days, respectively. The 30-day post-operative major complication occurred in 30 (1.7%) of LSAGB patients, 16 (2.0%) of LRYGB, and 15 (1.4%) of LSG patients. The follow-up rates at 1, 5, and 10 years were 89.3, 52.1, and 43.6%, respectively. At postoperative 1, 5, and 10 years, the mean percentage of weight loss (%WL) of LSAGB patients were 32.7, 32.2, and 29.1%, and mean BMI became 27, 26.9, and 27 kg/m2, respectively. The LSAGB had a higher weight loss than LRYGB and LSG at 2–6 years after surgery. LSG had a lower remission rate in dyslipidemia comparing to LSAGB and LRYGB. The overall revision rate of LSAGB is 4.0% (70/1731) which was lower than the 5.1% in LRYGB and 5.2% in the LSG.
Conclusion
LSAGB is an effective procedure for treating morbid obesity and metabolic disorders, which results in sustained weight loss and a high resolution of comorbidities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Obesity and its related metabolic disorders are becoming a global epidemic and surgical treatment remained to be the most important treatment method of its extreme, morbid obesity [1, 2]. Surgical treatment for morbid obesity has witnessed a significant increase in the volume since the advent of laparoscopic surgery [3]. However, the procedure of bariatric surgery still evolves and numerous procedures with a plethora of variations are presently advocated as the method of choice to treat morbid obesity [4]. According to the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) survey in 2013, among 468,609 bariatric procedures performed worldwide, the most commonly performed procedure was Roux-en-Y gastric bypass (RYGB) (45%), followed by sleeve gastrectomy (SG) (37%) and laparoscopic adjustable gastric banding (LAGB) (10%) [5]. Regional differences existed in the types of procedures performed. For example, in the North American chapter, SG was the most common (38%), on the other hand, in the European chapter, RYGB was still the most common (43%). In the Asia–Pacific chapter, 49% was SG, followed by RYGB (25%). Other procedures, such as Laparoscopic Mini-Gastric Bypass (MGB) and Bilio-Pancreatic Diversion/Duodenal Switch (BPD–DS) consisted about 1.5 and 2.2% [4].
MGB was first introduced by Dr. Robert Rutledge [6]. The procedure employs a long, narrow sleeve, gastric tube in conjunction with an ante-colic loop gastrojejunal anastomosis. The procedure has the technical advantages of using a tension-free gastrojejunal anastomosis, and of avoiding a R-Y limb construction and its potential complications [7]. Many studies have contributed significant knowledge to the LMGB was regarded to be an equivalent or even better weight loss than RYGB and SG [8,9,10]. Although, MGB outcomes have been addressed by many publication controversies raised by a group of surgeons continues [11]. Their concerns focused on the expectation of bile reflux with symptomatic gastritis and esophagitis requiring revision surgery, increased marginal ulceration, and increased risk of gastric cancer due to chronic alkaline bile reflux which all remain unproven yet. Single anastomosis gastric bypass (SAGB), therefore was proposed by IFSO to replace the MGB and avoid the controversies [12]. However, there was no long-term report (more than 10 years) of LSAGB up to now. Because obesity is a chronic disease, any weight reduction surgery should be shown to be durable before it can be accepted to be effective. Therefore, this study aims to further investigate the long-term (10–15) year’s result of LSAGB, and compare it with other commonly performed bariatric procedures (LRYGB and LSG) in our program.
Methods
Study design and patients
We performed a retrospective review of patients who underwent LSAGB between October 2001 and December 2015 at Min-Sheng General Hospital, Taoyuan, Taiwan. Preoperative assessment in the form of history, physical examination, laboratory evaluation, and directed specialty consultation was carried out on all patients. All the comorbidities like diabetes, hypertension, hyperlipidemia, asthma, sleep apnea, and osteoarthritis were recorded in the database. Informed consent was taken from all patients. A total of 1731 LSAGB were performed as the primary bariatric procedure and recruited for study. The baseline characteristic, surgical outcome, weight loss, and comorbidity resolutions at follow-up were included in the analysis. Patients’ follow-up was scheduled on the 1st, 3rd, 6th, and 12th months of the first year and then annually. Body weight loss and laboratory evaluation of nutritional status were recorded during every visit. All the follow-up data as well as the preoperative and perioperative data of every bariatric patient in our center were recorded in a prospectively maintained database. Another 1912 morbidly obese patients (805 patients receiving LRYGB and 1107 receiving LSG) were collected historically to compare the operation time, blood loss, day of hospital stay, analgesic usage, postoperative complications, and weight loss results. Effectiveness end points include BMI, percentage of weight loss (%WL), and resolution of obesity-related comorbidities. Safety end points were defined by the 30-day perioperative minor and major complications. Complication was graded according to Clavien–Dindo Classification [13].
We use the following criteria for defining the diagnosis or remission of obesity-related metabolic disorders. Remission of hypertension: blood pressure < 135/85 mmHg, without medication; remission of diabetes mellitus (DM): HbA1c < 6.5%, without medication; remission of hyperuricemia: uric acid < 6.5 mg/dl without medication; remission of dyslipidemia: triglyceride < 150 mg/dl and HDL > 50 mg in female, > 40 mg/dl in male without medication.
Procedures
We started to perform LRYGB and LSAGB from 2001, and LSG 2006. The type of operation is usually co-decided by the patient themselves and the surgeon after several comprehensive seminars with the multi-disciplinary team. Surgical procedures were performed by three senior surgeons (Lee, Chen, and Ser). Collectively, they possess more than 10 years of experience in various types of bariatric/metabolic surgeries following a standardized operative technique.
LSAGB
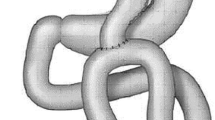
Patients were placed in a gentle reverse Trendelenburg position. Five skin incisions were placed at four sites of the abdomen including: (1) two skin incisions along the nature fold of the umbilicus (10-mm port for the video scope and 12-mm port as a working channel); (2) one skin incision at the left lateral abdominal wall for a 5-mm port (working channel); (3) one skin incision at the right lateral abdominal wall for 12-mm port (first assistant); (4) a stab incision at sub-xyphoid level for retraction of left lobe of liver. The gastric fat pad is dissected to expose the E–G junction. A long-sleeved gastric tube about 2 cm wide is created from the antrum distal to the crow’s foot all the way to E–G junction using a 36-Fr-size bougie as a calibration tube. The jejunum is then identified at the ligament of Treitz and measured 150–250 cm distally according to BMI. The whole intestine length was measured to make sure that the common channel was more than four meters. Antecolic Billroth type 2 side–side gastrojejunostomy was performed using a stapling technique. The gastroenteric defect is then closed by hand-sewn technique over 18F nasogastric tube placed into the efferent loop to ensure the patency of the anastomosis. Anchoring the afferent limb with continuous suture higher than the efferent loop to prevent bile reflux was performed (Fig. 1). The efferent limb is then fixed to the antrum to avoid torsion of the loop and functional obstruction of the efferent loop which might cause intractable bile reflux [8, 12].
LRYGB
RY was performed by the antecolic and antegastric route with 100 cm of biliopancreatic limb and 150 cm of alimentary limb. The gastric pouch was approximately 20 cc and the gastrojejunostomy was created by linear stapler with an anastomosis 1–2 cm diameter wide. The same technique was used to construct jejunojejunostomy [8].
LSG
In brief, a vertical gastrectomy was performed by resecting the greater curvature from the distal antrum (4 cm proximal to the pylorus) to the angle of His including the complete fundus, using a 36-Fr-size bougie as a calibration tube. The resected portion of the stomach was extracted from the extended periumbilical trocar site. A running absorbable seromuscular invagination suture was applied to the staple line with calibration tube in the side to prevent hemorrhage and leakage [14, 15].
All statistical analysis was performed using SPSS versus 19.0.0 (SPSS Inc., Chicago, IL., USA). With baseline comparison made using Chi-square tests and two-sample t test. Continuous variables were expressed as mean (standard deviation). The differences in patient characteristics were established with the use of t test for independent samples.
Results
Patient characteristics
There were a total of 3643 patients observed in this study (Table 1). Mean age, preoperative weight, and BMI of LSAGB patients were 33.6 ± 10.4 years, 110.8 ± 25.7 kg, and 40.4 ± 7.7 kg/m2, respectively. There was a female dominance of 70.0%. Across all three bariatric procedures, there was significant difference in patient characteristics. A higher female patient ratio is observed in LSG comparing LRYGB to LSAGB. On average, patients undergoing the LSAGB procedure are younger in age and possessed a greater overall BMI, while LSG patients were found to carry significantly lower BMI (Table 1).
Perioperative outcome
The mean operative time for LSAGB was 124.6 ± 38.8 min with mean blood loss of 39.5 ± 38.7 ml. The operative time of LSAGB is shorter than LRYGB but longer than LSG. The estimated blood loss of LSAGB is significantly less than the other two groups. Mean postoperative flatus passage of LSAGB was 1.7 ± 0.7 days, and the average length of hospital stay was 5.0 ± 4.1 days which was significantly longer than the other two groups (Table 1). Mean total small intestinal length of LSAGB group was 704.2 ± 104.6 and the average bypassed intestinal length was 220.8 ± 60.2 cm.
The overall early postoperative complication rate was 7.3% for LSAGB, including 97(5.6%) minor complications and 30(1.7%) major complications. Twenty out of the thirty had developed leakage at a percentage of 1.15%; however, the risk of leak was highly influenced by the learning curve of the surgeons as most of the leak occurred in the first 897 cases (0.86%), dropped to 0.29% for the subsequent 493 cases. There was no more postoperative leakage for the recent 341 cases in our study (0%). With regard to post-surgical complications, no statistically significant differences were observed between the procedures, 8.6% for LRYGB, and 6.5% for LSG (Table 1). Overall surgical mortality was 0.17% in this series.
Weight loss
The mean follow-up time was 92.8 ± 52.3 and 98.6 ± 52.0 months for LRYGB and LSAGB, 47.1 ± 26.8 months for LSG. The follow-up rate was 89.3% at 1 year and 52.1% at 5 year, similar in all groups. The 10-year follow-up for LSAGB and LRYGB was 43.6%. Our data showed that LSAGB had sustained and durable significant weight loss than RYGB and LSG from 2 to 6 years (Fig. 2). The percentage of weight loss (%WL) at 1, 2, 5, and 10 years were 32.7, 34, 32.2, and 29.1%, respectively. While the maximum weight loss in all the groups was noticed to be obvious in the first 2 years. The percentage of weight loss at 1, 2, 5, and 10 years were 33.4, 28.6, 26.5, and 26.7% for LRYGB and 29.5, 29.7, 28.2, and 26.9% for LSG, respectively. The percentage of excess weight loss (%EWL) at 1, 2, 5, and 10 years were 79.0, 81.1, 80.4, and 70.3% for LSAGB, 71.7, 74.2, 67.8, and 66.40% for LRYGB and 85.2, 92.2, 83.7, and 88.3% for LSG, respectively.
Remission of metabolic disorders
Across all procedures and all metabolic disorders, the improvement of obesity-related comorbidities reached the most optimal effect at 2 years. Across all years, the LSAGB group had the highest remission rates of DM and dyslipidemia. This study showed that 95.1% DM, 87.7% dyslipidemia, 44.4% hypertension, and 76% hyperuricemia were resolved or improved at a period of 5 years. In this study, LSG had similar high efficacy in diabetes remission rate to both bypass procedures. However, the LSG group consistently reported significantly lower values in the treatment of dyslipidemia by comparison to the LSAGB and LRYGB groups (Table 2).
Revision surgery
At follow-up, the overall revision rate for LSAGB was 4.0% (70/1731). The most common cause for revision was malnutrition in 43 patients (2.5% of overall and 61.4% of total revision), followed by intolerance in 14 (0.8% of overall and 20% of total revision) and weight regain in 9 (0.5% of overall and 12.9% of total revision). The type of revision procedure performed was conversion to LSG in 54 (81.8%), to RYGB in 5 (7.6%), to long limb RYGB in 5 (7.6%), and gastric tube plication in 2 (3.0%). In the LSAGB group, no patients underwent revision surgery for internal hernia. Both LRYGB and LSG had a higher overall revision rate than LSAGB but with different revision indications (Table 3). The overall revision rate for LRYGB was 5.1% with the most common cause of internal herniation in 17 (2.1% of overall and 41.5% of total revision), followed by weight regain in 10 (1.2% of overall and 24.4% of total revision) and malnutrition in 6 (0.7% of overall and 14.6% of total revision). The type of revision procedure performed was conversion to LSG in 16 patients, DJB-SG in 3 patients, 1 had BP limb extension and 1 had LAGB adding. Twenty patients had mesentery defect repair or adhesion lysis. The overall revision rate for LSG was 5.2% with the most common cause of reflux esophagitis in 31 (2.8% of overall and 53.4% of total revision) patients, followed by weight regain in 21 (1.9% of overall and 36.2% of total revision). The type of revision procedure performed was conversion to RYGB in 26 patients for reflux esophagitis and weight regain, SAGB and DJB-SG in 11 patients for weight regain, and 21 patients had hiatal hernia repair.
Discussion
Since we published the first randomized controlled trial comparing LSAGB to LRYGB in 2005, LSAGB started to grow slowly outside of the America. Up to now, there are eight centers reported more than 1000 LSAGB series with unanimous good result [10, 12, 16, 17]. This study is the first one to report the long-term (> 10 years) outcome of LSAGB and confirmed that this procedure is a simple, effective, and durable procedure, with non-inferior or better result than the other commonly performed procedures, LRYGB and LSG. At long-term follow-up, LSAGB also had a lower revision rate than the other two procedures.
The most important advantage regarding the long-term complication of SAGB versus RYGB is the avoidance of the complications from intestine obstruction or internal herniation [18]. Internal herniation is a significant complication of LRYGB with an incidence of more than 10% when there is no mesentery closure and around 1–2% with routine closure of mesentery defect [19, 20]. In this study, 2.1% of RYGB patients had internal herniation but none in LSAGB. Another advantage of LSAGB is a better weight loss than both LRYGB and LSG.
The reason why LSAGB had a better weight loss than LRYGB is intriguing. In this series, LSAGB was found to achieve weight loss percentage of 32.2% at 5 years and more than 29% after more than 10 years which is better than the 26.7% of LRYGB. Both LRYGB and LSAGB had a gastric restriction effect, although LRYGB is provided by a tiny gastric pouch and small outlet where LSAGB is provided by the long sleeve tube. Both procedures also had duodenojejunal bypass effect which eliminated the physiologic response of duodenal gut hormone and related enzyme secretion (glucagon, cholecystokinin, and biliopancreatic enzymes). The rapid food transit to distal gut induces a surge of distal gut hormone (GLP-1 and PYY) release can also been observed in both procedures [21, 22]. Therefore, the difference can only be explained by different bypass limb between two procedures. A standard RYGB had a biliopancreatic (BP) limb of 50 cm with a duodenum bypass effect. SAGB has a much longer BP limb, general being 200 cm, a length very close to mal-absorptive procedure. In biliopancreatic diversion, the estimated BP limb is 250 cm (if the total length of intestine is 500 cm) to 350 cm (if the total length of small intestine is 600 cm). Therefore, the better weight loss in SAGB might possibly be derived from the mal-absorptive effect of long BP limb. There are now more evidences showing that a longer BP limb may produce a better weight loss and metabolic effect than short BP limb. A randomized trial had shown a better weight loss and glycemic control comparing a 50 cm BP limb to 150 cm [23]. One study suggested that longer BP limb is important for the effect of revision surgery but not more than 70% [24]. A recent animal study also demonstrated the importance of BP limb for bariatric/metabolic surgery [25]. However, the side-effect of long BP limb is a higher incidence of anemia and oily stool, problems noted to be greater after SAGB comparing with RYGB [22].
The variety of surgical procedures offered for the treatment of morbid obesity and the disagreement between practitioners over the selection of the surgical technique suggests in part that there may be opportunities for improvement of the presently available surgical options [26]. Because of the relative simplicity, good weight result and less long-term nutritional problems, LSG becomes the most commonly performed bariatric/metabolic surgery worldwide within a decade [5]. However, although long-term data are unknown, the known long-term drawback of LSG is the development of GERD [4]. Our experience with LSG showed de novo GERD occurred up to 17% (31/58) in our long-term series [16]. In this study, the long-term revisional rate of LSG is 5.2% and the most important reason for revision is intractable reflux esophagitis. This study also disclosed an inferior metabolic effect of LSG comparing to gastric bypass procedure. The inferior is not only in dyslipidemia but also in diabetes remission in low BMI patients [27, 28].
In fact, the main long-term drawback of LSAGB is the development of nutritional deficiencies, and the most common presentation is in the form of anemia as demonstrated in this study at a rate of 34.3%. This drop has been found to be related to iron and vitamin B12 deficiencies which results from duodenum and proximal jejunum exclusion, decreased gastric acidity, and modified diet [8]. Although protein malnutrition is not a recognized complication associated with LSAGB in the present study, some patients did require revision surgery because of hypoalbuminemia.
This study has some limitations. Although all data were prospectively collected, the level of evidence provided may not be as strong as that of other well designed studies like randomized control trials. Another limitation of this study is the relative low follow-up rate which is a common problem in bariatric surgery. However, a relatively large numbers and long-term follow-ups still can provide valuable knowledge to help in clinical practice and design the future study.
In conclusion, the present study of LSAGB shows that this procedure is a safe and durable primary bariatric procedure with overall 29.1% WL at 10 years and satisfactory resolution of obesity-related comorbidities. The need for revision of LSAGB (4.0%) is lower than LRYGB and LSG. The revision is indicated mainly for anemia or protein malnutrition.
References
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, Schoelles K (2004) Bariatric surgery: a systematic review and meta-analysis. JAMA 292:1724–1737
Sjöström L, Narbro K, Sjöström CD, Karason K, Larsson B, Wedel H, Lystig T, Sullivan M, Bouchard C, Carlsson B, Bengtson C, Dahlgren S, Gummesson A, Jacobson P, Karlsson J, Lindroos AK, Lonroth H, Naslund I, Olbers T, Stenlof K, Torgerson J, Agren G, Carlsson L (2007) Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med 357:741–752
Buchwald H, Oien DM (2013) Metabolic/bariatric surgery worldwide 2011. Obes Surg 23(4):427–436
Himpens J, Dobbeleir J, Peeters G (2010) Long-term results of laparoscopic sleeve gastrectomy for obesity. Ann Surg 252:319–324
Angrisani L, Santonicola A, Iovino P, Formisano G, Buchwald H, Scopinaro N (2015) Bariatric surgery worldwide 2013. Obes Surg 25:1822–1832
Rutledge R (2001) The mini-gastric bypass: experience with the first 1,274 cases. Obes Surg 11(3):276–280. https://doi.org/10.1381/096089201321336584
Noun R, Skaff J, Riachi E, Daher R, Antoun N, Nasr M (2012) One thousand consecutive mini-gastric bypass: short- and long-term outcome. Obes Surg 22:697–703
Lee WJ, Yu PJ, Wang W, Huang MT (2005) Laparoscopic Roux-en-Y versus mini-gastric bypass for the treatment of morbid obesity. Ann Surg 242:20–28
Tacchino RM, Greco F, Matera D, Diflumeri G (2010) Single-incision laparoscopic gastric bypass for morbid obesity. Obes Surg 20:1154–1160
Bruzzi M, Rau C, Voron T, Guenzi M, Berqer A, Chevallier JM (2015) Single anastomosis or mini-gastric bypass: long-term results and quality of life after a 5-year follow-up. Surg Obes Relat Dis 11:321–326
Fisher BL, Buchwald H, Clark W et al (2001) Mini-gastric bypass controversy. Obes Surg 11(6):773–777
Lee WJ, Lin YH (2014) Single-anastomosis gastric bypass (SAGB): appraisal of clinical evidence. Obes Surg 24:1749–1756
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Ser KH, Lee WJ, Lee YC, Chen JC, Su YH, Chen SC (2010) Experience in laparoscopic sleeve gastrectomy for morbidly obese Taiwanese: staple-line reinforcement is important for preventing leakage. Surg Endosc 24(9):2253–2259
Pok EH, Lee WJ, Ser KH, Chen JC, Chen SC, Tsou JJ, Chin KF (2016) Laparoscopic sleeve gastrectomy in Asia: long term outcome and revisional surgery. Asian J Surg 39:21–28
Jammu G, Sharma R (2016) A 7-year clinical audit of 1107 cases comparing sleeve gastrectomy, Roux-en-Y gastric bypass and mini-gastric bypass, to determine an effective and safe bariatric and metabolic procedure. Obes Surg 26:926–932
Genser L, Carandina S, Tabbara M, Torcivia A, Soprani A, Siksik JM, Cady J (2016) Presentation and surgical management of leaks after mini-gastric bypass for morbid obesity. Surg Obes Relat Dis 12:305–312
Lee WJ, Ser KH, Lee YC, Tsou JJ, Chen SC, Chen JC (2012) Laparoscopic Roux-en-Y vs. mini-gastric bypass for the treatment of morbid obesity: a 10-year experience. Obes Surg 27:623–631
Paroz A, Calmes JM, Giusti V, Suter M (2006) Internal hernia after laparoscopic Roux-en-Y gastric bypass for morbid obesity: a continuous challenge in bariatric surgery. Obes Surg 16:1482–1487
Chowbey P, Baijal M, Kantharia N, Khullar R, Sharma A, Soni V (2016) Mesenteric defect closure decreases the incidence of internal hernias following laparoscopic Roux-en-Y gastric bypass: a retrospective cohort study. Obes Surg 26:2029–2034
Koner J, Inabnet W, Febres G, Conwell I, McMahon D, Salas R, Taveras C, Schrope B, Bessler M (2009) Prospective study of gut hormone and metabolic changes after adjustable gastric banding and Roux-en-Y gastric bypass. Int J Obes 33:786–793
Lee WJ, Chen CY, Chong K, Lee YC, Chen SC, Lee SD (2011) Changes in postprandial gut hormones after metabolic surgery: a comparison of gastric bypass and sleeve gastrectomy. Surg Obes Relat Dis 7:683–690
Venciauskas L, Johannes S, Emst A et al (2014) Short vs. long biliopancreatic limb gastric bypass for treatment of T2DM, randomized controlled study. Obes Surg 24:1149–1150
Caruana JA, Monte SV, Jacobs DM, Voytovich C, Ghanim H, Dandona P (2015) Distal small bowel bypass for weight regain after gastric bypass: safety and efficacy threshold occurs at < 70% bypass. Surg Obes Relat Dis 11:1248–1256
Miyachi T, Nagao M, Shikashi S, Kitahara Y, Tanaka N, Watanabe K, Tsuchiya T, Motoi F, Naitoh T, Unno M (2016) Biliopancreatic limb plays an important role in metabolic improvement after duodenal-jejunal bypass in a rat model of diabetes. Surgery 159(5):1360–1371
Flum DR, Dellinger P (2004) Impact of gastric bypass operation on survival: a population-based analysis. J Am Coll Surg 199:543–551
Lee WJ, Chong K, Ser KH, Lee YC, Chen SC, Chen JC, Tsai MH, Chung LM (2011) Gastric bypass vs sleeve gastrectomy for type 2 diabetes mellitus: a randomized controlled trial. Arch Surg 146(2):143–148
Schauer PR, Kashyap SR, Wolski K, Brethauer SA, Kirwan JP, Pothier CE, Thomas S, Abood B, Nissen SE, Bhatt DL (2012) Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med 366(17):1567–1576
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Narwaf Alkhalifah, Dr. Wei-Jei Lee, Dr. Tan Chun Hai, Dr. Kong-Han Ser, Dr. Jung-Chieh Chen, Dr. Chun-Chi Wu have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Alkhalifah, N., Lee, WJ., Hai, T.C. et al. 15-year experience of laparoscopic single anastomosis (mini-)gastric bypass: comparison with other bariatric procedures. Surg Endosc 32, 3024–3031 (2018). https://doi.org/10.1007/s00464-017-6011-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-6011-1