Abstract
Background
Colorectal endoscopic submucosal dissection (ESD) is a widely accepted treatment for colorectal tumors, but is technically more difficult and has a higher risk of complications such as perforation than gastric ESD. Few studies have investigated the factors associated with technical difficulty and perforation in colorectal ESD. This study aimed to evaluate the technical difficulty according to location, and the risk factors for perforation, in colorectal ESD.
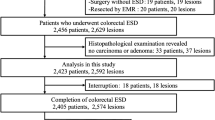
Methods
This retrospective study included 134 consecutive colorectal tumors treated by ESD in 122 patients at the Division of Endoscopy of Hokkaido University Hospital and the Department of Gastroenterology of Kitami Red Cross Hospital from November 2011 to February 2013. To evaluate the technical difficulty of performing ESD for colorectal tumors at specific locations, the en bloc R0 resection rate, specimen diameter, procedure speed, and procedure time were compared among tumor locations using the χ 2 test or analysis of variance. Risk factors for perforation were identified by multiple logistic regression analysis.
Results
The en bloc R0 resection rate was 86.6 % (116/134), the mean tumor diameter was 27.1 mm, and the mean procedure time was 63.5 min. The mean speed of procedures was significantly slower in the sigmoid colon (24.7 min/cm2) than in other areas. Perforation occurred in nine cases (6.7 %). Submucosal fibrosis was the only factor independently associated with perforation (odds ratio 5.684, 95 % confidence interval 1.307–24.727).
Conclusions
ESD was slower for sigmoid colon tumors than for tumors in other areas, suggesting that ESD was technically more difficult in the sigmoid colon than in other colorectal areas. Submucosal fibrosis was independently associated with perforation during colorectal ESD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Endoscopic submucosal dissection (ESD) for gastrointestinal neoplasms enables en bloc resection with tumor-free margins and is not limited by lesion size or location. ESD also enables detailed histological evaluation of the surgical specimen and accurate judgment of resection margins [1]. Following the use of ESD for the treatment of esophageal and gastric tumors, health insurance funding for the treatment of colorectal tumors by ESD was approved in Japan in April 2012 and has now gained widespread acceptance. As en bloc R0 resection of colorectal tumors by ESD is associated with a lower local recurrence rate than conventional endoscopic mucosal resection including piecemeal resection [2–7], ESD may eventually be used as an alternative to endoscopic mucosal resection of colorectal tumors worldwide. Currently, surgical treatment of large rectal tumors may also be performed by transanal resection or transanal endoscopic microsurgery (TEM). ESD has been reported to achieve a higher en bloc R0 resection rate and lower recurrence rate than transanal resection. Although ESD has also been reported to achieve a lower recurrence rate than TEM, the reported en bloc resection rate was lower for ESD than for TEM [8, 9]. There is an ongoing controversy regarding which of these three procedures will eventually lead to the best outcomes in patients with rectal tumors.
Colorectal ESD is technically difficult because of the anatomical features of the colon such as the thin walls, folds and flexures, and colonic peristalsis. This technical difficulty is likely to be associated with complications, especially perforation. However, no previous studies have reported on technical difficulty according to specific tumor location [10, 11]. Japanese studies reported a perforation rate during colonic ESD ranging from 2.5 to 10.4 % [12–14], which is higher than the reported perforation rate during gastric ESD of 2.4 to 4.5 % [15–18]. Perforation during colorectal ESD is dangerous because of the possibility of subsequent peritonitis. Although several previous studies investigated the risk factors for perforation during colorectal ESD, there is still limited information available regarding specific risk factors [10, 13, 19–21].
The aim of this study was to identify the relationship between specific tumor location and the technical difficulty of the procedure during ESD of colorectal tumors. The risk factors for perforation during ESD of colorectal tumors were also evaluated.
Patients and methods
This study retrospectively reviewed 134 consecutive colorectal tumors treated by ESD in 122 patients at the Division of Endoscopy of Hokkaido University Hospital and the Department of Gastroenterology of Kitami Red Cross Hospital in Japan between November 2009 and February 2013. The study protocol was approved by the ethical review boards of both participating institutions, and all patients provided written informed consent for ESD before treatment.
Indications for ESD
The indications for ESD were as follows: (1) depth of invasion limited to the mucosa or submucosa with a noninvasive pattern on magnification chromoendoscopy, (2) large tumor that was difficult to treat by en bloc endoscopic mucosal resection, and (3) recurrence of a lesion previously treated by endoscopic resection. Some carcinoid tumors were also treated by ESD, but they were not included in this study.
ESD method
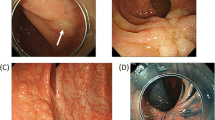
This study included 134 consecutive colorectal tumors that met the indications for ESD in 122 patients. For bowel preparation, each patient drank 2 L of polyethylene glycol solution in the morning before the procedure. ESD was performed under conscious sedation and analgesia. Midazolam (2 mg), diazepam (5 mg), and pentazocine (7.5 mg) were administered intravenously before ESD, and further increments of midazolam (2 mg) or pentazocine (7.5 mg) were given as needed to achieve appropriate sedation. The blood pressure, heart rate, electrocardiograph, and oxygen saturation were monitored during the procedure. Intravenous glucagon or scopolamine was administered to reduce colonic movements. ESD was performed with carbon dioxide insufflation, using a single-channel gastrointestinal endoscope with a transparent attachment hood fitted to the tip (CF-H260AI, GIF-Q260 J; Olympus Optical, Tokyo, Japan, or CF-EC590ZWM; Fujifilm Optical, Tokyo, Japan). The margins of the lesion were delineated before ESD using 0.4 % indigo carmine spray dye. A hyaluronic acid solution was injected into the submucosal layer before mucosal and submucosal cutting. After injection, a circumferential incision was made using a flush knife (Fujifilm Optical) or dual knife (Olympus Optical). Submucosal dissection was then performed using a flush knife, dual knife, or flex knife (Olympus Optical). An ICC 200 electrosurgical generator (Erbe Elektromedizin, Tubingen, Germany) was set to the Endo-Cut mode (Effect 3, 60–80 W) for incision of the mucosa, and to the Endo-Cut mode (Effect 3, 60–80 W) or forced coagulation mode (25–40 W) for incision of the submucosa. Hemorrhage was controlled using hemostatic forceps, such as the Coagrasper (Olympus Optical) in the soft coagulation mode (50 W). All procedures were performed by one of four endoscopists who had each performed more than 100 gastric ESD procedures.
Clinicopathological characteristics
Tumor location was divided into six areas as described by the Japanese Society for Cancer of the Colon and Rectum [22]: rectum, sigmoid colon, descending colon, transverse colon, ascending colon, or cecum. The macroscopic tumor type was classified as protruding tumor (Is), granular-type laterally spreading tumor (Is + IIa, IIa), non-granular-type laterally spreading tumor (IIa, IIc), or residual recurrent tumor [22].
Parameters for analyses
The technical difficulty of ESD was compared among the six colorectal areas by evaluating the en bloc R0 resection rate, tumor diameter, procedure speed, and procedure time for each area. The following factors were included in the analysis of risk factors for perforation during ESD: age, history of laparotomy, mobility of tumor location (mobile: sigmoid or transverse colon; or fixed: rectum, descending colon, ascending colon, or cecum), lesion at a fold or flexure, submucosal fibrosis, resection area, procedure time, procedure speed, and macroscopic type.
The procedure speed was defined as the procedure time per unit area of the resected specimen (min/cm2). The resection area was considered to be approximately oval in shape. En bloc R0 resection was defined as tumor removal in a single piece with tumor-free lateral and vertical margins. Perforation during ESD was defined as the creation of an immediately recognized hole in the bowel wall. Submucosal fibrosis was defined as a slightly white or muscle-like appearance on endoscopy when a hyaluronic acid solution was injected into the submucosal layer.
Histopathological evaluation
All specimens were fixed in 10 % formalin, cut into 2-mm slices, and stained with hematoxylin and eosin. The specimens were examined to determine histological type, depth of invasion, lymphatic invasion, vascular involvement, and lateral and vertical resection margins. Curative resection of adenocarcinoma was defined when all of the following criteria based on the Japanese Classification for Cancer of the Colon and Rectum were met: the lateral and vertical margins were free of tumor, submucosal invasion was <1,000 μm from the muscularis mucosa, and there was no lymphatic invasion, vascular involvement, or poorly differentiated component [22]. One pathologist made all the histological diagnoses at the time of resection.
Statistical analysis
Factors associated with technical difficulty were analyzed using the χ 2 test, Fisher’s exact test, or analysis of variance, as appropriate. Risk factors for perforation were determined using a logistic regression model. All risk factors were analyzed by univariate logistic regression analysis, and factors with a p value <0.1 were included in the multiple logistic regression model. A p value <0.05 was considered to indicate statistical significance in the multiple logistic regression analysis. All analyses were performed using SPSS version 21 (SPSS Japan Inc., Tokyo, Japan).
Results
Clinicopathological characteristics
The patients were 72 males and 50 females with a mean age of 67.9 ± 11.2 (range 38–91) years. The most common tumor location was the rectum (38.1 %). The mean tumor diameter was 27.1 ± 13.3 mm, and the histopathological diagnosis was adenocarcinoma in 78 cases (52.2 %) and adenoma in 56 cases (41.8 %).
Of the adenocarcinomas, 62 (79.5 %) were intramucosal and 16 (20.5 %) were submucosal. Granular-type laterally spreading tumors were the most common macroscopic type (79 cases, 59.0 %) (Table 1). In 16 cases of adenocarcinoma, the resection was judged to be non-curative because of massive submucosal invasion, lymphatic invasion, vascular involvement, positive resection margins, or piecemeal resection. Four of these patients underwent surgical resection with lymphadenectomy immediately after colorectal ESD; these patients had no lymph node metastasis. Another one of these patients underwent additional argon plasma coagulation. Among the remaining 11 patients who underwent non-curative resection by colorectal ESD without immediate surgery, local recurrence occurred in one patient after 29 months. Endoscopic findings indicated massive submucosal invasion of the recurrent lesion, and the patient underwent surgical resection with lymphadenectomy, which achieved curative resection with no evidence of lymph node metastasis. No recurrence has been detected in the remaining 10 patients on careful follow-up (Table 2).
Clinical outcomes of colorectal ESD
The overall en bloc R0 resection rate was 86.6 %, the curative resection rate was 85.1 %, and the mean procedure duration was 63.5 ± 42.6 min. Perforation during ESD occurred in nine cases (6.7 %), and all were successfully treated by endoscopic clipping and administration of intravenous antibiotics, with no need for emergency surgery. There were no cases of discontinuation of ESD owing to intraoperative complications such as perforation or bleeding. There were five cases of postoperative bleeding (3.7 %), which were all successfully treated using endoscopic hemostatic forceps (Table 3).
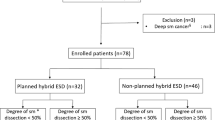
Technical difficulty according to tumor location
The en bloc R0 resection rate, mean tumor diameter, and mean procedure time were not significantly different among the six tumor locations. The mean speed of the procedure was significantly slower in the sigmoid colon than in other areas (p < 0.05) (Table 4).
Risk factors for perforation on univariate and multivariate analysis
Univariate analyses found that perforation was associated with submucosal fibrosis [odds ratio (OR) 6.892; 95 % confidence interval (CI) 1.642–28.937; p = 0.008] and procedure time (OR 1.012; 95 % CI 0.998–1.026; p = 0.089) (Table 5). Multiple logistic regression analysis identified only submucosal fibrosis as an independent risk factor for perforation during colorectal ESD (OR 5.684; 95 % CI 1.307–24.727) (Tables 5, 6).
Discussion
The results of this retrospective study indicate that tumors in the sigmoid colon are technically difficult to treat by ESD. Submucosal fibrosis was a risk factor for perforation during colorectal ESD.
Although previous reports indicated that colorectal ESD is technically difficult, the reasons for this difficulty are unclear. Previous studies reported that the anatomical features of the colon such as the folds and flexures, and the paradoxical movements of the endoscope owing to the flexures, may cause technical difficulty [10, 14, 20, 21]. This study evaluated the technical difficulty of colorectal ESD by comparing outcomes among six colorectal areas. The procedure time per unit area of the specimen (min/cm2) was analyzed to eliminate confounding differences due to tumor size. Our results show that the mean procedure speed was significantly slower in the sigmoid colon (24.7 ± 26.5 min/cm2) than in other areas, suggesting that tumors in the sigmoid colon are technically difficult to treat by ESD compared with tumors in other colorectal areas. Isomoto et al. [20] compared rates of incomplete resection after ESD for tumors of the rectum, left colon, and right colon. They reported that the rate of incomplete resection was highest in the right colon, suggesting that ESD in this area was technically difficult. The current study conducted a more detailed analysis of a wider range of variables, including tumor diameter, procedure speed, and procedure time in six colorectal areas. We believe that there are two reasons for the relatively slow procedure speed in the sigmoid colon. First, the sigmoid colon is relatively mobile and curved, and it may be difficult to achieve a stable connection between the endoscope and the bowel wall during the procedure. Second, tumors in this area tended to be smaller (16.5 ± 10.3 mm), making it more difficult to move the mucosal flap away from the muscle layer using its own weight [23]. When it is easy to open the mucosal flap, it is relatively easy to dissect the submucosal layer using a transparent attachment hood. Changing the position of the patient may enable the use of gravity to help control the movements of the flap and endoscope. Procedures in the sigmoid colon should be performed with extra care by experienced operators.
Perforation is the most important complication of colorectal ESD, because it may result in peritonitis. Previous studies reported that fibrosis, large tumor size, long procedure duration, an operator inexperienced with colonic ESD, and a right colonic lesion were risk factors for perforation during colorectal ESD [10, 13, 19–21]. Three previous studies reported using multiple logistic regression analysis to evaluate the risk factors for perforation during colorectal ESD [10, 20, 21]. The current study analyzed similar variables (patient, tumor, and procedure related), and also analyzed other parameters such as a history of laparotomy, a mobile tumor area (sigmoid or transverse colon), and a lesion at a fold or flexure that could influence control of the endoscope. Submucosal fibrosis was found to be an independent risk factor for perforation, which is consistent with the results reported by Kim et al. [10], Isomoto et al. [20], and Lee et al. [21]. However, these previous studies also reported that tumor size was a risk factor for perforation, which differs from the results of our study. The procedures in our study were performed between 2009 and 2013 (mainly 2010 or later), and the procedures in the previous studies were performed between 2001 and 2010 (mainly 2010 or earlier). This difference in treatment periods may explain the difference in results regarding the risk associated with tumor size. There are currently many opportunities for education regarding colorectal ESD techniques, including demonstrations of actual procedures, which may result in a faster learning curve and a lower risk of perforation when dissecting large tumors. Submucosal fibrosis was identified as a risk factor in our study as well as the studies by Kim et al. [10] and Isomoto et al. [20]. We are confident that submucosal fibrosis is an important risk factor for perforation, because these studies all analyzed data from procedures performed by endoscopists who were highly experienced in procedures such as gastric ESD [10, 20]. Isomoto et al. [20] also reported that perforation during colorectal ESD was associated with fibrosis, especially when tumor size was >20 mm. Matsumoto et al. [24] investigated the relationship between perforation and the degree of submucosal fibrosis (no fibrosis, mild fibrosis, or severe fibrosis) and reported that the perforation rate was very high when there was severe fibrosis, even when an experienced operator performed ESD. Although forceps biopsy, non-granular-type laterally spreading tumors, large villous tumors, and submucosal invasion are associated with fibrosis, it is difficult to predict the presence of fibrosis before the ESD procedure [24]. Further studies should be conducted to identify the preoperative factors predicting fibrosis in lesions treated by colorectal ESD. Moreover, the indications for ESD for colorectal tumors with fibrosis should take the skill of the endoscopist into consideration.
This study is limited by its retrospective nature and the relatively small number of cases. Prospective studies including larger numbers of patients are needed to confirm our results.
In conclusion, ESD is effective for en bloc R0 resection of colorectal tumors, with a good rate of curative resection. However, ESD for tumors of the sigmoid colon had a slower procedure speed than ESD in other colorectal areas, suggesting that procedures in this area are technically difficult. Submucosal fibrosis was identified as an independent risk factor for perforation during colorectal ESD. These results provide useful information for the selection of suitable lesions for complete resection by ESD, especially for inexperienced operators. Future studies should investigate the preoperative factors predicting fibrosis to further determine the safety of colorectal ESD.
References
Toyonaga T, Man-i M, East JE, Nishino E, Ono W, Hirooka T, Ueda C, Iwata Y, Sugiyama T, Dozaiku T, Hirooka T, Fujita T, Inokuchi H, Azuma T (2013) 1,635 Endoscopic submucosal dissection cases in the esophagus, stomach, and colorectum: complication rates and long-term outcomes. Surg Endosc 27:1000–1008
Hotta K, Saito Y, Matsuda T, Shinohara T, Oyama T (2010) Local recurrence surveillance after endoscopic resection of large colorectal tumors. Dig Endosc 22:S63–S68
Tanaka S, Haruma K, Oka S, Takahashi R, Kunihiro M, Kitadai Y, Yoshihara M, Shimamoto F, Chayama K (2001) Clinicopathologic features and endoscopic treatment of superficially spreading colorectal neoplasms larger than 20 mm. Gastrointest Endosc 54:62–66
Khashab M, Eid E, Rusche M, Rex DK (2009) Incidence and predictors of “late” recurrence after endoscopic piecemeal resection of large sessile adenomas. Gastrointest Endosc 70:344–349
Hurlstone DP, Sanders DS, Cross SS, Adam I, Shorthouse AJ, Brown S, Drew K, Lobo AJ (2004) Colonoscopic resection of lateral spreading tumors: a prospective analysis of endoscopic mucosal resection. Gut 53:1334–1339
Hotta K, Fujii T, Saito Y, Matsuda T (2009) Local recurrence after endoscopic resection of colorectal tumors. Int J Colorectal Dis 24:225–230
Sakamoto T, Matsuda T, Otake Y, Nakajima T, Saito Y (2012) Predictive factors of local recurrence after endoscopic piecemeal mucosal resection. J Gastroenterol 47:635–640
Kiriyama S, Saito Y, Matsuda T, Nakajima T, Mashimo Y, Joeng HK, Moriya Y, Kuwano H (2011) Comparing endoscopic submucosal dissection with transanal resection for non-invasive rectal tumor: a retrospective study. J Gastroenterol Hepatol 26:1028–1033
Arezzo A, Passera R, Saito Y, Sakamoto T, Kobayashi N, Sakamoto N, Yoshida N, Naito Y, Fujishiro M, Niimi K, Ohya T, Ohata K, Okamura S, Iizuka S, Takeuchi Y, Uedo N, Fusaroli P, Bonino MA, Verra M, Morino M (2014) Systematic review and meta-analysis of endoscopic submucosal dissection versus transanal endoscopic microsurgery for large noninvasive rectal lesions. Surg Endosc 28:427–438
Kim ES, Cho KB, Park KS, Lee KI, Jang BK, Chung WJ, Hwang JS (2011) Factors predictive of perforation during endoscopic submucosal dissection for the treatment of colorectal tumors. Endoscopy 43:573–578
Tanaka S, Oka S, Kaneko I, Hirata M, Mouri R, Kanao H, Yoshida S, Chayama K (2007) Endoscopic submucosal dissection for colorectal neoplasia: possibility of standardization. Gastrointest Endosc 66:100–107
Tamai N, Saito Y, Sakamoto T, Nakajima T, Matsuda T, Tajiri H (2012) Safety and efficacy of colorectal endoscopic submucosal dissection in elders: clinical and follow-up outcomes. Int J Colorectal Dis 27:1493–1499
Saito Y, Uraoka T, Yamaguchi Y, Hotta K, Sakamoto N, Ikematsu H, Fukuzawa M, Kobayashi N, Nasu J, Michida T, Yoshida S, Ikehara H, Otake Y, Nakajima T, Matsuda T, Saito D (2010) A prospective, multicenter study of 1111 colorectal endoscopic submucosal dissections (with video). Gastrointest Endosc 72:1217–1225
Yoshida N, Wakabayashi N, Kanemasa K, Sumida Y, Hasegawa D, Inoue K, Morimoto Y, Kashiwa A, Konishi H, Yagi N, Naito Y, Yanagisawa A, Yoshikawa T (2009) Endoscopic submucosal dissection for colorectal tumors: technical difficulties and rate of perforation. Endoscopy 41:758–761
Ohta T, Ishihara R, Uedo N, Takeuchi Y, Nagai K, Matsui F, Kawada N, Yamashina T, Kanzaki H, Hanafusa M, Yamamoto S, Hanaoka N, Higashino K, Iishi H (2012) Factors predicting perforation during endoscopic submucosal dissection for gastric cancer. Gastrointest Endosc 75:1159–1165
Toyokawa T, Inaba T, Omote S, Okamoto A, Miyasaka R, Watanabe K, Izumikawa K, Horii J, Fujita I, Ishikawa S, Morikawa T, Murakami T, Tomoda J (2012) Risk factors for perforation and delayed bleeding associated with endoscopic submucosal dissection for early gastric neoplasms: analysis of 1123 lesions. J Gastroenterol Hepatol 27:907–912
Isomoto H, Shikuwa S, Yamaguchi N, Fukuda E, Ikeda K, Nishiyama H, Ohnita K, Mizuta Y, Shiozawa J, Kohno S (2009) Endoscopic submucosal dissection for early gastric cancer: a large-scale feasibility study. Gut 58:331–336
Oda I, Saito D, Tada M, Iishi H, Tanabe S, Oyama T, Doi T, Otani T, Fujisaki J, Ajioka Y, Hamada T, Inoue H, Gotoda T, Yoshida S (2006) A multicenter retrospective study of endoscopic resection for early gastric cancer. Gastric Cancer 9:262–270
Yoon JY, Kim JH, Lee JY, Hong SN, Lee SY, Sung IK, Park HS, Shim CS, Han HS (2013) Clinical outcomes for patients with perforations during endoscopic submucosal dissection of laterally spreading tumors of the colorectum. Surg Endosc 27:487–493
Isomoto H, Nishiyama H, Yamaguchi N, Fukuda E, Ishii H, Ikeda K, Ohnita K, Nakao S, Shikuwa S (2009) Clinicopathological factors associated with clinical outcomes of endoscopic submucosal dissection for colorectal epithelial neoplasms. Endoscopy 41:679–683
Lee EJ, Lee JB, Choi YS, Lee SH, Lee DH, Kim do S, Youk EG (2012) Clinical risk factors for perforation during endoscopic submucosal dissection (ESD) for large-sized, nonpedunculated colorectal tumors. Surg Endosc 26:1587–1594
Japanese Society for Cancer of the Colon and Rectum. Tokyo: Kanehara and Co., Ltd.; 2009
Toyonaga T, Man-i M, Fujita T, East JE, Nishino E, Ono W, Morita Y, Sanuki T, Yoshida M, Kutsumi H, Inokuchi H, Azuma T (2010) Retrospective study of technical aspects and complications of endoscopic submucosal dissection for laterally spreading tumors of the colorectum. Endoscopy 42:714–722
Matsumoto A, Tanaka S, Oba S, Kanao H, Oka S, Yoshihara M, Chayama K (2010) Outcome of endoscopic submucosal dissection for colorectal tumors accompanied by fibrosis. Scand J Gastroenterol 45:1329–1337
Disclosures
Drs. Mizushima, Kato, Iwanaga, Sato, Kubo, Ehira, Uebayashi, Ono, Nakagawa, Mabe, Shimizu, and Sakamoto have no conflict of interests or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mizushima, T., Kato, M., Iwanaga, I. et al. Technical difficulty according to location, and risk factors for perforation, in endoscopic submucosal dissection of colorectal tumors. Surg Endosc 29, 133–139 (2015). https://doi.org/10.1007/s00464-014-3665-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3665-9