Abstract
Background
Leak is the second most common cause of death after bariatric surgery. The leak rate after laparoscopic sleeve gastrectomy (LSG) ranges between 1.1 and 5.3 %. The aim of the paper is to provide an overview of the current pathogenic and promoting factors of leakage after LSG on the basis of recent literature review and to report the evidence based preventive measures.
Methods
Risk factors and pathogenesis of leakage after LSG were examined based on an extensive review of literature and evidence based analysis of the most recent published studies using Oxford centre for evidence-based medicine, 2011, levels of evidence.
Results
Pathogenesis of leakage after LSG can be attributed to mechanical or ischemic causes. Many factors can predispose to leakage after LSG which are either technically related or patient related. Awareness of these predisposing factors and technical tips may decrease the incidence of leakage.
Conclusions
This review reports factors promoting leak and gives technical recommendations to avoid leak after LSG based on the available evidence and expert consensus which encompasses: (1) use a bougie size ≥40 Fr, EL:1, (2) begin the gastric transection 5–6 cm from the pylorus, EL:2–3, (3) use appropriate cartridge colors from antrum to fundus, EL:1, (4) reinforce the staple line with buttress material, EL:1, (5) follow a proper staple line, (6) remove the crotch staples, EL:4, (7) maintain proper traction on the stomach before firing, (8) stay away from the angle of His at least 1 cm, EL:1, (9) check the bleeding from the staple line, (10) perform an intraoperative methylene blue test, EL:4.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic sleeve gastrectomy (LSG) is currently gaining popularity due to its excellent efficacy in terms of combined restrictive and hormonal effects [1]. The mid-term effectiveness of LSG on excess weight loss (EWL) and on major comorbidities contributed to its recent worldwide success. A recent survey reported 546,368 of LSG performed worldwide with 171,548 new cases in 2013 only, showing a steep increase of 37 % from 2003 to 2013, thus becoming the second most commonly performed bariatric/metabolic procedure in the world [2]. Currently, LSG seems to be the most popular procedure for the treatment of morbid obesity in USA and Europe.
However, all surgeries in risky patients may have complications. Minor surgical complications have an overall incidence of 11 % while major surgical complications such as, bleeding, leakage and gastric stenosis constitute about 5 % in large series [3]. The risk of gastric leakage, which usually occurs at the proximal portion of the staple line, has a reported mean incidence of 2.1 % (1.1–5.3 %) [3]. A gastric leakage was defined as “the leak of luminal contents from a surgical join between two hollow viscera”. It can also be an effluent of gastrointestinal contents through a suture line, which may collect near the anastomosis, or exit through the wall or the drain [4]. Leak is the second most common cause of death after bariatric surgery with an overall reported mortality rate of 0.4 % [5]. The aim here is to overview the current pathogenic and favoring factors of leakage after LSG on the basis of recent literature evidence and to summarize the suitable evidences and preventive measures according to the Oxford centre for evidence-based medicine (2011) evidence levels (EL).
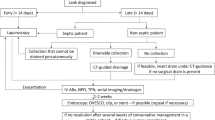
Leak classification
Leakage can be classified based either on the time of onset, clinical presentation, site of leak, radiological appearance, and/or mixed factors. According to the time of onset, Csendes et al. [6] classified leakage as early when appearing within the first four postoperative days, intermediate when appearing in postoperative days 5–9 and late when occurring in or after the tenth postoperative day. By clinical presentation and extent of dissemination, type I or subclinical leakage was defined as well localized leak without dissemination into the pleural or abdominal cavity and without systemic clinical manifestations, and usually they are easy to treat medically. Type II leakage was defined as leak which disseminates into abdominal or pleural cavity, with consequent severe and systemic clinical manifestations (Fig. 1). Based on both clinical and radiological findings, type A leaks are micro-perforations without clinical or radiographic evidence of leak, while type B are leaks detected by radiological studies but without any clinical finding, and finally, type C are leaks presenting with both radiological and clinical evidence [7].
Leaks can result in significant morbidity including sepsis, hemodynamic instability, multi-organ failure, and even mortality in 0–1.4 % of cases [7]. Understanding the correct pathogenesis will help to avoid these complications and to practice all the strategies to reduce it. The proposed pathogenic mechanisms will be discussed.
Causes of leak
Gastric leaks can be due to either mechanical or ischemic causes.
Mechanical aspects
According to Baker et al. [8], stapler misfiring or direct tissue injuries are categorized as “mechanical-tissular” causes and usually appear within 2 days of surgery (early leak). The mechanical factors are usually related to the intrinsic characteristic of the long staple line of LSG. The phenomena of tissue creep, stress relaxation, and shear stress are dependent upon one common factor, which is time. Hence, optimal stapling should allow adequate time for tissue compression and creeping while preventing production of excessive tensile stress. Usually, waiting at least 15 s before firing helps to optimize this concept and allow adequate pre-cut compression time [8].
Optimal stapling is related to proper cartridge choice. The thickness of stomach wall varies, usually decreasing, from pylorus to angle of His (AOH) [9]. Recently, an article published by the “father” of LSG as a definitive procedure [10] showed an interesting and accurate measurement of stomach wall thickness together with a pressure/stress test of suture line related to staple cartridge choice. Authors reported that male patients had a thicker gastric antrum than female patients (3.12 vs. 3.09 mm), while female patients had a thicker gastric wall in the midbody (3.09 vs. 2.57 mm) and proximal areas (1.72 vs. 1.67 mm). These results are similar to these obtained by Elariny et al. [9]. However, maximum fundal thickness reached up to 2.8 mm in females and 2.3 mm in males, and the antrum was as thick as 4.1 mm in females and 5.4 mm in males. Moreover, men had a longer average staple line (22.9 vs. 19.9 cm) [10]. Based on the latter evidence, the proper cartridges selection among the several options offered in the market by the two major brands (Ethicon Echelon™ Stapler-Echelon Flex™ Endopath® Stapler; Ethicon Endo-Surgery, Inc., Cincinnati, OH, USA and Covidien Endo GIA™ Reloads with Tri-Staple™ Technology-Covidien, Dublin, Ireland) is challenging in the absence of routine intraoperative measurement of gastric wall thickness. Under-sizing the staple cartridge increases the risk of inadequate staple formation or can lead to excessive tissue compression, which exceeds the tissue’s tensile strength, leading to tearing and perforation [11].
The appropriate cartridge colors using Stapler-Echelon Flex™ Endopath® Stapler at the antrum, midbody, and fundus of both patient groups (male/female) were black, black, and blue, respectively [10]. On the contrary, with Endo GIA™ Tri-Staple™ at the antrum, midbody, and fundus, the appropriate cartridge colors were black, black, and purple respectively, although the black cartridge for the antrum with this technology results to be completely appropriate in only one out of every six female patients [10].
The new powered staplers, an evolution of the flex staplers, offer greater stability for potentially less tissue trauma by minimizing inadvertent movement at the distal tip in tight spaces and at awkward angles while allowing less movement at the end effector during transection of thick tissues [12].
In absence of international guidelines, the only assumption is that 81 % of the panel experts of the international consensus summit for sleeve gastrectomy believe that “it is not appropriate to use staples with a closed height less than that of a blue load (1.5 mm) on any part of the sleeve gastrectomy” (EL:1) [11]. When using these devices to create a long staple line, the surgeon must search for and remove “migratory crotch staple” (EL:4) [8]. Failure to notice and remove this crotch staple may result in a staple misfire.
Ischemic aspects
Baker identified “ischemic” leaks occurring on the 5th or 6th postoperative day and it was found that most leaks after LSG occur at AOH [8]. Hence most investigations regarding ischemic pathogenesis were focused on this “critical area”. Basso et al. underlined the necessity to staple not so close to gastroesophageal (GE) junction in order to avoid ischemic complications related to the transection of the segmental vascularization of this area [13]. Thereafter, in the international consensus summit for sleeve gastrectomy, 96 % of the panel experts believe that “It is important to stay away from the GE junction on the last firing” (EL:1) [11], but in the same time not much away to avoid leaving residual fundus. Certain groups recommended 1–2 cm as safe distance to avoid stapling too close to the esophagogastric junction and they succeeded in eliminating leaks [14].
In a multicenter experience with 2834 patients, Sakran et al. concluded that leaks after LSG were related to aggressive dissection especially near the posterior aspect of the upper sleeve leading to devascularization and making that area more susceptible to leakage in addition to thermal injuries to the gastric tube by ultrasonic devices (harmonic or ligasure) [15]. Saber et al. published an interesting study about the gastric wall perfusion based on CT scan evaluation [16]. The authors demonstrated that the gastric wall perfusion is significantly decreased at the AOH and gastric fundus compared with perfusion at other gastric points. Gastric perfusion was significantly lower at all the gastric points, particularly at the AOH, among obese patients (33 cases) compared with non-obese patients (18 cases), and this was statistically significant only at the fundus. Gastric perfusion at all the points studied showed a decrease as the BMI increases [16].
On the contrary, a recent prospective study, comparing simple and mesh reinforced hiatoplasty in candidates to LSG reported 0 % of leakage in 96 patients [17]. In this study, the GE junction was completely mobilized and exposed with hiatoplasty in all patients and placement of mesh in 48 patients. These results are antagonistic to the hypothesis of the ischemic aspects of leakage.
Furthermore, in an experimental study by Natoudi et al. [18], the authors measured lactic acid, glycerol, pyruvate levels and lactate/pyruvate (L/P) ratio by microdialysis in GE junction and pylorus before and nine times after LSG in 12 swine. Moreover, air was insufflated inside the tabularized stomach till a rupture of the staple line occurred ex vivo. Surprisingly, when the measured levels of lactic acid, glycerol and the L/P ratio between the GE junction and pylorus were compared, no statistical significances were observed. During the second phase of the experiment, the majority of ruptures (66.6 %) after air insufflation of the tabularized specimen occurred in GE junction, with two cases probably related to staple malfunction. The authors concluded that increased intraluminal pressure and stapling malfunction may play the most important role in fistula formation after LSG [18].
Technical tips
There was an old overall tendency toward more restriction of the final sleeve by using a smaller bougie and leaving a shorter antrum. The conclusions of the 2012 summit on sleeve gastrectomy supported more capacity restriction by using a smaller bougie, with 36 Fr being the most common size used, and by leaving a shorter segment of the pyloric antrum, with 59.5 % of surgeons leaving less than a 5-cm antral pouch [11].
Bougie size
Baltazar et al. used a 32-Fr bougie with transection starting 2–3 cm from the pylorus [19] while, Gagner et al. used a 60-Fr bougie and started the transection at 10 cm away from the pylorus [20]. The bougie size did not affect the mean excess weight loss (EWL) in the short-term studies but weight loss is significantly different in calibrated sleeves compared to non-calibrated sleeves [21]. In the Expert consensus statement in 2012, 87 % of the panelists agreed that it was important to use a bougie to size the sleeve and the optimal size of the bougie should be between 32 to 36 Fr [11]. Using a bougie of <32 Fr may increase the postoperative strictures while a bougie of >36 Fr may bring about limited weight loss effects due to possible dilatation of the sleeve.
A recent meta-analysis of Parikh et al. including 198 leaks in 8922 patients, revealed that the risk of leak decreased with a bougie ≥40 Fr with no difference in %EWL between a bougie <40 Fr and a bougie ≥40 Fr up to 36 months (EL:1) [22]. This strong evidence supports the use of ≥40 Fr bougies to decrease the leak rates without affecting % EWL.
Mid-gastric strictures increase the intragastric sleeve pressure favoring dilation of the upper portion (Fig. 2) and leaks at AOH. Closer staple line to incisura angularis, induced by a narrow bougie size or twisted sleeve due to incorrect staple line orientation, could create different pressure zones similar to the “hourglass model” causing potential leaks in the critical area. The final size of gastric tube and intragastric pressure as well, will also depend on other factors like oversewing the staple line and whether the sutures are snug or lax in relation to the bougie [22]. These factors affect the staple line orientation thus causing twisting and narrowing of the sleeve.
Distance from the pylorus
A recent prospective randomized study by Elgeidie et al. comparing 2 groups depending on the distance at which the gastric division started from the pylorus (Group A with antral preservation and gastric resection starting 6 cm from the pylorus and Group B with antral resection 2 cm from the pylorus), reported higher incidence of leakage with group B (EL:2) [23]. Another retrospective study by Obeidat et al. reported similar results although the group with antral resection was operated after the group of antral preservation (better experience and technique) (EL:3) [24]. This can be attributed to the higher intragastric pressure obtained after antral resection. Increasing the size of the resected antrum might be associated with better short- and mid-term weight loss results but could increase the intragastric pressure which is a risk factor for leakage.
Staple line
Bleeding
Staple line bleeding is considered a direct predisposing factor for leakage after LSG, hematomas over the suture line affect its vascularity and vitality. Bleeding from the staple line (intra- or extraluminal) represents the most frequent complication, up to 9.3 % (mean rate 3.6 %) [25], as the majority of the postoperative events are self-limiting. The re-operation rate for overall complications after LSG ranges 0–10 % [25], with a mean rate of 1.4 % for major bleeding, mainly secondary to staple line bleeding [25, 26]. Modifiable factors should be investigated and corrected before surgery. A direct correlation between smoke and alcohol assumption and postoperative bleeding risk has been demonstrated, particularly if associated with non steroidal anti-inflammatory drugs treatment [27, 28]. Comorbidities, as liver disease (non-alcoholic fatty liver), coagulopathy, hypertension and super-obesity, increased the bleeding risk and should be carefully evaluated and treated pre-operatively when possible. Patients candidate to LSG as revisional procedure, mainly after adjustable gastric band failure/complications, represent a high-risk subset.
The second key point is related to stapling technique. During the last years, several tools have been proposed to reinforce the staple-line and prevent staple line bleeding which includes: oversewing, absorbable synthetic buttress material (synthetic glycolidetrimethylene carbonate copolymer Gore®Seamguard® Bioabsorbable Staple Line Reinforcement), biologic cross-linked buttressing (Bovine pericardium strips, Peri-strips Dry® and PSD Veritas®Baxter), biologic non-cross-linked buttressing (absorbable) (porcine small intestinal submucosa, Surgisis Biodesign®), thrombin matrix (Floseal®, Baxter Healthcare) and fibrin glue (Tisseel, Baxter Healthcare).
The first prospective randomized trial, by Dapri et al. in 2010, comparing three different techniques (no reinforcement, absorbable synthetic buttressing and suture) in 75 patients submitted to LSG demonstrated that staple line buttressing reduces blood loss [29]. Two years later, Gentileschi et al. carried out a prospective randomized trial evaluating three different ways of reinforcement (oversewing, absorbable buttress, thrombin matrix) on 102 patients submitted to LSG and reported similar results [30]. In the same year, Choi in a meta-analysis involving 1335 patients demonstrated that the reinforced LSG had a lower bleeding rate than the non-reinforced group although it was not statistically significant [31]. However, the subgroup analysis demonstrated lower incidence of bleeding than in the non-reinforced group with the use of buttress (OR = 2.2), but higher with suture (OR = 0.2) (EL:1) [31]. Recently, Knapps et al. published a systematic review comparing sleeve gastrectomy performed with or without reinforcement including 4881 patients (without subgroup analysis on the basis of reinforcement). The author did not find any differences between the two groups [32]. The difference with the meta-analysis from Choi can be attributed to the study design and to the lenient selection of papers that did not allow a subgroup analysis. Glaysher et al. published a second review comparing reinforced vs. non-reinforced reporting similar results [33]. D’Ugo et al. reported the results of a multicenter retrospective study including 1162 patients comparing reinforcement (oversewing, Peri-strips Dry, Duet TRS, Seamguard and Floseal) vs. no reinforcement. The authors observed a significant reduction in blood loss and post-operative bleeding incidence with reinforcement [34].
Gagner issued a systematic review about the staple line reinforcement options (no reinforcement, oversewing, non-absorbable bovine pericardial strips (BPS), and absorbable polymer membrane (APM). Leak rates after LSG were 2.6 % (n. 67/2512) in patients without reinforcement, 2 % (n. 86/4128) in patients reinforced with oversewing (suture), 3.3 % (n = 22/643) in patients reinforced with BPS and 1.1 % (n = 16/1446) in patients reinforced with APM, demonstrating that the leak rate of 1.1 % for the APM group was considerably lower than that attained by the three other reinforcement options (all differences significant at p < 0.05) (EL:1) [3]. On the other hand, in 2015, Shikora published a meta-analysis about the same four staple line reinforcement options. Leak rates after LSG were 3.3 % (n = 129/3958) for patients without reinforcement, 2.7 % (n = 166/6141) for patients with oversewing, 1.8 % (n = 31/1678) for patients with BPS and 3.3 % (n = 60/1850) for patients with APM, demonstrating that the leak rate of 1.8 % for the BPS group was significantly lower than that attained by the other three reinforcement options (EL:1) [35]. Both systematic reviews agree that absorbable buttress applied on the adequate cartridges seems to offer a safer and more effective staple line bleeding and leak control at an increased cost (Table 1).
Unfortunately, the staple-line oversewing (cheapest method) did not show any advantage compared with the control group with respect to leak, hemorrhage, and overall complications [3, 35]. In addition, it could lead to stricture of the gastric sleeve and leak through the tears caused by the sutures. As recently published by Rogula et al. [36], the inverting suture (Lambert’s suture) seems to improve the strength and the burst pressure of staple line showing a positive effect on leak occurrence unlike the through to through sutures which are potentially dangerous, but the evaluation was in vitro and in a small number of patients. A recent prospective randomized study comparing two groups of patients who underwent LSG, one group LSG was performed with a running absorbable suture placement at the staple line and in the other group the running suture was not placed, demonstrated more problems after reinforcement of the staple line, such as hematomas. Moreover, dealing with possible leaks and hemorrhage of the staple line was also problematic after placement of the running suture (EL:2) [37].
The use of buttress materials increases surgical costs and cost-effective studies on this particular topic are lacking. Albanopoulos estimated an increased cost of about 1300 € [38], however, Gentileschi reported an extra cost of 580 € [31]. These results when compared with the reduction in terms of re-operation rate for bleeding, days of hospitalization and units of blood for transfusions demonstrated in a large series, increase the attractiveness of the buttress materials, especially synthetic ones, making them potentially cost-effective. The international LSG consensus expert panels reported that reinforcement of LSG staple line is not only a valid option, but it is practiced by the majority of surgeons. Reinforcement may have been historically aimed at leak prevention, but may definitively minimize hemorrhage (100 % of panelist) [11].
Reinforcement
Intragastric pressure has been shown to increase with coughing to as high as 233 mmHg (mean = 37 mmHg) and with vomiting to as high as 290 mmHg (mean = 81 mmHg) [39]. Yehoshua et al. [40] showed that in sleeve gastrectomy, performed on a 50 Fr bougie and reinforced with absorbable running suture, the mean intrasleeve pressure, filled with saline, was 43 mmHg (range: 32–58 mmHg) and that small additional fluid volumes (150 cm3) result in significant elevation of intraluminal pressure (58 mmHg before fluid refluxed into the esophagus). Thus, as patients swallow saliva, the gastric mucosa secretes mucous, the volume/burst/leak pressure ratio of the gastric sleeve staple line may become clinically significant, clarifying the possible relations between postoperative vomiting and leak. Certainly, intrasleeve pressure could affect microcirculation and anastomotic failure.
The evidence of a high pressure system cannot demonstrate the relationship between eventual stenosis, due to a technical error previously described, and gastric leakage. A recent study published by Aydin et al. [41] evaluates the burst pressures of the resected stomach specimens and adverse postoperative events. The authors divided the measurements based on the preferred type of staple line reinforcement; group I: 25 patients, no reinforcement (NoR); group II: 26 patients, fibrin glue (FG) (Tissell; Baxter International, Deerfield, Illinois); group III: 44 patients, suture reinforcement with 2–0 polypropylene sutures (S); and group IV: 14 patients, the biological buttressing material Peri-Strip Dry (PS) (Baxter International). Five postoperative leaks occurred in the reinforcement groups (2 with fibrin glue; 2 with absorbable buttresses and 1 with sutures); no leaks were evident in the no reinforcement group. Suturing afforded the highest burst pressure (mean pressure 74.9 mmHg) and took the longest to perform among the methods but there was no correlation between the leaks and burst pressures. All leaks in the patients were detected in the proximal stomach within 5 cm of the GE junction [41]. In our opinion, the most important bias was the evaluation of burst pressure in the resected stomach which is a structure too much different from the sleeve. The principal rule to avoid overpressure in the sleeve is the critical orientation of the created sleeve, respecting the incisura and the staple line orientation, together with a correct bougie choice, as showed before [42]. The creation of a gastric tube that is not cylindrical in shape results in a high pressure especially at the most proximal corner of the staple line, based on Laplace Law, and thus results in higher chances of leak at the proximal third of the tubular stomach. For example, a spiral shaped staple line can result in functional obstruction of the sleeve, in addition, stapling too close to the incisura can result in anatomical narrowing creating a high pressure system, both are preventable causes of leak that can result in a potentially high pressure system [42]. Avoiding such technical errors which creates an overpressure should be related to experience.
Intraoperative provocative tests
For identifying staple line leak during LSG, provocative intraoperative testing, including methylene blue and/or air leak tests are usually performed. The international sleeve gastrectomy expert panel failed to reach a consensus (48 % consensus) about whether routine intraoperative leak tests should be performed [11]. A recently published study [43] reported that intraoperative leak testing is not correlated with leak due to LSG and is not predictive of the later development of staple line leak, however, it was retrospective study, with unequal groups (1329 vs. 221 patients), operated by different surgeons and different bougies sizes were used. Literature is full of examples of intraoperative positive methylene blue tests with successful management of leak. The routine practice of the intraoperative leak test prevents the serious postoperative consequences that would occur in case of a missed leak (EL:4).
Surgeon related factors
LSG seems to be an easily performed operation, yet is a technically demanding procedure; it has to be learned through proctorship and mentorship. Zacharoulis et al. showed that the experience surely decreased the operative time and hospital stay as opposed to mortality and morbidity rates, conversion rate, and %EWL which were unchanged [44]. Conversely, in 2014, Rebibo et al. [45] evaluated 3 different periods, from 2004 to 2012, on sleeve surgery in a single bariatric centre, showed a decreasing leak rate from 4.6 to 1.9 % in 600 patients. In the same year, based on database evaluation recorded since 2005, 5400 patients were evaluated. The staple line leak rate decreased during the study period from 6.5 to 1.4 % reporting a significant correlation with the operation’s year, more leak at the beginning, and with longer operation time [45]. Noel et al. recently published an interesting retrospective evaluation of 1800 cases [46], primary and revisional LSG, performed by a single centre from 2005 to 2014. The authors dividing the experience in two group, Group A (first 900) and Group B (last 900 LSG), showed a critical decreasing leak rate from 2 to 0.2 %, (p = 0.001) [46]. The leak’s rate improved over time based on the experience of surgeons and based on the adaption of all the evidence published worldwide, which appears strongly related to technical modifiable errors.
Patient-related factors
A recent German multicentric observational study involving 5400 patients with LSG as primary procedure analyzed the risk factors increasing the rate of staple line leakage and reported an association of male gender and BMI between 50 and 59.9 kg/ m2 with significantly higher leakage rate (2.5 vs. 1.6 %; p = 0.02: p < 0.01 respectively) [47]. The presence of at least one comorbidity did not increase the risk of leak in that study (2 vs. 1.3 %; p = 0.24). However, a significant association was only demonstrated for a concomitant sleep apnea (2.6 vs. 1.8 %; p = 0.04) when analyzing each comorbidity separately. In patients with primary laparotomy, the leak rate increased up to 4.4 %. The highest proportion of staple line leaks was demonstrated for procedures with conversion to open approach (14.6 %; p < 0.01) [47].
However, for revisional sleeve gastrectomies as LSG after gastric band and re-sleeve, the risk of leakage is higher due to dense adhesions, scaring and ischemic tissues [48]. For LSG after gastric banding, there is a debate on leak rates between one stage [46] and two stage conversions [49]. A literature review of 15 studies on one-step approach and 8 studies on two-step approach reported a significantly higher leak rate in the one-step group (4.2 %) than in the two-step revisional surgery (1.7 %) [46]. Another recent systematic review and meta-analysis including six studies with 364 patients reported statistically similar leak and fistula rates for one step and two-step LSG [50]. For re-sleeve gastrectomies and fundectomies after LSG, much higher leakage rates were reported ranging from 0 to 14.2 % [51].
Does an ideal sleeve exist?
Till date there are no standard steps for performing LSG. According to our experience and the recently published techniques of expert surgeons, the procedure should start by division of the gastric greater curvature vascular supply starting 5–6 cm from the pylorus and proceeding proximally to the AOH by ultrasound dissection or radiofrequency sealing. The gastroesophageal junction should always be exposed by dissection of the gastroesophageal fat. Good visualization of the AOH with complete mobilization of the gastric fundus should be achieved. The critical steps during the dissection are the left pillar exposure and complete dissection of the fundus to detect any hiatal defect or retroesophageal lipoma.
Subsequently sleeve calibration is performed by inserting a calibrating bougie of ≥40 Fr next to the lesser curvature. The stomach is then transected by linear stapler reinforced by buttress material and a gastric sleeve of 80–100 ml is created. Two sequential black/green cartridges for transection of the antrum 5–6 cm from the pylorus and 1 cm away from the incisura angularis, followed by 2–3 sequential yellow cartridges for the gastric body and fundus when using Echelon Flex™ Endopath® Stapler or 2–3 black cartridges followed by purple cartridges when using Endo GIA™ Tri-Staple™. The last firing should be at least 1 cm away from the gastroesophageal junction. Continuous lateral traction over the stomach should be equal over the anterior and posterior gastric walls to avoid twisted sleeve. An intraoperative methylene blue test is recommended.
Conclusions
This review reports the factors promoting leakage and gives technical recommendations to prevent leakage after LSG based on the available evidence and expert consensus. To summarize, (1) use a bougie size ≥40 Fr, EL:1, (2) begin the gastric transection 5–6 cm from the pylorus, EL:2–3, (3) use appropriate cartridge colors from antrum to fundus, EL:1, (4) reinforce the staple line with buttress material, EL:1, (5) follow a proper staple line, (6) remove the crotch staples, EL:4, (7) maintain proper traction on the stomach before firing, (8) stay away from the AOH at least 1 cm, EL:1, (9) check the bleeding from the staple line, (10) perform an intraoperative methylene blue test, EL:4.
References
Del Genio G, Tolone S, Limongelli P, Brusciano L, D’Alessandro A, Docimo G, Rossetti G, Silecchia G, Iannelli A, Del Genio A, Del Genio F (2014) Sleeve gastrectomy and development of “de novo” gastroesophageal reflux. Obes Surg 24(1):71–77
Angrisani L, Santonicola A, Iovino P, Formisano G, Buchwald H, Scopinaro N (2015) Bariatric surgery worldwide 2013. Obes Surg 25(10):1822–1832
Gagner M, Buchwald JN (2014) Comparison of laparoscopic sleeve gastrectomy leak rates in four staple-line reinforcement options: a systematic review. Surg Obes Relat Dis 10(4):713–723
Peel AL, Taylor EW (1991) Proposed definitions for the audit of postoperative infection: a discussion paper. Surgical infection study group. Ann R Coll Surg Engl 73(6):385
Jurowich C, Thalheimer A, Seyfried F, Fein M, Bender G, Germer CT, Wichelmann C (2011) Gastric leakage after sleeve gastrectomy—clinical presentation and therapeutic options. Langenbeck's Arch Surg 396(7):981–987
Csendes A, Burdiles P, Burgos AM, Maluenda F, Diaz JC (2005) Conservative management of anastomotic leaks after 557 open gastric bypasses. Obes Surg 15(9):1252–1256
Rached AA, Basile M, El Masri H (2014) Gastric leaks post sleeve gastrectomy: review of its prevention and management. World J Gastroenterol 20(38):13904–13910
Baker RS, Foote J, Kemmeter P, Brady R, Vroegop T, Serveld M (2004) The science of stapling and leaks. Obes Surg 14(10):1290–1298
Elariny H, González H, Wang B (2005) Tissue thickness of human stomach measured on excised gastric specimens from obese patients. Surg Technol Int 14:119–124
Huang R, Gagner M (2015) A thickness calibration device is needed to determine staple height and avoid leaks in laparoscopic sleeve gastrectomy. Obes Surg 25(12):2360–2367
Rosenthal RJ, Panel, I.S.G.E (2012) International sleeve gastrectomy expert panel consensus statement: best practice guidelines based on experience of >12,000 cases. Surg Obes Relat Dis 8(1):8–19
Marczyk S, Tyco Healthcare Group Lp (2009) Powered surgical stapling device. U.S. Patent 7,637,409
Basso N, Casella G, Rizzello M, Abbatini F, Soricelli E, Alessandri G, Maglio C, Fantini A (2011) Laparoscopic sleeve gastrectomy as first stage or definitive intent in 300 consecutive cases. Surg Endosc 25(2):444–449
Bellanger DE, Greenway FL (2011) Laparoscopic sleeve gastrectomy, 529 cases without a leak: short-term results and technical considerations. Obes Surg 21(2):146–150
Sakran N, Goitein D, Raziel A, Keidar A, Beglaibter N, Grinbaum R, Matter I, Alfici R, Mahajna A, Waksman I, Shimonov M, Assalia A (2013) Gastric leaks after sleeve gastrectomy: a multicenter experience with 2834 patients. Surg Endosc 27(1):240–245
Saber AA, Azar N, Dekal M, Abdelbaki TN (2015) Computed tomographic scan mapping of gastric wall perfusion and clinical implications. Am J Surg 209(6):999–1006
Ruscio S, Abdelgawad M, Badiali D, Iorio O, Rizzello M, Cavallaro G, Severi C, Silecchia G (2016) Simple versus reinforced cruroplasty in patients submitted to concomitant laparoscopic sleeve gastrectomy: prospective evaluation in a bariatric center of excellence. Surg Endosc 30(6):2374–2381
Natoudi M, Theodorou D, Papalois A, Drymousis P, Alevizos L, Katsaragakis S, Zografos G, Leandros E, Menenakos E (2014) Does tissue ischemia actually contribute to leak after sleeve gastrectomy? An experimental study. Obes Surg 24(5):675–683
Baltasar A, Serra C, Pérez N, Bou R, Bengochea M, Ferri L (2005) Laparoscopic sleeve gastrectomy: a multi-purpose bariatric operation. Obes Surg 15(8):1124–1128
Gagner M, Rogula T (2003) Laparoscopic reoperative sleeve gastrectomy for poor weight loss after biliopancreatic diversion with duodenal switch. Obes Surg 13(4):649–654
Weiner RA, Weiner S, Pomhoff I, Jacobi C, Makarewicz W, Weigand G (2007) Laparoscopic sleeve gastrectomy—influence of sleeve size and resected gastric volume. Obes Surg 17(10):1297–1305
Parikh M, Issa R, McCrillis A, Saunders JK, Ude-Welcome A, Gagner M (2013) Surgical strategies that may decrease leak after laparoscopic sleeve gastrectomy: a systematic review and meta-analysis of 9991 cases. Ann Surg 257(2):231–237
ElGeidie A, ElHemaly M, Hamdy E, El Sorogy M, Abdelgawad M, GadElHak N (2015) The effect of residual gastric antrum size on the outcome of laparoscopic sleeve gastrectomy: a prospective randomized trial. Surg Obes Relat Dis 11(5):997–1003
Obeidat F, Shanti H, Mismar A, Albsoul N, Al-Qudah M (2015) The magnitude of antral resection in laparoscopic sleeve gastrectomy and its relationship to excess weight loss. Obes Surg 25(10):1928–1932
Trastulli S, Desiderio J, Guarino S, Cirocchi R, Scalercio V, Noya G, Parisi A (2013) Laparoscopic sleeve gastrectomy compared with other bariatric surgical procedures: a systematic review of randomized trials. Surg Obes Relat Dis 9(5):816–829
Sarkhosh K, Birch DW, Sharma A, Karmali S (2013) Complications associated with laparoscopic sleeve gastrectomy for morbid obesity: a surgeon's guide. Can J Surg 56(5):347
Tønnesen H, Nielsen PR, Lauritzen JB, Møller AM (2009) Smoking and alcohol intervention before surgery: evidence for best practice. Br J Anaesth 102(3):297–306
Loke YK, Trivedi AN, Singh S (2008) Meta-analysis: gastrointestinal bleeding due to interaction between selective serotonin uptake inhibitors and non-steroidal anti-inflammatory drugs. Aliment Pharmacol Ther 27(1):31–40
Dapri G, Cadière GB, Himpens J (2010) Reinforcing the staple line during laparoscopic sleeve gastrectomy: prospective randomized clinical study comparing three different techniques. Obes Surg 20(4):462–467
Gentileschi P, Camperchioli I, D’Ugo S, Benavoli D, Gaspari AL (2012) Staple-line reinforcement during laparoscopic sleeve gastrectomy using three different techniques: a randomized trial. Surg Endosc 26(9):2623–2629
Choi YY, Bae J, Hur KY, Choi D, Kim YJ (2012) Reinforcing the staple line during laparoscopic sleevegastrectomy: does it have advantages? A meta-analysis. Obes Surg 22(8):1206–1213
Knapps J, Ghanem M, Clements J, Merchant AM (2013) A systematic review of staple-line reinforcement in laparoscopic sleeve gastrectomy. JSLS 17(3):390–399
Glaysher M, Khan OA, Mabvuure NT, Wan A, Reddy M, Vasilikostas G (2013) Staple line reinforcement during laparoscopic sleeve gastrectomy: does it affect clinical outcomes? Int J Surg 11(4):286–289
D’Ugo S, Gentileschi P, Benavoli D, Cerci M, Gaspari A, Berta RD, Moretto C, Bellini R, Basso N, Casella G, Soricelli E (2014) Comparative use of different techniques for leak and bleeding prevention during laparoscopic sleeve gastrectomy: a multicenter study. Surg Obes Relat Dis 10(3):450–454
Shikora SA, Mahoney CB (2015) Clinical benefit of gastric staple line reinforcement (SLR) in gastrointestinal surgery: a meta-analysis. Obes Surg 25(7):1133–1141
Rogula T, Khorgami Z, Bazan M, Mamolea C, Acquafresca P, El-Shazly O, Aminian A, Schauer P (2015) Comparison of reinforcement techniques using suture on staple-line in sleeve gastrectomy. Obes Surg 25(11):2219–2224
Albanopoulos K, Tsamis D, Arapaki A, Kleidi E, Zografos G, Leandros E (2015) Staple line reinforcement with stitch in laparoscopic sleeve gastrectomies. Is it useful or harmful? J Laparoendosc Adv Surg Tech 25(7):561–565
Albanopoulos K, Alevizos L, Flessas J, Menenakos E, Stamou KM, Papailiou J, Natoudi M, Zografos G, Leandros E (2012) Reinforcing the staple line during laparoscopic sleeve gastrectomy: prospective randomized clinical study comparing two different techniques. Preliminary results. Obes Surg 22(1):42–46
Iqbal A, Haider M, Stadlhuber RJ, Karu A, Corkill S, Filipi CJ (2008) A study of intragastric and intravesicular pressure changes during rest, coughing, weight lifting, retching, and vomiting. Surg Endosc 22(12):2571–2575
Yehoshua RT, Eidelman LA, Stein M, Fichman S, Mazor A, Chen J, Bernstine H, Singer P, Dickman R, Shikora SA, Rosenthal RJ (2008) Laparoscopic sleeve gastrectomy—volume and pressure assessment. Obes Surg 18(9):1083–1088
Aydin MT, Aras O, Karip B, Memisoglu K (2015) Staple line reinforcement methods in laparoscopic sleeve gastrectomy: comparison of burst pressures and leaks. JSLS 19(3). doi:10.4293/JSLS.2015.00040
Shabbir A, Teh JL (2014) A new emerging procedure-sleeve gastrectomy. Essentials and controversies in bariatric surgery. InTech. Chapter 5, p 101–124
Sethi M, Zagzag J, Patel K, Magrath M, Somoza E, Parikh MS, Saunders JK, Ude-Welcome A, Schwack BF, Kurian MS, Fielding GA (2015) Intraoperative leak testing has no correlation with leak after laparoscopic sleeve gastrectomy. Surg Endosc 30(3):883–891
Zacharoulis D, Sioka E, Papamargaritis D, Lazoura O, Rountas C, Zachari E, Tzovaras G (2012) Influence of the learning curve on safety and efficiency of laparoscopic sleeve gastrectomy. Obes Surg 22(3):411–415
Rebibo L, Blot C, Verhaeghe P, Cosse C, Dhahri A, Regimbeau JM (2014) Effect of perioperative management on short-term outcomes after sleeve gastrectomy: a 600-patient single-center cohort study. Surg Obes Relat Dis 10(5):853–858
Noel P, Nedelcu M, Gagner M (2015) Impact of the surgical experience on leak rate after laparoscopic sleeve gastrectomy. Obes Surg:1–6. doi:10.1007/s11695-015-2003-1
Benedix F, Benedix DD, Knoll C, Weiner R, Bruns C, Manger T, Stroh C, Obesity Surgery Working Group (2014) Are there risk factors that increase the rate of staple line leakage in patients undergoing primary sleeve gastrectomy for morbid obesity? Obes Surg 24(10):1610–1616
Abdelgawad M, De Angelis F, Iossa A, Rizzello M, Cavallaro G, Silecchia G (2016) Management of complications and outcomes after revisional bariatric surgery: 3-year experience at a bariatric center of excellence. Obes Surg:1–6. doi:10.1007/s11695-016-2071-x
Silecchia G, Rizzello M, De Angelis F, Raparelli L, Greco F, Perrotta N, Lerose MA, Campanile FC (2014) Laparoscopic sleeve gastrectomy as a revisional procedure for failed laparoscopic gastric banding with a “2-step approach”: a multicenter study. Surg Obes Relat Dis 10(4):626–631
Dang JT, Switzer NJ, Wu J, Gill RS, Shi X, Thereaux J, Birch DW, de Gara C, Karmali S (2016) Gastric band removal in revisional bariatric surgery, one-step versus two-step: a systematic review and meta-analysis. Obes Surg 26(4):866–873. doi:10.1007/s11695-016-2082-7
Silecchia G, De Angelis F, Rizzello M, Albanese A, Longo F, Foletto M (2015) Residual fundus or neofundus after laparoscopic sleeve gastrectomy: is fundectomy safe and effective as revision surgery? Surg Endosc 29(10):2899–2903
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals.
Additional information
Angelo Iossa and Mohamed Abdelgawad contributed equally to this work.
Rights and permissions
About this article
Cite this article
Iossa, A., Abdelgawad, M., Watkins, B.M. et al. Leaks after laparoscopic sleeve gastrectomy: overview of pathogenesis and risk factors. Langenbecks Arch Surg 401, 757–766 (2016). https://doi.org/10.1007/s00423-016-1464-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-016-1464-6