Abstract
Introduction
Successful localization is mandatory for focused parathyroidectomy. If ultrasound and sestamibi scan are negative, bilateral neck exploration is necessary. We examined the contribution of complementary computed tomography (CT) scan to identify the affected parathyroid gland.
Methods
Between November 1999 and April 2014, 25 patients (20 females and 5 males; mean age 67 ± 11 years) with negative or dubious standard imaging (ultrasound and sestamibi scan) underwent CT scan prior to parathyroidectomy and were included in this study. Fifteen patients had had previous neck surgery for parathyroidectomy (n = 11) or thyroidectomy (n = 4). Thin-slice CT (n = 9) or four-dimensional (4D) CT imaging (n = 16) was used. Cure was defined as >50 % post-excision fall of intraoperatively measured parathyroid hormone or fall into the normal range, confirmed by normocalcaemia at least 6 months after surgery.
Results
Preoperative CT scan provided correct localization in 13 out of 25 patients (52 %) and was false positive once. Parathyroidectomy was performed by a focused approach in 11 of these 13 patients as well as in 1 patient guided by intraoperatively measured parathyroid hormone (ioPTH). Thirteen patients required bilateral neck exploration. The cure rate was 96 % (24/25 patients). One patient has persistent primary hyperparathyroidism (pHPT) and one a recurrent disease. Six patients presented a multiglandular disease.
Conclusion
A CT scan identifies about half of abnormal parathyroid glands missed by conventional imaging and allows focused surgery in selected cases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Primary hyperparathyroidism (pHPT) is usually caused by a single adenoma (80–85 %) but can also be due to double adenomas (2–5 %), chief cell hyperplasia (15–20 %) or parathyroid carcinoma (<1 %) [1]. Preoperative localization studies are used to plan the operative approach and thereby minimize the extent of surgical dissection. The aim of the localization studies should be to differentiate between solitary adenoma and multiglandular disease as well as to obtain details regarding the anatomical location of the enlarged gland(s), due to the significant embryologic variations in parathyroid anatomy [2]. Knowledge of common and unusual anatomic locations is essential for the operative success during both initial and reoperative parathyroid surgical exploration.
Positive preoperative localization studies are accepted as a precondition for applying minimally invasive surgical techniques. If preoperative localization studies are inconclusive, bilateral neck exploration (BNE) is usually considered as the standard option [3]. BNE allows identifying all parathyroid glands, to detect or exclude the presence of multiglandular disease and remove the abnormal gland(s). Because of the increased risk for morbidity and failure in reoperation, the current consensus calls for two concordant imaging studies localizing the hyperfunctioning parathyroid tissue [4].
Recently, four-dimensional computed tomography (4D CT) has been described as a new option for preoperative localization. It takes advantage of the rapid contrast uptake and washout that is characteristic of parathyroid adenomas, compared to the progressive enhancement pattern of lymph nodes [5, 6]. Four-dimensional CT hereby associates functional and detailed anatomic information [7].
In the present study, we report our experience with preoperative computed tomography. In a setting of failed localization by ultrasound and sestamibi scintigraphy with or without prior surgery, we examined the contribution of complementary non-invasive imaging using either standard thin-slice or 4D CT scan.
Methods
Between November 1999 and April 2014, 926 patients (240 men and 686 women; mean age 57 ± 14 years) underwent surgery for pHPT in our department. Adenomas were localized in 677 patients with either ultrasound alone (n = 179) or concordant findings in ultrasound and sestamibi scintigraphy (n = 498). Twenty-five patients (5 males and 20 females; mean age 67 ± 11 years) with negative or dubious ultrasound and/or sestamibi scintigraphy underwent thin-slice CT scan or 4D CT prior to surgery and therefore met the inclusion criteria of the present study. Nine patients were symptomatic, two had a history of osteopenia or osteoporosis and seven had a history of nephrolithiasis. Baseline patient characteristics are summarized in Table 1. Between 1999 and 2011, preoperative CT was not routinely performed in the case of missing localization. During this period, nine patients were referred to our hospital having undergone thin-slice CT. Since 2012, 16 patients underwent 4D CT at our institution prior to surgery.
Fifteen patients had a history of neck surgery including four thyroidectomies, three parathyroidectomies and eight unsuccessful parathyroid explorations (Table 2).
Imaging technique
Four-dimensional CT imaging was performed on a Brilliance 16-MDCT scanner (Philips Healthcare, Netherlands) using the following parameters: tube voltage of 120 kVp, tube current of 250 mAs, collimation of 16 × 0.75; pitch of 0.938, rotation of 0.75 s, matrix of 512, slice thickness of 2 mm and increment of −1.0 mm. Images were obtained from the maxilla to the tracheal bifurcation after intravenous administration of 120 ml of contrast material (Imeron 300; Bracco) at a rate of 2 ml/s, followed by a bolus of 50 ml of saline. Images were performed pre- and post-contrast after a delay of 25, 50 and 80 s (Fig. 1). Images were reconstructed at 1 mm in thickness overlapping with an increment of −0.5 mm in the axial view. Thin-slice CT scans were performed elsewhere prior and after the administration of iodinated contrast (with different post-contrast delay according to the referral radiologist) with image reconstruction at 1 to 3 mm in thickness.
Surgery
General anaesthesia was used in all cases followed by collection of a baseline sample of intact parathyroid hormone (iPTH) from the peripheral vein. A single post-excision sample was collected 15 min after gland removal for intraoperative PTH analysis (Nichols Institute Diagnostic, San Juan Capistrano, CA, USA; published normal range, 10–65 pg/ml). Patients with a single-gland disease underwent focused parathyroidectomy, while those suspected to have bilateral or multiglandular disease underwent a four-gland exploration. Intraoperative localization was documented in the operative and pathology reports. Cure was defined as >50 % post-excision fall of intraoperatively measured parathyroid hormone (ioPTH) or fall into the normal range. PTH and calcium levels have been confirmed to remain in the normal range 6 months after surgery. All patients underwent a pre- and postoperative direct laryngoscopy to assess the vocal cord function.
Statistical analysis
Continuous variables are expressed as mean ± standard deviation (SD). Between-group differences were assessed by paired t test. Fisher’s exact test was used for categorical data. Significance was accepted for p < 0.05. Statistical analysis was performed using a commercially available program (Prism 5®; GraphPad Software Inc., La Jolla, USA).
Results
Preoperative CT scan showed a suspicious lesion in 14 cases (six by thin-slice CT and eight by 4D CT). A true-positive localization was intraoperatively confirmed in 13 patients (positive predictive value 93 %). In one case, the preoperative thin-slice CT scan showed a false-positive result. We observed a higher sensitivity of preoperative CT in the case of reoperation. Among 15 patients with previous history of neck surgery, 10 patients showed a positive localization by the CT scan (67 %). In the case of primary surgery (10 patients), the sensitivity was 30 %. Nevertheless, the difference was not statistically significant (p = 0.1).
The overall cure rate after surgery was 96 % (24/25 patients). Twenty-one patients were cured at primary exploration. Three patients were cured after reoperation and removal of a mediastinal adenoma (two cases) or extensive resection of a parathyroid carcinoma. The mediastinal adenomas were localized by intraoperative selective venous sampling for PTH in one case and by re-evaluation by means of 11C-methionine positron emission tomography (PET) scan and repeated CT in the other one. One patient with persistent disease and histologically proven parathyroid carcinoma underwent re-exploration and en bloc resection of the ipsilateral thyroid lobe including the lymph nodes of the central compartment. Postoperative PTH dropped to 24 pg/ml. The patient died 3 years after surgery due to pneumonia. The PTH level at this time was 1360 pg/ml, and the recurrent disease was medically controlled with calcimimetics. One patient still suffers from persistent pHPT. An extensive re-evaluation including 11C-methionine positron emission tomography scan of the neck and mediastinum failed to identify any site of positive uptake.
A bilateral exploration was performed in 13 patients (52 %). This was started with the video-assisted technique (MIVAP) in eight patients. A conversion to standard cervicotomy was necessary in four cases. A focused unilateral parathyroidectomy was performed in 12 patients, including 11 with positive preoperative CT scan and 1 case guided by ioPTH measuring. In the suspected multiglandular disease, we performed a four-gland exploration irrespective of CT findings. Therefore, bilateral exploration was performed in 11 patients with negative CT scan and in 2 patients with positive CT scan. Simultaneously, two hemithyroidectomies and two thyroidectomies were carried out (three cases of multinodular goitre and one case of suspected intrathyroidal parathyroid gland).
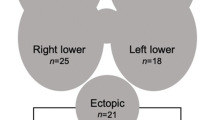
The mean operating time was 87 ± 81 min (range 20–240 min). We found an ectopic localization in five patients (three mediastinal, one intrathyroidal and one laterocervical). Histology showed solitary adenomas in 19 patients and multiglandular disease in 6 patients (two parathyroidectomies following earlier removal of one adenoma, three subtotal parathyroidectomies and one case of hyperplasia of two glands). The mean diameter of the resected gland was 14.2 ± 6 mm (range 7–30 mm). There was no significant difference between the CT-positive group (mean size 14.7 ± 7 mm) and the CT-negative group (mean size 13.5 ± 4 mm) (p = 0.36).
Postoperative complications included one case of transient nerve palsy in a patient with a known non-recurrent inferior laryngeal nerve at third exploration. The laryngoscopy performed 1 year later prior to the fourth surgery (thoracoscopy for mediastinal adenoma) showed normal motility of the vocal cords. Three patients required calcium and vitamin D substitution for transitory hypoparathyroidism. After a mean follow-up of 19.5 months, we observed one case of recurrent disease 2 years after surgery (Table 3).
Discussion
Negative localization in patients with primary hyperparathyroidism entails a negative selection of patients with a high rate of unsuccessful explorations and an increased risk for persistent pHPT [8]. In the Mayo experience, operation was curative in 90.4 % with a negative sestamibi scan compared to a 97.5 % cure rate with localization (p < 0.001). Moreover, a negative scan entailed a higher rate of multiglandular resection (32 vs. 13 %, p < 0.001) [9]. This represents even a risk for postoperative hypoparathyroidism [10].
Therefore, the use of ioPTH should be recommended in negative or discordant imaging in order to decrease the risk of persistent disease and hypocalcaemia. The data of the Scandinavian Quality Register for Thyroid and Parathyroid Surgery support this strategy. Patients who underwent surgery with ioPTH measurement had a lower risk for persistent pHPT than patients without ioPTH (7/79 (9 %) vs. 23/85 patients (27 %), respectively, p = 0.003) [10].
Apart from patients with unclear localization, reoperation for persistent/recurrent disease represents a considerable challenge. For experienced parathyroid surgeons, the success rate of reoperations can be as high as 95 % [4]. Nevertheless, a higher rate of complications should be taken into account. Karakas et al. reported a recurrent laryngeal nerve palsy rate of 9 % and an incidence of permanent hypoparathyroidism ranging between 6 and 9 % [11]. To minimize the extent of exploration and potential complications, a clear localization should be available before reoperation [4].
In the setting of failure of standard imaging procedures, there is a need for additional diagnostic tools to localize parathyroid adenomas preoperatively. Apart from ultrasound and planar or 3D scintigraphy, there is a variety of diagnostic studies to choose from, including regular MRI or CT, 4D CT, CT-methoxyisobutylisonitrile (MIBI) image fusion, PET/CT in combination with 11C-methionine and invasive selective venous sampling [12, 13].
Novel localization techniques, such as CT-MIBI image fusion, 4D CT or Met-PET/CT, evolved in the last decade and yielded the most precise information for localizing parathyroid adenomas. Recently, 11C-methionine positron emission tomography has been reported to detect parathyroid adenomas with a sensitivity of 91 % even in the presence of multinodular goitre or after previous neck surgery [13]. However, its applicability is reduced due to relatively high costs and restricted availability (needing an on-site cyclotron to produce the short-lived tracer 11C-methionine). For all localization studies, efficiency is reduced in the presence of multiglandular disease [13, 14].
Four-dimensional CT associates both functional information—based on changes in perfusion—and anatomic detail in a single study [5]. The sensitivity of 4D CT has been shown to be superior (92 %) compared with sestamibi scintigraphy (70 %). In a sestamibi-negative subgroup, the BNE was avoided in 62 % due to localization in 4D CT. In the reoperative subgroup, there was no need for BNE at all [7]. In a different study of 45 patients who had undergone previous neck exploration, the 4D CT had 88 % sensitivity for abnormal parathyroid glands compared to sestamibi-SPECT (54 %) or neck ultrasound (21 %) [15]. Hunter et al. showed that 4D CT accurately lateralized the abnormal gland in 93.7 %. Due to the superior accuracy compared with ultrasound and sestamibi scanning, the authors proposed that 4D CT may be sufficient to be used as the sole presurgical localization method [6].
In the present study, we present our experience with preoperative CT in a negative selection of a patient collective with failed localization, including seven persistent and four recurrent pHPT as well as four re-explorations after thyroid surgery. The overall cure rate was 96 % (including three reoperations). As negative or discordant imaging selects a patient collective with an increased risk of multiglandular disease [14], we observed a rate of 24 % (six of 25 patients) in the present series. The overall sensitivity of CT scan was 54 %, with no significant difference between the thin-slice CT and the 4D CT. After previous neck surgery, 10/15 patients (67 %) compared to 3/10 patients (30 %) of surgically naive cases could be correctly localized using the preoperative CT scan. Our results support the findings of Mortenson et al. who reported a sensitivity of 88 % for 4D CT [15]. In their study, the 4D CT significantly more often correctly localized and lateralized hyperfunctional parathyroid tissue than sestamibi did. Four-dimensional CT successfully localized hyperfunctional parathyroid tissue in 18 (82 %) of 22 cases after previous neck surgery for non-HPT conditions, 10 (91 %) of 11 cases after previously unsuccessful neck exploration for HPT and 8 (67 %) of 12 cases who had a previous neck exploration with resection of at least one hypercellular parathyroid.
All in all, a bilateral exploration could be avoided in 10 out of 13 patients with positive CT. The advantage of a limited exploration is mainly represented by the lower incidence of postoperative hypoparathyroidism. In the present series, we observed one case of postoperative hypoparathyroidism after focused parathyroidectomy and previous thyroidectomy compared to two cases after bilateral exploration. The main limitation of the CT scan was the inability to detect multiglandular disease (three patients with resection of more than one gland in our series). Our results are therefore in contrast with the experience reported by Brown et al. from Sidney [7]. In fact, in their series of 99 patients, six of eight cases with multiple adenomas were identified preoperatively by 4D CT. All six cases with preoperatively localized multiple adenoma were cured, whereas one of the two without preoperative diagnosis had persistent hyperparathyroidism. Four-dimensional CT showed a sensitivity of 75 % and a positive predictive value (PPV) of 50 %, compared with sestamibi with a sensitivity of 7.7 % and a PPV of 100 %. The authors related the observed high false-positive rate to the exquisite detail in image acquisition, therefore over-diagnosing normal parathyroid glands as adenomas. Also, Rodgers and colleagues reported a correct prediction of multigland disease in five (45 %) out of 11 patients [5]. In three of these patients, the 4D CT correctly identified all of the diseased glands. In contrast, ultrasonography recognized no enlarged parathyroid gland in these patients (0 %), whereas sestamibi predicted the involvement of one gland in a single patient (9 %).
The second limitation of the CT scan was the inability to detect two cases of mediastinal parathyroid glands. In both cases, the preoperative thin-slice CT scan was not able to identify the enlarged gland located in the anterior mediastinum. Four-dimensional CT could have a higher detection rate due to the different dynamics of the iodinated contrast of parathyroid tissue compared to enlarged lymph nodes.
According to these limitations, 4D CT should be used judiciously in young pHPT patients as it imparts a significantly higher thyroid radiation dose than Sestamibi scintigraphy with a calculated risk of 4D CT-related thyroid cancer developing, calculated for a 20-year-old woman, of 1040/million (about 0.1 %) [16].
In conclusion, the CT scan identified more than half of abnormal parathyroid glands missed by conventional imaging. The sensitivity of thin-slice CT and 4D CT did not differ significantly. Both failed in detecting a multiglandular disease. BNE remains necessary if there are multiple candidate lesions or failed localization. We suggest a routine use of a preoperative CT scan in challenging cases with negative/unclear sestamibi and ultrasound prior to reoperation. The superiority of 4D CT should be demonstrated in larger comparative studies.
References
Kaplan EL, Yashiro T, Salti G (1992) Primary hyperparathyroidism in the 1990s. Choice of surgical procedures for this disease. Ann Surg 215(4):300–317
Mihai R, Simon D, Hellman P (2009) Imaging for primary hyperparathyroidism—an evidence-based analysis. Langenbeck's Arch Surg/Dtsch Ges Chir 394(5):765–784. doi:10.1007/s00423-009-0534-4
Alesina PF, Singaporewalla RM, Walz MK (2010) Video-assisted bilateral neck exploration in patients with primary hyperparathyroidism and failed localization studies. World J Surg 34(10):2344–2349. doi:10.1007/s00268-010-0700-4
Henry JF (2010) Reoperation for primary hyperparathyroidism: tips and tricks. Langenbeck's Arch Surg/Dtsch Ges Chir 395(2):103–109. doi:10.1007/s00423-009-0560-2
Rodgers SE, Hunter GJ, Hamberg LM, Schellingerhout D, Doherty DB, Ayers GD, Shapiro SE, Edeiken BS, Truong MT, Evans DB, Lee JE, Perrier ND (2006) Improved preoperative planning for directed parathyroidectomy with 4-dimensional computed tomography. Surgery 140(6):932–940. doi:10.1016/j.surg.2006.07.028, discussion 940-931
Hunter GJ, Schellingerhout D, Vu TH, Perrier ND, Hamberg LM (2012) Accuracy of four-dimensional CT for the localization of abnormal parathyroid glands in patients with primary hyperparathyroidism. Radiology 264(3):789–795. doi:10.1148/radiol.12110852
Brown SJ, Lee JC, Christie J, Maher R, Sidhu SB, Sywak MS, Delbridge LW (2014) Four-dimensional computed tomography for parathyroid localization: a new imaging modality. ANZ J Surg. doi:10.1111/ans.12571
Bergenfelz AO, Wallin G, Jansson S, Eriksson H, Martensson H, Christiansen P, Reihner E (2011) Results of surgery for sporadic primary hyperparathyroidism in patients with preoperatively negative sestamibi scintigraphy and ultrasound. Langenbecks Arch Chir Surg/Dtsch Ges Chir 396(1):83–90. doi:10.1007/s00423-010-0724-0
Dy BM, Richards ML, Vazquez BJ, Thompson GB, Farley DR, Grant CS (2012) Primary hyperparathyroidism and negative Tc99 sestamibi imaging: to operate or not? Ann Surg Oncol 19(7):2272–2278. doi:10.1245/s10434-012-2325-3
Thier M, Nordenstrom E, Bergenfelz A, Westerdahl J (2009) Surgery for patients with primary hyperparathyroidism and negative sestamibi scintigraphy—a feasibility study. Langenbeck’s Arch Surg/Dtsch Ges Chir 394(5):881–884. doi:10.1007/s00423-009-0524-6
Karakas E, Muller HH, Schlosshauer T, Rothmund M, Bartsch DK (2013) Reoperations for primary hyperparathyroidism—improvement of outcome over two decades. Langenbeck’s Arch Surg/Dtsch Ges Chir 398(1):99–106. doi:10.1007/s00423-012-1004-y
Schalin-Jantti C, Ryhanen E, Heiskanen I, Seppanen M, Arola J, Schildt J, Vaisanen M, Nelimarkka L, Lisinen I, Aalto V, Nuutila P, Valimaki MJ (2013) Planar scintigraphy with 123I/99mTc-sestamibi, 99mTc-sestamibi SPECT/CT, 11C-methionine PET/CT, or selective venous sampling before reoperation of primary hyperparathyroidism? J Nucl Med 54(5):739–747. doi:10.2967/jnumed.112.109561
Weber T, Maier-Funk C, Ohlhauser D, Hillenbrand A, Cammerer G, Barth TF, Henne-Bruns D, Boehm BO, Reske SN, Luster M (2013) Accurate preoperative localization of parathyroid adenomas with C-11 methionine PET/CT. Ann Surg 257(6):1124–1128. doi:10.1097/SLA.0b013e318289b345
Sebag F, Hubbard JG, Maweja S, Misso C, Tardivet L, Henry JF (2003) Negative preoperative localization studies are highly predictive of multiglandular disease in sporadic primary hyperparathyroidism. Surgery 134(6):1038–1041. doi:10.1016/j.surg.2003.07.021, discussion 1041-1032
Mortenson MM, Evans DB, Lee JE, Hunter GJ, Shellingerhout D, Vu T, Edeiken BS, Feng L, Perrier ND (2008) Parathyroid exploration in the reoperative neck: improved preoperative localization with 4D-computed tomography. J Am Coll Surg 206(5):888–895. doi:10.1016/j.jamcollsurg.2007.12.044, discussion 895-886
Mahajan A, Starker LF, Ghita M, Udelsman R, Brink JA, Carling T (2012) Parathyroid four-dimensional computed tomography: evaluation of radiation dose exposure during preoperative localization of parathyroid tumors in primary hyperparathyroidism. World J Surg 36(6):1335–1339. doi:10.1007/s00268-011-1365-3
Conflicts of interest
The manuscript has not been submitted to more than one journal for simultaneous consideration. The manuscript has not been published previously (partly or in full). The study is not split up into several parts and submitted to various journals. No data have been fabricated or manipulated (including images). Consent to submit has been received explicitly from all the co-authors before the work is submitted. The authors whose names appear on the submission have contributed sufficiently to the scientific work and therefore share collective responsibility and accountability for the results. The authors have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Seeliger, B., Alesina, P.F., Koch, JA. et al. Diagnostic value and clinical impact of complementary CT scan prior to surgery for non-localized primary hyperparathyroidism. Langenbecks Arch Surg 400, 307–312 (2015). https://doi.org/10.1007/s00423-015-1282-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-015-1282-2