Abstract
The aim of this study is to evaluate the effectiveness of preoperative imaging localization of hyper functioning parathyroid glands and comparing it with operative neck exploration in secondary hyperparathyroidism. This study was performed in Minia University Hospital between January 2017 and May 2018. Twenty patients with secondary hyperparathyroidism were included in this study. Ultrasonography was done for all patients, and then we classify our patients into two groups: in group 1 patients, Technetium-99 m sestamibi scan and computed tomography were done preoperatively while in group 2, patients underwent operation with neck exploration directly without other preoperative localization procedures. Mean age in our cases was 45.2 ± 9.46, while the most affected age group was (40–49) years by (35%), then (30–39) years by (30%), then (50–59) years by (25%), and then (≥ 60) years by (10%), while females were more affected than male by (75%) of cases. CT sensitivity in detection of parathyroid disease was 70%, and sestamibi detects 80% while neck exploration detection sensitivity was 100%. Neck exploration is the only reliable localization procedure in the cases of secondary hyperparathyroidism.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The majority of patients with secondary hyperparathyroidism can be managed by medical treatment. Some patients require surgical treatment; successful parathyroidectomy often results in a dramatic drop in the parathyroid hormone levels, relieves the patients from clinical symptoms, and reduces mortality [1].
In the era of minimally invasive parathyroid surgery, preoperative imaging is routinely performed to aid both surgical planning and intra-operative dissection [2].
However, even when multiglandular disease is suspected or imaging fails to localize abnormal parathyroid glands, ultrasonography has an important role to play in the management of concurrent thyroid disease. The reported incidence of nodular thyroid disease detected at ultrasonography in patients with concurrent hyperparathyroidism ranges from 29 to 51% [3].
Contrast-enhanced computed tomography can be used to detect abnormal parathyroid glands. Lesion conspicuity is increased by the intense enhancement of the lesions [4]. Technetium-99 m sestamibi is the most commonly used radiotracer for parathyroid scintigraphy [5].
Abnormal parathyroid tissue commonly retains Technetium-99 m sestamibi longer than thyroid tissue, leading to the widespread use of delayed imaging to improve upon the conspicuity of hyperfunctioning parathyroid tissue [6]. Negative or discordant imaging studies should not inhibit referral to an experienced parathyroid surgeon [7].
Patients and Methods
This study was performed in the El-Minia University Hospital between January 2017 and May 2018. Twenty patients with secondary hyperparathyroidism were included in this study. Patients included in the study had serum parathormone (PTH) level more than 500 pg/mL on two or more occasions with hypercalcemia (serum calcium level more than 1 mg/dl of upper limit of normal calcium range) and hypercalciuria (24 h urinary Ca more than 400 mg) or had diffuse hyperplasia identified by ultrasound imaging. We excluded patients with serum PTH level less than 500 pg/mL on two or more occasions, patients with primary hyperparathyroidism, and patients unfit for anesthesia and operation.
All Patients underwent complete history taking and clinical examination with assessment of the patient’s general medical fitness, laboratory investigation as complete blood picture, measurement of blood calcium (total and ionized) and phosphorus, serum albumin, PTH assay and interpretation, vitamin D and calcitonin, serum alkaline phosphatase, serum urea and creatinine, serum TSH, free T3, free T4, 24-h urinary calcium, creatinine and calcium/creatinine ratio (UCCR), coagulation profile as prothrombin time (PT), concentration (PC), and INR.
Ultrasonography was done for all patients by single sonography consultant (professor). Then, we classify our patients into two groups: in group 1 patients, Technetium-99 m sestamibi scan and 4-D computed tomography (4-D CT) were done preoperatively while in group 2, patients underwent operation with neck exploration directly without other preoperative localization procedures. The exact protocol was operating for diagnosed cases of hyperparathyroidism and did not treat medically as it is expensive and patients are non-compliant.
Vocal cords were assessed by preoperative indirect laryngoscopy. In patients with high calcium levels preoperatively, we treat them with hydration, diuresis, and steroids (prednisolone 20 mg TID for 5 days before surgery).
Neck exploration was done for all patients whatever the imaging results were.
Patients were kept in postoperative room with the head end tilted 30° upwards. Once patient was fully awake with normal breathing which was 4–6 h, patient is shifted to the ward.
Patients were observed for bleeding, formation of hematoma, stridor, drop in O2 saturation, tachycardia, and tachypnea. Patients receive analgesic (paracetamol) given once daily.
Circumoral paresthesia/numbness, change in mental status, carpopedal spasm, and tetany were observed. Hungry bone syndrome can cause severe hypocalcemia in immediate postoperative period which is initially corrected by IV calcium gluconate—10 ml of 10% which was given in some cases.
In some cases, wound infection occurred which needed antibiotic for 5 to 7 days and repeated wound dressing with topical antibiotic.
Drain was removed after 24 h, and patients were discharged except three cases stayed at the hospital until correction of postoperative hypocalcemia, but they were discharged after 3 days.
Oral calcium (calcium carbonate) and vitamin D supplementation were given for 2–6 months.
We followed the patients in outpatient clinic after 2 weeks, 3 months, and 12 months by neck U/S, PTH, and serum calcium.
Statistical Analysis
Statistical analysis was performed with SPSS version 23.0. Data were expressed as range (minimum and maximum), mean, and standard deviation (SD) for numerical data or number and percent (%) categorical data. Student’s t test, chi-square, and Fisher’s exact test were used for comparison as most appropriate. A P value of less than 0.05 was considered statistically significant.
Result
Table 1 shows that mean age in our cases was 45.2 ± 9.46, while the most affected age group was (40–49) years by (35%), then (30–39) years by (30%), then (50–59) years by (25%), and then (≥ 60) years by (10%), while females were more affected than male by (75%) of cases. The most common clinical picture was musculoskeletal pain which occurred in 14 cases, then nephrolithiasis which occurred in three cases only, and then neck and mandibular swelling.
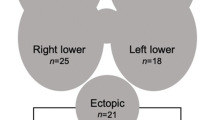
Table 2 shows that two glands were affected in 20% of cases, the right side more affected than the left side by (15%) to (10%), the inferior glands more affected than the superior glands by (25%) to (0%), while both the superior and inferior gland were affected in 20% of cases. CT neck showed one gland affected in 50% of cases while two glands were affected in 20% of cases. Tech-99 was done in ten cases; eight of them showed overactive lesion (four in all glands and four in 2 glands) while in two cases showed equivocal study. Mean PTH is 1583.7 ± 517.8, mean Ca is 10.85 ± 0.82, mean ALP is 629.5 ± 525.1, mean phosphorus is 4.8 ± 2.3, and mean 24-h urinary Ca is 332.7 ± 59.8.
Table 3 shows minimally invasive procedure done in 0 while bilateral neck exploration done in all cases (100%); in seven cases, 1 gland was excised and in two cases, 2 glands were excised, while total parathyroidectomy was done in 11 cases (nine cases with sternomastoid autotransplantation and two cases with forearm autotransplantation).
Table 4 shows sensitivity, specificity, positive, and negative predictive values of ultrasound, CT, and sestamibi separately, and it was found that sonar detects four out of ten cases (40%), CT detects seven out of ten cases (70%) of parathyroid enlargement while sestamibi detects 80% neck exploration, and 100% of cases were found to have parathyroid disease. Also, sensitivity was determined for combined results considering sonar, CT, and sestamibi as a single test, and it was found that sensitivity increased and reached 96%.
The most common postoperative complication was carpopedal spasm (15%) while wound infection was (10%). Eighty-five percent of cases were discharged after 1 day while (10%) of cases were discharged after 2 days and (5%) after 3 days due to carpopedal spasm.
Table 5 shows that mean PTH after 2 weeks was 10.4 ± 1.4, mean Ca after 2 weeks was 7.76 ± 0.32, mean PTH after 3 months was 27.3 ± 6.7, mean Ca after 3 months was 8.3 ± 0.60, mean PTH after 12 months was 47.1 ± 6.67, and mean Ca after 12 months was 8.8 ± 0.51.
Discussion
In this study, mean age was 45.2 ± 9.46 years; while in [8], mean age was 50.8 years; in [9], mean age was 43 years; and in [10], mean age was 38.8 ± 9.8 years.
In this study, 75% of cases were female; while in [8], 57% of cases were female; in [10], 76% of cases were female; in [9], 68% of cases were female; and in [11], 74% of cases were female.
In this study, the most common presentation was musculoskeletal pain which occurred in 70% of cases, then nephrolithiasis by 15% of cases; while in [8], the most common presentation was nephrolithiasis which occurred in (56.7%) of cases, then osteopenia or osteoporosis by (43.3%) of cases; and while in [12], the most common presentation was musculoskeletal pain by 52.8%, then nephrolithiasis by 30%.
In this study, neck ultrasound (US) was done in all cases, while in [13], neck US was done 81.4%.
In this study, neck US shows that all glands were affected in 0% of cases, two glands affected in 20% of cases, one gland affected in 25% of cases, while in [8], neck US shows that one gland was affected in 60% of cases, two glands were affected in 30% of cases, and all glands were affected in 3.3% of cases.
In this study, right glands were affected in 15%, while left glands were affected in 10%, both right and left glands affected in 20%, while in [8], right glands were affected in 30%, left glands were affected in 25%, and intrathymic glands occurred in 30% of cases.
In this study, inferior glands were affected alone in 25% of cases, superior glands were affected alone in 0% of cases, while both superior and inferior glands were affected in 20% of cases, while in [8], inferior glands alone were affected in 20% of cases, while superior glands were affected alone in 35% of cases.
In this study, CT neck was done in 50% of cases; 50% of cases in CT show one gland was affected and 20% of cases, two glands were affected, while in [13], CT neck was done in 9% of cases while in [8], CT neck was done in 33% of cases.
In this study, Tech-99 was done in 50% of cases; 80% of cases showed overactive lesion and 20% of cases showed equivocal study, while in [13], Tech-99 was done in 32.5% of cases, and 97% of this cases showed overactive lesion, while in [8], Tech-99 was done in 83% of cases, and 60% of this cases showed overactive lesion.
In this study, the mean PTH was 1583.7 ± 517.8; while in [14], mean PTH in secondary cases was 261 ± 280; in [8], mean PTH was 118.6 ± 25.7; in [15], mean PTH was 219.75 ± 238.01 in secondary cases; and in [12], mean PTH was 114 in secondary cases.
The difference in values between our results and the others is due to the inability of our patients to take medical treatment for their disease as it is costly.
In this study, mean calcium was 10.85 ± 0.82; while in [12], mean calcium in secondary cases was 11.2 ± 0.7; in [14], mean calcium in secondary cases was 11.0; and in [8], mean calcium in secondary cases was 10.9 ± 0.2.
In this study, mean phosphorus was 4.8 ± 2.3; while in [8], mean phosphorus was 2.8 ± 0.1; and in [15], mean phosphorus was 0.82 ± 0.2 (mmol/l).
In this study, bilateral neck exploration was done in all cases, excision of one gland was done in 35% of the cases, excision of two glands was done in 10% of the cases, and total parathyroidectomy with autotransplantation was done in 55% of cases; while in [16], bilateral neck exploration was done in all cases, 52% of cases in total parathyroidectomy was done, with 50% of total cases were excision of four glands and 48% of cases were total parathyroidectomy with autotransplantation; and in [17], total parathyroidectomy with autotransplantation was done in 67% of cases and subtotal parathyroidectomy was done in 33% of cases.
In this study, the most common complication was carpopedal spasm which was done in 15% of cases, then wound infection in 10% of the cases; while in [17], the most common complication was recurrence in 1.9% of cases then hypocalcemia in 0.73%, then hematoma in 0.15% of cases; while in [16], the most common complication was recurrent laryngeal nerve palsy in 10.5% of cases then postoperative bleeding in 4%, then persistence in 3% of cases; while in [12], the most common complication was recurrent nerve injury in 0.99% of cases then hypocalcemia in 0.49%.
In this study, postoperative hospital stay was 1 day in 85%, 2 days in 10%, and 3 days in 5% of cases, while in [16] was 7–10 days in 90% of cases.
In this study, mean PTH after 2 weeks postoperative was 10.4 ± 1.4; while in [17], mean PTH postoperative in secondary cases was 61.4 ± 12.6; in [16], mean PTH was 98.2 ± 156.8 in secondary cases; in [15], mean PTH was 49.5 ± 47.4; and in [8], mean PTH was 17.7 ± 3.8.
In this study, mean postoperative calcium was 7.76 ± 0.32; while in [14], mean calcium in secondary cases was 8.75; in [8], mean calcium was 9.3 ± 0.2; in [15], mean calcium was 2.27 ± 0.17 (mmol/l); and in [16], mean calcium was 2.2 (mmol/l).
No level I or II evidence reliably identifies preoperative clinical risk factors for determining which patients should have routine bilateral neck exploration for multi-gland disease or for intraoperative decision making to convert to bilateral neck exploration [18].
In our study, bilateral neck exploration was the only localizing procedure that detects all diseased glands with a large percent difference than CT and sestamibi scan. So, we cannot rely on these localizing investigations in parathyroid surgery especially in secondary hyperparathyroidism in which parathyroid hyperplasia is common.
References
Tominaga Y, Matsuoka S, Uno N (2009) Surgical and medical treatment of secondary hyperparathyroidism in patients on continuous dialysis. World J Surg 33(11):2335–2342
Tublin ME, Pryma DA, Yim JH, Ogilvie JB, Mountz JM, Bencherif B, Carty SE (2009) Localization of parathyroid adenomas by sonography and technetium Tc 99m sestamibi single-photon emission computed tomography before minimally invasive parathyroidectomy. J Ultrasound Med 28(2):183–190
Adler JT, Chen H, Schaefer S, Sippel RS (2010) Does routine use of ultrasound result in additional thyroid procedures in patients with primary hyperparathyroidism? J Am Coll Surg 211(4):536–539
Gotway M, Higgins CB (2000) MR imaging of the thyroid and parathyroid glands. Magn Reson Imaging Clin N Am 8(1):163–182 ix
Bergenfelz A, Tennvall J, Valdermarsson S, Lindblom P, Tibblin S (1997) Sestamibi versus thallium subtraction scintigraphy in parathyroid localization: a prospective comparative study in patients with predominantly mild primary hyperparathyroidism. Surgery 121(6):601–605
Taillefer R, Boucher Y, Potvin C, Lambert R (1992) Detection and localization of parathyroid adenomas in patients with hyperparathyroidism using a single radionuclide imaging procedure with technetium-99m-sestamibi (double-phase study). J Nucl Med 33(10):1801–1807
Kunstman JW, Kirsch JD, Mahajan A, Udelsman R (2013) Parathyroid localization and implications for clinical management. J Clin Endocrinol Metabol 98(3):902–912
Sun PY, Thompson SM, Andrews JC, Wermers RA, McKenzie TJ, Richards ML, Farley DR, Thompson GB (2016) Selective parathyroid hormone venous sampling in patients with persistent or recurrent primary hyperparathyroidism and negative, equivocal or discordant noninvasive imaging. World J Surg 40(12):2956–2963
Lai H-W, Lee C-H, Chen J-Y, Tseng L-M, Yang A-H (2006) Insular thyroid carcinoma: collective analysis of clinicohistologic prognostic factors and treatment effect with radioiodine or radiation therapy. J Am Coll Surg 203(5):715–722
Huang DK-R, Chou F-F, Chi S-Y, Chan Y-C, Huang S-C (2017) Surgical management of primary hyperparathyroidism: a single-center experience. Asian Journal of Surgery 41(4):377–383
Gasser RW (2013) Clinical aspects of primary hyperparathyroidism: clinical manifestations, diagnosis, and therapy. Wien Med Wochenschr 163(17–18):397–402
Udelsman R, Lin Z, Donovan P (2011) The superiority of minimally invasive parathyroidectomy based on 1650 consecutive patients with primary hyperparathyroidism. Ann Surg 253(3):585–591
Cheung K, Wang TS, Farrokhyar F, Roman SA, Sosa JA (2012) A meta-analysis of preoperative localization techniques for patients with primary hyperparathyroidism. Ann Surg Oncol 19(2):577–583
Eigelberger MS, Cheah WK, Ituarte PH, Streja L, Duh Q-Y, Clark OH (2004) The NIH criteria for parathyroidectomy in asymptomatic primary hyperparathyroidism: are they too limited? Ann Surg 239(4):528–535
Philippon M, Guerin C, Taieb D, Vaillant J, Morange I, Brue T, … Sebag F (2014) Bilateral neck exploration in patients with primary hyperparathyroidism and discordant imaging results: a single-centre study. Eur J Endocrinol 170(5):719–725
Schlosser K, Bartsch DK, Diener MK, Seiler CM, Bruckner T, Nies C, … Glockzin G (2016) Total parathyroidectomy with routine thymectomy and autotransplantation versus total parathyroidectomy alone for secondary hyperparathyroidism: results of a nonconfirmatory multicenter prospective randomized controlled pilot trial. Ann Surg 264(5):745–753
Chen J, Jia X, Kong X, Wang Z, Cui M, Xu D (2017) Total parathyroidectomy with autotransplantation versus subtotal parathyroidectomy for renal hyperparathyroidism: a systematic review and meta-analysis. Nephrology 22(5):388–396
Moalem J, Guerrero M, Kebebew E (2009) Bilateral neck exploration in primary hyperparathyroidism--when is it selected and how is it performed? World J Surg 33(11):2282–2291
Acknowledgements
The authors would like to offer their sincere thanks to all the people who participated in the study.
Author information
Authors and Affiliations
Contributions
Dr. Emad and Dr. Adel had made substantial contributions to conception and design and perform analysis and interpretation of data. Dr. Mohammed and Dr. Amr participate in the result section of the paper and they had been involved in drafting the manuscript or revising it critically for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
The title, aim, and plan of the study were discussed and approved regarding the ethics of research in the General Surgical Department and we took the agreement from the ethical committee of the Minia Faculty of Medicine. All patients signed a written consent, accepted, and were aware of the procedure in the treatment they will receive.
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
El-Sageer, E.M., Shehata, A.M., Khalaf, M. et al. Neck Exploration Versus Imaging Localization of Parathyroid in Secondary Hyperparathyroidism. Indian J Surg 81, 457–461 (2019). https://doi.org/10.1007/s12262-018-1842-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-018-1842-0