Abstract
Background and aims
The physiology of the patient during laparoscopy differs from that of open surgery. Both pneumoperitoneum and obstructive jaundice impair the hepatic function, but the combined insult has not been previously examined. In this study, we aimed to investigate the effects of carbon dioxide (CO2) pneumoperitoneum on hepatic function in a rat model of obstructive jaundice.
Methods
Forty-four male Sprague–Dawley rats were divided into four groups: group 1 (n = 10), sham-operated group; group 2 (n = 12), obstructive jaundice group; group 3 (n = 10), CO2 pneumoperitoneum group; and group 4 (n = 12), obstructive jaundice and CO2 pneumoperitoneum group. Common bile duct was ligated and divided in the obstructive jaundice groups. After 6 days, a 12-mmHg pneumoperitoneum was induced, maintained for 60 min, and released for 120 min. Blood samples were drawn for the measurement of white blood cell and platelet counts, serum liver enzymes (aspartate aminotransferase [AST], alanine aminotransferase [ALT], total bilirubin). Tissue samples were obtained for analyses of malondialdehyde (MDA), glutathione (GSH), and superoxide dismutase (SOD) levels. We evaluated the degree of liver injury on a grading scale from 0 to 4, histopathologically.
Results
Pneumoperitoneum after biliary obstruction resulted in an increase in AST and ALT levels and a decrease in white blood cell and platelet counts. However, changes in liver tissue MDA, GSH, and SOD levels did not correlate with the changes in AST and ALT levels and white blood cell and platelet counts. After sham operation with pneumoperitoneum, the GSH levels in liver homogenate were significantly decreased in the group 3 when compared to the group 2. On the other hand, obstructive jaundice itself caused significant reduction in the SOD activity of liver homogenate in comparison to the group 3. Histopathologically, sinusoidal congestion and vacuolization were more severe in the group 3.
Conclusions
Alterations in hepatic function occur in pneumoperitoneum applied jaundiced subjects. However, there were no statistically significant differences between the groups 2 and 4 with regard to white blood cell and platelet counts, serum liver enzymes including AST, ALT, and total bilirubin values, MDA and GSH levels and SOD activity of liver homogenate, and histologic damage. These results indicate that there is no additional risk on liver function associated with pneumoperitoneum performed in obstructive jaundice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic surgery is now being used in the vast majority of more extensive and time-consuming abdominal surgical operations including antireflux fundoplication, splenectomy, gastric or colorectal resection with its numerous advantages such as decreased postoperative pain, shorter hospital stay, reduction in complications, and lost working days [1]. However, several studies have shown that carbon dioxide (CO2) pneumoperitoneum (PP) alters adversely systemic and pulmonary hemodynamic parameters, including reduced cardiac output and increased mean arterial pressure, vena caval pressure, and pulmonary arterial wedge pressure [2]. In addition, acid-base changes, bacterial translocation, and splanchnic ischemia have been demonstrated during CO2 PP [3–5]. On the other hand, the intra-abdominal pressure of 12–14 mmHg of CO2 traditionally used in laparoscopic surgery is higher than normal pressure values of the portal system (7–10 mmHg). This PP value, therefore, reduces portal flow and causes physiological alterations in liver function.
Biliary obstruction results in development of oxidant injury, hepatic fibrosis, biliary cirrhosis, and portal hypertension [6]. Although the mechanism of acute hepatocellular injury and resultant progressive fibrogenesis in bile flow obstruction is not well elucidated, oxidant stress has been proposed as one process which might be involved in both problems. Cholestasis per se reduces antioxidative capacities in liver mitochondria [7]. Accumulation of hydrophobic bile acids and inflammatory cells in the liver tissue may cause increased production of free radicals in biliary obstruction [8]. Bile acids, especially, enhance reactive oxygen species (ROS) released by polymorphonuclear leukocytes [9]. Moreover, in obstructive jaundice (OJ), the absence of intestinal bile flow, impaired reticuloendothelial system function and immunity, intestinal bacterial overgrowth, and physical disruption of the gut mucosal barrier explain the high incidence of infectious complications [10, 11].
Surgery in patients with OJ is associated with increased morbidity and mortality. Laparoscopy can be used in jaundiced patients with biliary tract or pancreatic head carcinoma both for staging and palliative treatment and in patients with common bile duct (CBD) stones for biliary exploration and clearance of their stones. On the other hand, cholestasis can be reproduced in rodents by surgical ligation of the CBD. The model of CBD ligation has been well evaluated and described in rats [12]. Although a detailed description of the morphological and molecular changes following bile duct ligation (BDL) in rats is lacking, this model has been used widely to study cholestatic liver injury [13], fibrogenesis [14], and the impact of OJ on a second hit such as infection or hepatic ischemia [15, 16]. Importantly, the effect of CO2 PP on injury and repair in the different cellular compartments of the liver in the setting of biliary obstruction has not been characterized. Therefore, in this study, we investigated the impact of CO2 PP on hepatocellular injury and proliferation, serum markers of cholestasis, and tissue indicators of oxidative stress in CBD-ligated rats
Materials and methods
Animal care and use
Male Sprague–Dawley rats weighing between 250 and 280 g were used in this study. Animals were housed in a light-controlled room with a 12-h light/dark cycle and were allowed free access to food and water. The operative procedure, use of anesthesia, and animal care methods in the experiments were consistent with the guidelines in the National Institute of Health’s Guide for the Care and Use of Laboratory Animals (NIH publication number 86-23, revised 1985, Bethesda, Maryland). After obtaining the approval of Institutional Animal Use and Care Committee of Ankara University, Faculty of Veterinary Medicine, the experiment was performed at Experimental Research Center of Selcuk University, School of Medicine.
Operative details and study groups
After an overnight fast, the rats were anesthetized by an intramuscular injection of ketamine 50 mg/kg (Ketalar; Parke Davis, Eczacibasi, Istanbul, Turkey) and xylazine 10 mg/kg (Rompun; Bayer AG, Leverkusen, Germany). Animals were allowed to breathe spontaneously during the surgery. A heating lamp was used to preserve the body temperature at approximately 37°C. A total of 10 mL lactated Ringer’s solution was given subcutaneously to prevent dehydration of the rats. After skin shaving and preparation of the abdominal wall with 10% povidone–iodine solution, a midline laparotomy was performed. The animals were allocated into four groups: in group 1 (sham-operated control group, n = 10), these animals were anesthetized and underwent laparotomy, identical to other groups. The CBD was isolated, and a ligature was passed around the bile duct without ligation, then the abdominal incision was closed. The animals received food and water ad libitum. The animals were followed-up for 6 days to simulate the OJ in other groups. In group 2 (OJ group, n = 12), the CBD was exposed carefully and doubly ligated with 4-O monofilament glycomer (Biosyn, USSC, USA), then divided to prevent recanalization of the bile duct. In group 3 (CO2 PP group, n = 10), identical to sham-operated rats except for the induction of CO2 PP. After 6 days, these animals were reanesthetized. The abdomen was punctured with a 20-gauge intravenous cannula, and the cannula was connected to an electronic insufflator (Storz & Co., Tutthufen, Germany). A 12 mmHg PP was induced at a flow rate of 0.2 L/min, maintained for 60 min, and released completely for 120 min. In group 4 (OJ and CO2 PP group, n = 12), the same procedures as described for groups 2 and 3 were performed.
On postoperative day 6, all animals were anesthetized again, and at the end of 2 h of desufflation period in the CO2 PP groups 3 and 4, all animals in four groups were sacrificed. Blood samples were drawn by cardiac puncture into two sets of tubes, with and without ethylenediaminetetraacetic acid (EDTA). Then, the abdomen was opened and a small portion of the left lobe (for analysis of tissue malondialdehyde [MDA] level), median lobe (for analysis of tissue glutathione [GSH] level), and right lobe (for analysis of tissue superoxide dismutase [SOD] activity and histologic examination) of the liver were excised and immediately frozen in liquid nitrogen and stored at −80°C until assay.
Laboratory tests
These included white blood cell and platelet counts, serum liver enzymes, liver tissue MDA and GSH levels, and liver tissue SOD activities. All samples were blindly analyzed.
Blood tests
The tubes were centrifuged at 3,000 rpm for 30 min immediately after drawn, and plasma was separated. White blood cell and platelet counts and levels of serum aspartate aminotransferase (AST), alanine aminotransferase (ALT), and total bilirubin were measured by automated analyzers using appropriate kits (Coulter AU 400, USA, and Olympus AU 400, Japan).
Analysis of MDA levels
The tissue level of MDA was determined in the liver specimen homogenized in a ratio of 1:10 (w:v) in 1.15% cold KCl solution. Zero point five milliliter homogenate was mixed with 3 mL of 1% phosphoric acid and 1 mL of 0.6% thiobarbituric acid solution. The mixture was heated in a water bath for 45 min. After cooling to room temperature, 4 mL of n-butanol was added, and the mixture was shaken vigorously. After centrifugation at 3,000 rpm for 5 min, the n-butanol layer’s absorption was measured at 535 and 520 nm. The difference between the two absorptions was expressed as the MDA level in nanomoles per milligram of liver tissue [17].
Quantification of reduced GSH levels
The reduced-form GSH contents of liver tissue samples were measured by the method of Ellman [18]. Tissue samples were homogenized in 1 mL of 0.5 M metaphosphoric acid. This homogenate was centrifuged at 3,500 rpm for 10 min, and the supernatant was assayed. A standard solution was prepared in 3 mL amounts by mixing 0.3 mL of water, 0.3 mL of tamponate, and 2.4 mL of dithionitrobenzoic acid. The sample mixtures were each prepared by mixing 0.1 mL of water, 0.3 mL of tamponate, 2.4 mL of dithionitrobenzoic acid, and 0.2 mL of supernatant. The absorption of the two mixtures was measured at 410 nm, and the change in absorption was read as optical density. The protein concentration of the same samples was measured by the method of Lowry [19]. The amount of GSH in the tissues was then expressed as micromoles per milligram of protein.
Determination of SOD activity
Liver samples were homogenized in 0.1 M Tris/HCl buffer, pH 7.2, containing 154 mM NaCl. The homogenate was centrifuged at 13,000 rpm for 15 min. The protein concentration of the supernatant was measured by the method of Lowry [19]. SOD activities of the samples were determined by inhibition of nitroblue tetrazolium reduction, and xanthine–xanthine oxidase was used as a superoxide generator in the same supernatants [20]. The results were expressed as unit per milligram of protein. One unit of SOD is defined as the amount that inhibits the rate of nitroblue tetrazolium reduction by 50%.
Histopathologic evaluation
A part of each liver was fixed in 10% buffered formalin, embedded in paraffin, and stained with hematoxylin and eosin (HE). Blind analysis was performed on all samples by a pathologist based on the criteria used by Suzuki et al. [21]. Histologic changes were scored from 0 to 4 based on sinusoidal congestion and vacuolization, necrosis of parenchymal cells, and proliferation of bile ducts as shown in Table 1.
Statistical analysis
The results of liver injury scoring were expressed as median (range), whereas, other results were expressed as mean ± SEM (the standard error of the mean). The differences among the groups were evaluated by using one-way analysis of variance followed by post-hoc test (Tukey’s HSD test). The differences among the groups in terms of liver injury scores were evaluated using Kruskal–Wallis rank test, and multiple comparisons between the groups were performed with Mann–Whitney U test. The results were considered to be of statistical significance when p < 0.05. The data were analyzed by statistical software (SPSS for Windows 18.0; SPSS, Chicago, Illinois, USA).
Results
All animals, but four, tolerated the surgical procedures. Four rats in the OJ groups died during the experiment; one at postoperative day 2 and one at postoperative day 5 (group 2) and two during PP (group 4).
Blood test results
White blood cell and platelet counts and serum liver enzymes including AST, ALT, and total bilirubin values are shown in Table 2.
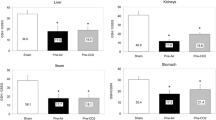
The levels of AST, ALT, and total bilirubin in the OJ groups (groups 2 and 4) were significantly higher than the values of the sham-operated group 1 and the PP-only group 3 (p = 0.001 and p = 0.01, respectively; Fig. 1). However, there were no significant differences between the groups 2 (OJ+/PP-) and 4 (OJ+/PP+) in terms of the levels of AST, ALT, and total bilirubin (p > 0.05). PP itself (group 3) elevated the levels of AST and ALT significantly compared to the sham-operated group 1 (p = 0.001 for AST level and p = 0.01 for ALT level) but statistically lower than the groups 2 (OJ+/PP-) and 4 (OJ+/PP+; p = 0.01). On the other hand, group 4 (OJ+/PP+) had higher AST and ALT levels than the groups 2 (OJ+/PP-) and 3 (OJ-/PP+).
The levels of AST and ALT in the groups (mean ± SEM). OJ obstructive jaundice, PP pneumoperitoneum. There were no significant differences between the groups 2 and 4 (p > 0.05). PP itself (group 3) elevated the levels of AST and ALT significantly compared to the group 1 (p = 0.001 for AST level and p = 0.01 for ALT level) but statistically lower than the groups 2 and 4 (p = 0.01; one-way analysis of variance (ANOVA) and Tukey’s HSD test)
The white blood cell counts in the groups 2 (OJ+/PP-), 3(OJ-/PP+), and 4 (OJ+/PP+) were significantly lower than the values of the sham-operated group 1 (p = 0.007, p = 0.003, and p = 0.004, respectively; Fig. 2). However, there were no significant differences between the groups 2 (OJ+/PP-) and 4 (OJ+/PP+) in terms of the white blood cell counts (p > 0.05). PP itself (group 3) decreased the white blood cell counts compared to the sham-operated group 1 (p = 0.003), but this reduction was not statistically significant in comparison to the OJ groups (groups 2 and 4; p > 0.05). On the other hand, group 4 (OJ+/PP+) had lower white blood cell counts than the groups 2 (OJ+/PP-) and 3 (OJ-/PP+).
White blood cell counts of the groups (mean ± SEM). OJ obstructive jaundice, PP pneumoperitoneum. The white blood cell counts in the groups 2, 3, and 4 were significantly lower than the values of the group 1 (p = 0.007, p = 0.003, and p = 0.004, respectively). However, there were no significant differences between the groups 2 and 4 (p > 0.05; one-way analysis of variance (ANOVA) and Tukey’s HSD test)
Although the platelet counts in the groups 2 (OJ+/PP-), 3 (OJ-/PP+), and 4 (OJ+/PP+) were lower than the values of the sham-operated group 1, only the difference between the sham-operated group 1 and the group 4 (OJ+/PP+) was statistically significant (p = 0.008; Fig. 3). In addition, there were no significant differences between the groups 2 (OJ+/PP-) and 4 (OJ+/PP+) in terms of the platelet counts (p > 0.05). PP itself (group 3) reduced the platelet counts, but this decrease was not statistically significant when compared to the OJ groups (groups 2 and 4; p > 0.05). On the other hand, group 4 (OJ+/PP+) had lower platelet counts than the groups 2 (OJ+/PP-) and 3 (OJ-/PP+).
Platelet counts of the groups (mean ± SEM). OJ obstructive jaundice, PP pneumoperitoneum. Although the platelet counts in the groups 2, 3, and 4 were lower than the values of the group 1, only the difference between the groups 1 and 4 was statistically significant (p = 0.008). However, there were no significant differences between the groups 2 and 4 (p > 0.05; one-way analysis of variance (ANOVA) and Tukey’s HSD test)
Briefly, group 4 (OJ+/PP+) had lower white blood cell and platelet counts and higher levels of AST, ALT, and total bilirubin in comparison to the group 2 (OJ+/PP-), although these were not statistically significant (p > 0.05).
MDA and GSH levels and SOD activity of liver homogenate
The levels of MDA and GSH and SOD activity are shown in Table 3. The MDA and GSH levels and the SOD activities were not significantly different between the groups 2 (OJ+/PP-) and 4 (OJ+/PP+; p > 0.05). However, there were significant differences between the groups 2 (OJ+/PP-) and 3 (OJ-/PP+) in terms of the GSH levels (p = 0.02) and SOD activities (p = 0.04). After sham operation with CO2 PP, the GSH levels in liver homogenate were significantly decreased in the group 3 when compared to the sham-operated group 1 and the group 2 (OJ+/PP-; p = 0.001 and p = 0.02, respectively; Fig. 4). On the other hand, OJ itself (group 2) caused significant reduction in the SOD activity of liver homogenate in comparison to the PP-only group 3 (p = 0.04). CO2 PP-induced liver tissue injury might lead to a perturbation in antioxidant defense mechanism of liver, suggesting that more oxygen free radicals were produced in the CO2 PP-only group 3, and GSH was rapidly consumed after elimination of free oxygen radicals. Similarly, OJ-induced liver tissue insult might cause an impairment in antioxidant capacity of liver, meaning that more ROS was generated in the OJ-only group 2, and SOD was quickly consumed before GSH after removal of free oxygen radicals.
GSH levels of the groups (mean ± SEM). OJ obstructive jaundice, PP pneumoperitoneum. There were no significant differences between the groups 2 and 4 (p > 0.05). Only the differences between the groups 1 and 3 and between the groups 2 and 3 were statistically significant (p = 0.001 and p = 0.02, respectively; one-way analysis of variance (ANOVA) and Tukey’s HSD test)
Histopathological values
The degree of histologic damage seen in liver tissue is shown in Fig. 5. No morphological damage was observed in any of the rats in the sham-operated group 1. OJ and PP each caused sinusoidal congestion and vacuolization, but these were more severe in the PP-only group 3 than in the OJ-only group 2 and the group 4 (OJ+/PP+; p = 0.001 and p = 0.04, respectively). However, there were no significant differences between the groups 2 (OJ+/PP-) and 4 (OJ+/PP+) in terms of sinusoidal congestion and vacuolization (p > 0.05). Up to 30% necrosis was seen in three rats in group 2 (OJ+/PP-), in two rats in group 3 (OJ-/PP+), and in two rats in group 4 (OJ+/PP+). In addition, apoptosis was seen in two rats in group 4 (OJ+/PP+). In terms of necrosis, however, there were no significant differences between any of the groups. Bile duct proliferation was observed only in the OJ groups (groups 2 and 4). Addition of the PP to the OJ did not affect the mean bile duct proliferation value (p > 0.05), but severe ductal proliferation was seen only in the group 4 (OJ+/PP+).
The degree of histologic damage seen in liver tissue (median [range]). OJ obstructive jaundice, PP pneumoperitoneum. There were no significant differences between the groups 2 and 4 (p > 0.05). Although sinusoidal congestion and vacuolization were developed in the groups 2, 3, and 4, these were more severe in the group 3 than in the groups 2 and 4 (p = 0.001 and p = 0.04, respectively; Kruskal–Wallis test and Mann–Whitney U test)
Discussion
Laparoscopic surgery has become the standard procedure of cholecystectomy and is being increasingly used for more complex procedures. However, the use of laparoscopic surgery for jaundiced patients has not yet been established. The adverse effects of CO2 PP on cardiac, pulmonary and renal function have been described in both experimental and clinical studies [22, 23]. Nevertheless, the effects of CO2 PP on hepatic function have not been studied in jaundiced patients. In the current study, a standardized rat model of BDL has been used to investigate the effects of CO2 PP on hepatic function in OJ. No statistically significant differences were found between the groups 2 (OJ+/PP-) and 4 (OJ+/PP+) with regard to white blood cell and platelet counts, serum liver enzymes including AST, ALT, and total bilirubin values, MDA and GSH levels and SOD activity of liver homogenate, and histologic damage.
The insufflation of CO2 into the peritoneal cavity to create the PP deteriorates hepatic cellular integrity with a subsequent increase in liver enzymes and alteration of the hepatic microcirculation [24–26]. Hepatic function during and after laparoscopic surgery has been examined in a number of clinical studies, and AST and ALT serum activities were found to be increased as a result of intra-abdominal pressure increase [24, 25, 27, 28]. Nickkholgh et al. clearly demonstrated the ischemia/reperfusion (I/R) injury after PP in an in vivo microscopy study of the liver in a rat model [26]. After deflation of the PP, they observed a release of transaminases as well as an increasing number of leukocytes and platelets permanently adherent to the endothelium in all subacinar zones together with activated Kupffer cells indicating microcirculation abnormalities. It has been shown that necrosis of even a few hepatocytes results in a high level of transaminase [29]. Therefore, the elevation of AST and ALT after CO2 PP may be attributed to hepatocellular damage due to intra-abdominal hypertension-induced ischemic injury to the hepatocytes [24, 25, 27]. From the present study, it is clear that elevation of hepatic transaminases can occur after CO2 PP or biliary obstruction. However, these risings of liver enzymes were not significant after laparoscopic insufflation in the jaundice group.
There is limited information on liver histologic changes during PP. The consequence of the histologic changes in humans appears to be clinically nonsignificant because the hemodynamic changes are completely reversible [30, 31]. An electron microscopy study by Izumi et al. found hepatic vascular endothelium changes after CO2 PP in a murine model [32]. Schachtrupp et al. found low-grade paracentral hypoxic necrosis and moderate sinusoidal leukocyte infiltration after 24 h of CO2 PP in a porcine model [33]. A study by Alexakis et al. showed a time course increase in portal inflammation, intralobular inflammation, edema, sinusoidal dilation, sinusoidal hyperemia, centrilobular dilation, centrilobular hyperemia, pericentrilobular ischemia, and focal lytic necrosis scores in a porcine model [34]. On the other hand, as early as 2 to 3 h after BDL, patches of hepatic necrosis are evident [35]. Kupffer cells adjacent to the necrotic areas are prominent and packed with phagocytic vacuoles and slight congestion of the sinusoids is apparent. Twenty-four hours after ligation, the proximal bile duct remnant is slightly dilated. After 2 to 3 days, dilatation and proliferation of the small intralobular and interlobular bile ducts occur [36]. Proliferation of fibroblasts is seen 7 days after BDL [37]. Later, infiltration by leukocytes and fibrosis occur with continued proliferation of ducts. The current study found liver histomorphology impairment after both CO2 PP and BDL. In HE stained liver samples, OJ and PP each caused sinusoidal congestion and vacuolization in hepatocytes, but this was more severe in the PP-only group 3 than in the OJ-only group 2 and PP applied jaundiced subjects (group 4), indicating that ischemia or anoxia occurs during CO2 PP [34]. These changes indicate hepatic tissue damage. However, there were no significant differences between the OJ-only group 2 and PP applied jaundiced subjects (group 4) in terms of sinusoidal congestion and vacuolization. Up to 30% necrosis was seen in three rats in group 2, in two rats in group 3, and in two rats in group 4. In addition, apoptosis was seen in two rats in group 4. In terms of necrosis, however, there were no significant differences between any of the groups. Bile duct proliferation was observed only in the OJ groups (groups 2 and 4). Addition of the PP to the OJ did not affect the mean bile duct proliferation value, but severe ductal proliferation was seen only in PP applied jaundiced subjects (group 4).
The role of elevated intra-abdominal pressure generated by the PP in hepatic function and cell-conveyed immune response is well established. Several studies have showed that there is a direct correlation between portal blood flow changes and immediate effects on liver clearance function and phagocytic activity [38, 39]. Local defense and immune mechanisms might be suppressed by the altered pH during CO2 insufflation. Macrophages, for example, exhibit less phagocytic activity under acidic conditions [40]. In a study reported by Gutt et al., phagocytic activity in the liver was analyzed during laparoscopy and laparotomy in a rat model. They found a decreased antigen elimination during CO2 PP [41]. On the other hand, biliary obstruction in the rats results in a significant depression of the reticuloendothelial system phagocytic function, which may cause impaired systemic bacterial clearance and is associated with decreased survival following Escherichia coli endotoxemia [42]. In our study, we observed that leukocyte counts were decreased in both OJ-only group 2 and PP-only group 3. However, the white blood cell count in PP applied jaundiced subjects (group 4) was not significantly decreased in comparison to the OJ-only group 2. The decrease in white blood cell counts observed in our study might be explained by the same mechanisms. Although we did not measure portal blood flow and Kupffer cell activity, our observation may correlate well with the functional disturbances of the liver observed in our rat model.
MDA is an end product of peroxidative decomposition of polyenic fatty acids in the lipid peroxidation process. The concentration of MDA in liver homogenate is a direct marker for the level of oxygen radicals. There is some evidence that free radicals and lipid peroxides are generated and contribute to the pathogenesis of cholestatic liver injury [8, 43]. Liu et al. demonstrated excessive production of superoxide radicals and hydroxyl radicals in blood and liver in rats with OJ induced by ligation of the CBD [44]. On the other hand, abdominal deflation at the end of a laparoscopic procedure results in the generation of oxygen-derived free radicals, possibly as a result of an I/R phenomenon induced by the inflation and deflation of the PP. ROS provoke severe changes at cellular level leading to cell death, especially the Kupffer and the endothelial cells of the hepatic sinusoids, because of their extreme reactivity [45]. They attack to essential cell constituents, such as proteins, lipids and nucleic acids, and cause the modification of proteins leading to the formation of protein carbonyl groups [46]. Eleftheriadis et al. previously demonstrated that elevated intra-abdominal pressure with a 15-mm Hg CO2 PP for 60 min in rats led to intestinal, spleen, liver, and lung oxygen free radical production [47]. In that study, significant quantities of MDA were released from the intestine, spleen, liver, and lung 30 min after intra-abdominal pressure abolition. We observed an increase in MDA concentrations in the liver tissue of bile duct-ligated rats. The increase in hepatic MDA levels with PP, however, was not significant in the group with OJ. This nonsignificant increase may be due to the short period of obstruction. In the early phase of OJ, antioxidants and free-radical scavengers may compensate for the injury. With prolonged obstruction, the peroxidation level may become high, resulting in liver injury, possibly due to decreased amounts of antioxidants.
GSH, a key antioxidant, is an essential component of the cellular defense mechanism against oxidative stress that induced by ROS. The primary site for de novo GSH synthesis is the liver, which supplies approximately 90% of the circulating plasma GSH [48]. Reduced GSH, which constitutes the main component of endogenous nonprotein sulfhydryl pool, is known to be a major low molecular weight scavenger of free radicals in the cytoplasm [49]. Because of their exposed sulfhydryl groups, nonprotein sulfhydryls bind a variety of electrophilic radicals and metabolites that may be damaging to the cells [50]. Oxidation of hepatic GSH occurs during biliary obstruction. It is possible that free radical generation in the liver is related to an increased oxidative stress in cholestatic rats and could spill over to other organ systems [51]. Huang et al. studied the mitochondrial functions in bile duct-ligated rats and suggested that biochemical and molecular changes are related to oxidative stress in the liver [52]. GSH is protective against postischemic injury by reducing lipid peroxidation. When animals with different preischemic GSH contents subjected to a 90-min of ischemia, followed by a 3-h of reperfusion, it was found that the early postischemic cell death was more extensive in rats with low initial GSH content than in rats with high GSH content [53]. Bickel et al. reported that, in a clinical setting, induction of positive pressure PP during elective laparoscopic cholecystectomy created I/R changes and revealed a decrease in total glutathione level after 30 min of PP termination [54]. In our study, by comparing hepatic GSH content after PP with changes after OJ, it was seen that the effect of PP alone was more severe than its effect after OJ. The decrease in GSH level suggests the same role in protecting the liver during PP. The decrease of GSH content after a long-term insult like OJ might be compensated for and the additional insult of PP might then cause only a nonsignificant reduction in GSH content.
The production of oxygen-derived free radicals by postischemic tissues may contribute to cell damage during I/R injury. The source of free oxygen radicals has been shown to be from xanthine oxidase (XO), an important enzyme in purine metabolism. XO has a role in free radical metabolism and catalyzes the conversion reaction of hypoxanthine to xanthine. In the presence of adequate purine substrate and oxygen, XO generates reactive oxygen metabolites such as superoxide anion (O -2 ), hydrogen peroxide (H2O2), and hydroxyl radical (OH). The use of scavengers of superoxide and hydroxyl radicals, such as SOD, has been suggested to alleviate the problem of oxidative injury in various tissues. Recent studies suggest that disturbance of the oxidant–antioxidant balance might be responsible for cholestatic liver injury and that SOD enzymatic activity is hepatoprotective and play important roles in preventing oxidative stress [55]. The dismutation of free oxygen radicals with SOD leads to the creation of H2O2. H2O2 plays an important role as a free radical with different intra-abdominal pressures during CO2 PP [56]. The activity of SOD would decrease after oxygen radicals are cleaned in liver tissues, indicating that the number of oxygen radicals is increased after CO2 PP [57]. In our study, compared with the jaundice-only group 2, the PP applied group with jaundice (group 4) had not significant changes in the SOD activity. The decreased activity of SOD may be a sign that it had been used to scavenge free radicals in injured liver tissues. But the change in SOD activity was not correlated with the changes in GSH level. Further studies are needed to elucidate these findings.
Conclusion
In summary, the study was designed to be as clinically relevant as possible. To our knowledge no published reports have addressed the effect of PP after BDL. Alterations in hepatic function occur in PP applied jaundiced subjects. However, there were no statistically significant differences between the groups 2 and 4 with regard to white blood cell and platelet counts, serum liver enzymes including AST, ALT, and total bilirubin values, MDA and GSH levels and SOD activity of liver homogenate, and histologic damage. Our results indicate that there is no additional risk on liver function associated with PP performed in OJ. Despite experimental studies have proven to be useful, clinical studies are needed to test these findings in the clinical setting.
References
Neugebauger E, Troidl H, Kum CK et al (1995) The E.A.E.S. Consensus Development Conferences on laparoscopic cholecystectomy, appendectomy, and hernia repair. Consensus statements—September 1994. The Educational Committee of the European Association for Endoscopic Surgery. Surg Endosc 9:550–563
Holthausen UH, Nagelschmidt M, Troidl H (1999) CO2 pneumoperitoneum: what we know and what we need to know. World J Surg 23:794–800
Steinman M, da Silva LE, Coelho IJ et al (1998) Hemodynamic and metabolic effects of CO2 Pneumoperitoneum in an experimental model of hemorrhagic shock due to retroperitoneal hematoma. Surg Endosc 12:416–420
Ozmen MM, Col C, Aksoy AM et al (1999) Effect of CO2 insufflation on bacteremia and bacterial translocation in an animal model of peritonitis. Surg Endosc 13:801–803
Eleftheriadis E, Kotzampassi K, Botsios D et al (1996) Splanchnic ischemia during laparoscopic cholecystectomy. Surg Endosc 10:324–326
Kountouras J, Billing BH, Scheuer PJ (1984) Prolonged bile duct obstruction: a new experimental model for cirrhosis in the rat. Br J Exp Pathol 65:305–311
Krähenbühl S, Talos C, Lauterburg BH et al (1995) Reduced antioxidative capacity in liver mitochondria from bile duct ligated rats. Hepatology 22:607–612
Sokol RJ, Devereaux M, Khandwala R et al (1993) Evidence for involvement of oxygen free radicals in bile acid toxicity to isolated rat hepatocytes. Hepatology 17:869–881
Dahm LJ, Hewett JA, Roth RA (1988) Bile and bile salts potentiate superoxide anion release from activated, rat peritoneal neutrophils. Toxicol Appl Pharmacol 95:82–92
Deitch EA (1990) The role of intestinal barrier failure and bacterial translocation in the development of systemic infection and multiple organ failure. Arch Surg 125:403–404
Clements WD, Parks R, Erwin P et al (1996) Role of the gut in the pathophysiology of extrahepatic biliary obstruction. Gut 39:587–593
Johnstone JM, Lee EG (1976) A quantitative assessment of the structural changes in the rat’s liver following obstruction of the common bile duct. Br J Exp Pathol 57:85–94
Miyoshi H, Rust C, Roberts PJ et al (1999) Hepatocyte apoptosis after bile duct ligation in the mouse involves Fas. Gastroenterology 117:669–677
Bataller R, Schwabe RF, Choi YH et al (2003) NADPH oxidase signal transduces angiotensin II in hepatic stellate cells and is critical in hepatic fibrosis. J Clin Invest 112:1383–1394
Abe T, Arai T, Ogawa A et al (2004) Kupffer cell-derived interleukin 10 is responsible for impaired bacterial clearance in bile duct-ligated mice. Hepatology 40:414–423
Georgiev P, Navarini AA, Eloranta JJ et al (2007) Cholestasis protects the liver from ischaemic injury and post-ischaemic inflammation in the mouse. Gut 56:121–128
Mihara M, Uchiyama M (1978) Determination of malonaldehyde precursor in tissues by thiobarbituric acid test. Anal Biochem 86:271–278
Ellman G (1959) Tissue sulfhydryl groups. Arch Biochem Biophys 82:70–77
Lowry OH, Rosebrough NJ, Farr AL et al (1951) Protein measurement with the Folin phenol reagent. J Biol Chem 193:265–275
Sun Y, Oberley LW, Li Y (1988) A simple method for clinical assay of superoxide dismutase. Clin Chem 34:497–500
Suzuki S, Toledo-Pereyra LH, Rodriguez FJ et al (1993) Neutrophil infiltration as an important factor in liver ischemia and reperfusion injury. Modulating effects of FK506 and cyclosporine. Transplantation 55:1265–1272
Ishizaki Y, Bandai Y, Shimomura K et al (1993) Changes in splanchnic blood flow and cardiovascular effects following peritoneal insufflation of carbon dioxide. Surg Endosc 7:420–423
Volpino P, Cangemi V, D’Andrea N et al (1998) Hemodynamic and pulmonary changes during and after laparoscopic cholecystectomy. A comparison with traditional surgery. Surg Endosc 12:119–123
Andrei VE, Schein M, Margolis M et al (1998) Liver enzymes are commonly elevated following laparoscopic cholecystectomy: is elevated intraabdominal pressure the cause? Dig Surg 15:256–259
Morino M, Giraudo G, Festa V (1998) Alterations in hepatic function during laparoscopic surgery. An experimental clinical study. Surg Endosc 12:968–972
Nickkholgh A, Barro-Bejarano M, Liang R et al (2008) Signs of reperfusion injury following CO2 pneumoperitoneum: an in vivo microscopy study. Surg Endosc 22:122–128
Saber AA, Laraja RD, Nalbandian HI et al (2000) Changes in liver function tests after laparoscopic cholecystectomy: not so rare, not always ominous. Am Surg 66:699–702
Sato K, Kawamura T, Wakusawa R (2000) Hepatic blood flow and function in elderly patients undergoing laparoscopic cholecystectomy. Anesth Analg 90:1198–1202
Omari A, Bani-Hani KE (2007) Effect of carbon dioxide pneumoperitoneum on liver function following laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech, Part A 17:419–424
Gutt C, Schmandra T (1999) Portal venous flow during CO2 pneumoperitoneum in the rat. Surg Endosc 13:902–905
Jakimowicz J, Stultiens G, Smulders F (1998) Laparoscopic insufflation of the abdomen reduces portal venous flow. Surg Endosc 12:129–132
Izumi K, Ishikawa K, Shiroshita H et al (2005) Morphological changes in hepatic vascular endothelium after carbon dioxide pneumoperitoneum in a murine model. Surg Endosc 19:554–558
Schachtrupp A, Toens C, Hoer J et al (2002) A 24-h pneumoperitoneum leads to multiple organ impairment in a porcrine model. J Surg Res 106:37–45
Alexakis N, Gakiopoulou H, Dimitriou C et al (2008) Liver histology alterations during carbon dioxide pneumoperitoneum in a porcine model. Surg Endosc 22:415–420
Cameron GR, Oakley CL (1932) Ligation of the common bile duct. J Pathol Bacteriol 35:769–798
Trams EG, Symeonidis A (1957) Morphologic and functional changes in the livers of rats after ligation or excision of the common bile duct. Am J Pathol 33:13–27
Zimmermann H, Reichen J, Zimmermann A et al (1992) Reversibility of secondary biliary fibrosis by biliodigestive anastomosis in the rat. Gastroenterology 103:579–589
Andersen MN, Kuchiba K (1970) Measurement of acute changes in liver function and blood flow. Arch Surg 100:541–545
Cardoso JE, Giroux L, Kassissia I et al (1994) Liver function improvement following increased portal blood flow in cirrhotic rats. Gastroenterology 107:460–467
Bendet N, Morozov V, Lavi R et al (1999) Does laparoscopic cholecystectomy influence peri-sinusoidal cell activity? Hepatogastroenterology 46:1603–1606
Gutt CN, Heinz P, Kaps W et al (1997) The phagocytosis activity during conventional and laparoscopic operations in the rat. A preliminary study. Surg Endosc 11:899–901
Holman JM Jr, Rikkers LF (1982) Biliary obstruction and host defense failure. J Surg Res 32:208–213
Parola M, Leonarduzzi G, Robino G et al (1996) On the role of lipid peroxidation in the pathogenesis of liver damage induced by long-standing cholestasis. Free Radic Biol Med 20:351–359
Liu TZ, Lee KT, Chern CL et al (2001) Free radical-triggered hepatic injury of experimental obstructive jaundice of rats involves overproduction of proinflammatory cytokines and enhanced activation of nuclear factor κB. Ann Clin Lab Sci 31:383–390
Glantzounis GK, Tselepis AD, Tambaki AP et al (2001) Laparoscopic surgery-induced changes in oxidative stress markers in human plasma. Surg Endosc 15:1315–1319
Halliwell B (1991) Reactive oxygen species in living systems: source, biochemistry, and role in human disease. Am J Med 91:14–22
Eleftheriadis E, Kotzampassi K, Papanotas K et al (1996) Gut ischemia, oxidative stress, and bacterial translocation in elevated abdominal pressure in rats. World J Surg 20:11–16
Sciuto AM (1997) Antioxidant properties of glutathione and its role in tissue protection. In: Baskin SI, Salem H (eds) Oxidants, antioxidants, and free radicals. Taylor and Francis, Washington, pp 171–191
Ross D (1988) Glutathione, free radicals and chemotherapeutic agents. Mechanisms of free-radical induced toxicity and glutathione-dependent protection. Pharmacol Ther 37:231–249
Szabo S, Nagy L, Plebani M (1992) Glutathione, protein sulfhydryls and cysteine proteases in gastric mucosal injury and protection. Clin Chim Acta 206:95–105
Ramachandran A, Balasubramanian KA (2001) Intestinal dysfunction in liver cirrhosis: Its role in spontaneous bacterial peritonitis. J Gastroenterol Hepatol 16:607–612
Huang YT, Hsu YC, Chen CJ et al (2003) Oxidative-stress-related changes in the livers of bile-duct-ligated rats. J Biomed Sci 10:170–178
Jennische E (1984) Possible influence of glutathione on postischemic liver injury. Acta Pathol Microbiol Immunol Scand A 92:55–64
Bickel A, Drobot A, Aviram M et al (2007) Validation and reduction of the oxidative stress following laparoscopic operations: a prospective randomized controlled study. Ann Surg 246:31–35
Roeb E, Purucker E, Gartung C et al (2003) Effect of glutathione depletion and hydrophilic bile acids on hepatic acute phase reaction in rats with extrahepatic cholestasis. Scand J Gastroenterol 38:878–885
Sare M, Yilmaz I, Hamamci D et al (2000) The effect of carbon dioxide pneumoperitoneum on free radicals. Surg Endosc 14:649–652
Xu GS, Liu HN, Li J et al (2009) Hepatic injury induced by carbon dioxide pneumoperitoneum in experimental rats. World J Gastroenterol 15:3060–3064
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bostanci, E.B., Yol, S., Teke, Z. et al. Effects of carbon dioxide pneumoperitoneum on hepatic function in obstructive jaundice: an experimental study in a rat model. Langenbecks Arch Surg 395, 667–676 (2010). https://doi.org/10.1007/s00423-009-0577-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-009-0577-6