Abstract
Background:
Liver metastasis is an important prognostic factor in advanced colorectal cancer. Several studies have demonstrated that carbon dioxide (CO2) pneumoperitonem enhances liver metastasis in an animal model. In the present study, we used scanning electron microscopy (SEM) to investigate morphological changes in hepatic vascular endothelium after CO2 pneumoperitoneum in a murine model.
Methods:
Thirty-three male BALB/c mice were randomized to undergo pneumoperitoneum (CO2, air, or helium ), open laparotomy, and anesthesia alone. After each procedure, the animals’ livers were excised at days 0, 1, and 3 and examined by SEM.
Results:
In the CO2 pneumoperitoneum group, we observed rough surface and derangement of the hepatic vascular endothelial cells and intercellular clefts on day 1. In the other groups, no major morphologic changes were observed at any time.
Conclusions:
Hepatic vascular endothelium changes after CO2 pneumoperitoneum. Such characteristic changes may play an important role in establishing liver metastasis after CO2 pneumoperitoneum.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopic surgery yields favorable short-term clinical outcomes in the management of colorectal malignancies. As a less invasive alternative to open surgery, it has been shown to be technically feasible and to improve patient comfort. There have been few reports, however, on long-term outcomes.
Liver metastasis is the most important prognostic factor in advanced colorectal cancer. Therefore, the effects of pneumoperitoneum on liver metastasis of colorectal cancer have been a matter of cancer. Several experimental studies have shown that carbon dioxide (CO2) pneumoperitoneum enhances liver metastasis [4, 5, 6, 7]. Carbon dioxide pneumoperitoneum causes a decrease in portal blood flow [13, 18, 19] and provides favorable conditions for the adherence of free tumor cells, which can then spread into the portal system, to the hepatic vascular endothelium. However, it is uncertain whether morphological changes occur in the hepatic vascular endothelium after surgical procedures such as the CO2 pneumoperitoneum or open laparotomy.
In the present study, we used a murine pneumoperitoneum model to investigate morphological changes in hepatic vascular endothelium by scanning electron microscopy (SEM).
Materials and methods
Animals
Thirty-three male BALB/c mice weighting 20-24 g and aged 6-8 weeks were used in this study. All animals were kept under standard laboratory conditions (temperature, 20-24°C; relative humidity, 50-60%; 12 h light/dark cycles) and given a standard laboratory diet with free access to water and food. All experiments were performed under the guidelines for animal experimentation of the Oita University Faculty of Medicine.
Procedures
All surgical procedures were performed under general anesthesia induced by diethyl ether inhalation. Thirty-three BALB/c mice were divided into three operative groups; pneumoperitoneum, laparotomy, and anesthesia only (control).
In the pneumoperitoneum group, nine mice underwent CO2 pneumoperitoneum at 8-10 mmHg for 60 min and were killed after either 0 h (n = 3), 24 h (n = 3), or 72 h (n = 3). In addition, six mice received an air or helium (n = 3 each) pneumoperitoneum at 8-10 mmHg for 60 min and were killed after 24 h. The procedure for establishing the pneumoperitoneum has been described previously [16]. A 22-gauge intravenous cannula was inserted into the left lower quadrant and used as an insufflation needle. A 20-gauge intravenous cannula was inserted into the right lower quadrant and used to measure intraperitoneal pressure. A disposable syringe was used to inject the gas. A syringe pump was used to maintain continuous insufflation, and intraperitoneal pressure was measured as the distance between the right and left water levels in the U-shaped tube.
In the laparotomy group (n = 9), a 3-cm abdominal midline incision was made, and the laparotomy conditions were maintained for 60 min. The mice were killled after either 0 h (n = 3), 24 h (n = 3), or 72 h (n = 3).
The control group (n = 9) underwent only diethyl ether anesthesia for 60 min. The mice were killed after either 0 h (n = 3), 24 h (n = 3), or 72 h (n = 3).
After each procedure, the left lobe of the murine liver was excised, and four samples from each liver were prepared for examination with an SEM. These samples were put into fixative solution composed of 2% formaldehyde and 2.5% glutaraldehyde in 0.05 M cacodylate buffer solution. They were then placed into 1% osmium tetroxide for 60 min, dehydrated stepwise in alcohol, and dried by mens of a critical points apparatus. The dried specimens were mounted on aluminium stubs, spatter-coated with gold, and examined with an SEM (Hitachi S800, Ibaragi, Japan). Photographs of the five areas selected at random in each sample were analyzed.
None of the animals died at any time during this experiment.
Analysis
Following the same procedure used by Suematsu et al. [17], the photographs were evaluated by five independent observers (one histologist, one pathologist, and three surgeons) who were not informed of the procedures used to quantify the results. The following characteristics of the hepatic vascular endothelium were observed: (a) dilatation of intercellular clefts, (b) derangement of the endothelial cells, and (c) a rough surface. We then compared these characteristics with those of normal hepatic vascular endothelium of untreated mice and graded the changes as none or slight (-), moderate (+), or marked (+ +). If over half of the observers were in agreement, the results were adopted. In cases where the observers disagreed about the results, the lower grade was adopted.
Results
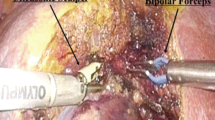
Figure 1 shows the normal hepatic vascular endothelium of untreated mice. Normal liver endothelium is characterized by a smooth surface, a regular arrangement of the endothelial cells that corresponds with the direction of the blood flow, and no intercellular clefts. In the CO2 pneumoperitoneum group (Fig. 2), we observed both derangement of the hepatic vascular endothelial cells and intercellular clefts on day 1. These changes were recognized immediately after creation of the CO2 pneumoperitoneum and persisted 3 days. However, in the air pneumoperitoneum group, the changes were not as marked on day 1 (Fig. 3a). Also, on day 1 after helium pneumoperitoneum, the changes were unremarkable (Fig. 3b). There were also no remarkable changes at any time in the control group or the laparotomy group (Figs. 4 and 5). In the laparotomy group, only the rough surface of endothelium was observed on day 3, but this change was slight as compared with the CO2 pneumoperitoneum group.
In the CO2 pneumoperitoneum group, there were marked changes in the hepatic vascular endothelium. Dilatation of intercellular clefts, irregular arrangement of endothelial cells, and a rough surface were observed. Original magnification, ×2,000. The bar represents 15 μm. a Immediately after CO2 pneumoperitoneum. b Day 1. c Day 3.
Table 1 summarizes the morphological changes in each group. There were no wide disparities among the five observers in grading the results.
Discussion
Laparoscopic surgery has been adopted for colorectal cancer because it is less invasive and yields a better cosmetic result. However, the effects of the pneumoperitoneum on liver metastasis, which is the most important prognostic factor for colorectal cancer, remain unclear. In the present study, we used SEM to investigated the morphologic changes to hepatic vascular endothelial cells that occur after CO2 pneumoperitoneum. Other studies have used SEM to investigate morphological changes to the peritoneum after CO2 pneumoperitoneum [17, 20], but this is the first study to clarify changes to the hepatic vascular endotheliem after CO2 pneumoperitoneum.
The first step in liver metastasis is the adherence of tumor cells to the hepatic vascular endothelium. Thus, injury to the hepatic vascular endothelium may be associated with an increase in the incidence of liver metastasis. In hepatic ischemia-reperfusion injury, the damage to the ischemic lobe creates a favorable condition for liver metastasis or intrahepatic tumor growth [2], and the expression of adhesion molecules promotes the establishment of liver metastasis.
Several studies have previously shown that the intraabdominal insufflation of CO2 causes a marked and rapid decrease (35% to 84%) in portal blood flow [8, 12, 14]. This reduction correlates with the degree of intraabdominal pressure, and may be caused by either mechanical compression of the thin-walled portal vein or hypercapnia-induced vasoconstriction; by contrast, the hepatic arterial flow appears to be less compromised. In this study, intraabdominal pressure was kept at 8-10 mmHg after insufflation in the pneumoperitoneum group. This high level of intraabdominal pressure must influence portal blood flow, and it may serve to induce hepatic ischemia after creation of the pneumoperitoneum.
In the CO2 pneumoperitoneum group, we observed distinct morphological changes to the hepatic vascular endothelium, including (a) dilatation of intercellular clefts, (b) irregular arrangement of the endothelial cells, and (c) a rough surface. On day 1 after CO2 pneumoperitoneum, these changes were remarkable. However, on day 1 after air and helium pneumoperitoneum, the changes to the hepatic vascular endothelium were comparatively slight. Our results suggest that these morphological changes are caused not only by the reduction in portal blood flow induced by intraabdominal high pressure but also by the CO2 itself.
Shuto et al. [15] have shown that metabolic acidosis occurs after both helium and CO2 pneumoperitoneum, but hypercapnia occurs only after CO2 pneumoperitoneum. Furthermore, several studies have shown that whereas helium pneumoperitoneum does not cause either hypercapnia or acidic changes, CO2 pneumoperitoneum induces both hypercapnia and acidosis[1, 3, 9, 10, 11]. Therefore, morphological changes to the hepatic vascular endothelium may be a result of a combination of CO2 absorption and the hepatic ischemia induced by the CO2 pneumoperitoneum.
In conclusion, morphological changes to the hepatic vascular endothelium occur after CO2 pneumoperitoneum. Clinical studies are needed to investigate whether these changes are associated with the enhancement of liver metastasis after laparoscopic colorectal surgery.
References
MR Brackman FC Finelli T Light O Llorente K McGill J Kirkpatrick (2003) ArticleTitleHelium pneumoperitoneum ameliorates hypercarbia and acidosis associated with carbon dioxide insufflation during laparoscopic gastric bypass in pigs Obes Surg 13 768–771 Occurrence Handle10.1381/096089203322509363 Occurrence Handle14627474
K Doi T Horiuchi M Uchinami T Tabo N Kimura J Yokomachi M Yoshida et al. (2002) ArticleTitleHepatic ischemia-reperfusion promotes liver metastasis of colon cancer J Surg Res 105 243–247 Occurrence Handle10.1006/jsre.2002.6356 Occurrence Handle1:CAS:528:DC%2BD38XltFSktrw%3D Occurrence Handle12121713
SD Fitzgerald CH Andrus LJ Baudendistel TE Dahms DL Kaminski (1992) ArticleTitleHypercarbia during carbon dioxide pneumoperitoneum Am J Surg 163 186–190 Occurrence Handle10.1016/0002-9610(92)90274-U Occurrence Handle1:STN:280:By2C38rmtFA%3D Occurrence Handle1733368
CN Gutt ZG Kim T Schmandra V Paolucci M Lorenz (2000) ArticleTitleCarbon dioxide pneumoperitoneum is associated with increased liver metastases in a rat model Surgery 127 566–570 Occurrence Handle10.1067/msy.2000.105029 Occurrence Handle1:STN:280:DC%2BD3c3nvFSgug%3D%3D Occurrence Handle10819066
CN Gutt V Riemer ZG Kim J Erceg M Lorenz (2001) ArticleTitleImpact of laparoscopic surgery on experimental hepatic metastases Br J Surg 88 371–375 Occurrence Handle10.1046/j.1365-2168.2001.01700.x Occurrence Handle1:STN:280:DC%2BD3M7mtVaqtA%3D%3D Occurrence Handle11260101
H Ishida Y Idezuki M Yokoyama H Nakada A Odaka N Murata M Fujioka et al. (2001) ArticleTitleLiver metastasis following pneumoperitoneum with different gases in a mouse model Surg Endosc 15 189–192 Occurrence Handle10.1007/s004640000312 Occurrence Handle1:STN:280:DC%2BD3Mvit1Ggtw%3D%3D Occurrence Handle11285965
H Ishida N Murata Y Idezuki (2001) ArticleTitle) Increased insufflation pressure enhances the development of liver metastasis in a mouse laparoscopy model World J Surg 25 1537–1541 Occurrence Handle1:STN:280:DC%2BD38%2FkvVWisg%3D%3D Occurrence Handle11775187
J Jakimowicz G Stultiens F Smulders (1998) ArticleTitleLaparoscopic insufflation of the abdomen reduces portal venous flow Surg Endosc 12 129–132 Occurrence Handle10.1007/s004649900612 Occurrence Handle1:STN:280:DyaK1c7ktVemsQ%3D%3D Occurrence Handle9479726
T Leighton N Pianim SY Liu M Kono S Klein F Bongard (1992) ArticleTitleEffectors of hypercarbia during experimental pneumoperitoneum Am Surg 58 717–721 Occurrence Handle1:STN:280:ByyD1cbmvFA%3D Occurrence Handle1456592
TA Leighton SY Liu FS Bongard (1993) ArticleTitleComparative cardiopulmonary effects of carbon dioxide versus helium pneumoperitoneum Surgery 113 527–531 Occurrence Handle1:STN:280:ByyB2MrltFM%3D Occurrence Handle8488470
TJ Neuberger CH Andrus CM Wittgen TP Wade DL Kaminski (1996) ArticleTitleProspective comparison of helium versus carbon dioxide pneumoperitoneum Gastrointest Endosc 43 38–41 Occurrence Handle1:STN:280:ByiD2MbkvFE%3D Occurrence Handle8903816
M Schafer L Krahenbuhl (2001) ArticleTitleEffect of laparoscopy on intra-abdominal blood flow Surgery 129 385–389 Occurrence Handle10.1067/msy.2001.110224 Occurrence Handle1:STN:280:DC%2BD3M3js1yqtQ%3D%3D Occurrence Handle11283527
TC Schmandra CN Gutt (1998) ArticleTitle[Changes in portal blood flow volume by CO2 pneumoperitoneum in the rat.] Langenbecks Arch Chir Suppl Kongressbd 115 565–569 Occurrence Handle1:STN:280:DC%2BD3svlsleltQ%3D%3D Occurrence Handle14518318
TC Schmandra ZG Kim CN Gutt (2001) ArticleTitleEffect of insufflation gas and intraabdominal pressure on portal venous flow during pneumoperitoneum in the rat Surg Endosc 15 405–408 Occurrence Handle10.1007/s004640000331 Occurrence Handle1:STN:280:DC%2BD38%2Fht1yhsQ%3D%3D Occurrence Handle11395825
K Shuto S Kitano T Yoshida T Bandoh Y Mitarai M Kobayashi (1995) ArticleTitleHemodynamic and arterial blood gas changes during carbon dioxide and helium pneumoperitoneum in pigs Surg Endosc 9 1173–1178 Occurrence Handle10.1007/BF00210922 Occurrence Handle1:STN:280:BymC3s7ovFU%3D Occurrence Handle8553228
T Suematsu A Shiromizu K Yamaguchi N Shiraishi Y Adachi S Kitano (1999) ArticleTitleConvenient murine pneumoperitoneal model for the study of laparoscopic cancer surgery Surg Laparosc Endosc Percutan Tech 9 279–281 Occurrence Handle10.1097/00019509-199908000-00010 Occurrence Handle1:STN:280:DC%2BD3czis12qsA%3D%3D Occurrence Handle10871177
T Suematsu Y Hirabayashi N Shiraishi Y Adachi H Kitamura S Kitano (2001) ArticleTitleMorphology of the murine peritoneum after pneumoperitoneum vs laparotomy Surg Endosc 15 954–958 Occurrence Handle10.1007/s004640090100 Occurrence Handle1:STN:280:DC%2BD3MrlvVCktA%3D%3D Occurrence Handle11443469
S Takagi (1998) ArticleTitleHepatic and portal vein blood flow during carbon dioxide pneumoperitoneum for laparoscopic hepatectomy Surg Endosc 12 427–431 Occurrence Handle10.1007/s004649900696 Occurrence Handle1:STN:280:DyaK1c3ktVKhsQ%3D%3D Occurrence Handle9569363
MJ Tunon P Gonzalez F Jorquera A Llorente M Gonzalo-Orden J Gonzalez-Gallego (1999) ArticleTitleLiver blood flow changes during laparoscopic surgery in pigs: a study of hepatic indocyanine green removal Surg Endosc 13 668–672 Occurrence Handle10.1007/s004649901070 Occurrence Handle1:STN:280:DyaK1Mzhs1eqtg%3D%3D Occurrence Handle10384072
J Volz S Koster Z Spacek N Paweletz (1999) ArticleTitleThe influence of pneumoperitoneum used in laparoscopic surgery on an intraabdominal tumor growth Cancer 86 770–774 Occurrence Handle10.1002/(SICI)1097-0142(19990901)86:5<770::AID-CNCR11>3.0.CO;2-3 Occurrence Handle1:STN:280:DyaK1MzptlChtw%3D%3D Occurrence Handle10463974
Acknowledgment
This study was supported in part by a Grant-in-Aid for Scientific Research (no. 15390401) from the Japanese Ministry of Education, Science, and Culture. We also thank Tatsuo Shimada, Department of Fundamental Nursing, Oita University Faculty of Medicine, for his support of our work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Izumi, K., Ishikawa, K., Shiroshita, H. et al. Morphological changes in hepatic vascular endothelium after carbon dioxide pneumoperitoneum in a murine model. Surg Endosc 19, 554–558 (2005). https://doi.org/10.1007/s00464-004-9081-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-004-9081-9