Abstract
Background
Although CO2 is the insufflation gas of choice in laparoscopic procedures, room air is usually used in natural orifice transluminal endoscopic surgery. The aim of the present study was to compare the safety of room air versus CO2 pneumoperitoneum in terms of their effect on the oxidative state, apoptosis and tissue injury of splanchnic organs.
Methods
Eighteen Wistar rats were assigned to three groups (n = 6 per group) and were subjected to 8 mm Hg room air (group Pne-Air) or CO2 pneumoperitoneum (group Pne-CO2) or sham operation for 60 min. Forty-five minutes postdeflation, tissue samples were excised from the liver, stomach, ileum and kidneys for reduced glutathione-to-glutathione disulfide (GSH/GSSG) ratio, caspase-8 and caspase-3 and hypoxia-inducible factor-1α (HIF-1α) immunohistochemical assessment and histopathologic examination.
Results
GSH/GSSG ratio substantially declined in both pneumoperitoneum groups. No change was noted in HIF-1α expression. Mild upregulation of caspase-8 and caspase-3 was noted in both pneumoperitoneum groups being less pronounced in group Pne-Air. Histopathologic score was increased in all organs studied, but the stomach, in both pneumoperitoneum groups.
Conclusion
Pneumoperitoneum established by either room air or CO2 induced substantial oxidative stress, mild apoptosis and mild tissue injury in splanchnic organs. While air pneumoperitoneum conferred a less pronounced apoptotic effect, the oxidative state and histopathologic profile of splanchnic organs did not differ between insufflation gases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Natural orifice transluminal endoscopic surgery (NOTES) is a revolutionary method of minimally invasive surgery that combines endoscopy with laparoscopy to perform diagnostic and therapeutic procedures on splanchnic organs via natural orifices (mouth, urethra, vagina or anus). The method is performed using rigid or flexible endoscopes that facilitate the establishment of pneumoperitoneum and the insertion of standard or specially designed endoscopic instruments through their working channels into the abdominal cavity. Standard endoscopes are designed to insufflate hollow organs under inspection with room air in order to optimize their visualization, facilitate advancement of the endoscope and gain working space. For practical reasons, pneumoperitoneum in NOTES procedures is usually created by insufflation of room air, although carbon dioxide (CO2) is considered the insufflation gas of choice in laparoscopic procedures [1].
Nevertheless, CO2 pneumoperitoneum has been shown to induce oxidative stress [2, 3]. There is evidence that this effect is attributed not only to high intraabdominal pressure but also to the type of the insufflation gas used [3]. Systemic absorption of CO2 leads to increased pCO2 and decreased systemic pH with subsequent visceral vasoconstriction and reduction in splanchnic organs’ blood flow [4]. With deflation, this ischemia–reperfusion insult promotes tissue oxidative stress which is a key triggering factor of apoptosis and hence tissue injury [5].
Given that room air tends to be used in NOTES procedures, the issue of its safety compared to CO2 pneumoperitoneum is currently under debate. The aim of the present study was to compare the safety of room air against CO2 pneumoperitoneum in terms of their effects on the oxidative state, apoptosis and the tissue damage of splanchnic organs in a rat model.
Materials and methods
Animals
Eighteen male Wistar rats, 4 months of age, weighing 300–350 g, provided from our laboratory’s rat colony, were used. They were housed in polycarbonate cages, three rats per cage, at 20–22 °C room temperature, on a 12:12-h light/dark cycle, and were provided with commercial pelleted diet and tap water ad libitum.
Experimental design
Animals were assigned to three groups of six rats each and were subjected to 8 mm Hg room air pneumoperitoneum (group Pne-Air), 8 mm Hg CO2 pneumoperitoneum (group Pne-CO2) or sham operation (group Sham) for 60 min. Forty-five minutes postdeflation, tissue samples were excised under general anesthesia from the liver, stomach, ileum and kidneys for oxidative state and apoptosis assessment and histopathologic examination. Finally, the animals were euthanized by exsanguination. The experimental protocol was approved by the Animal Care and Use Committee of the local veterinary service (License number Τ/701/17-3-2010) since it complied with the requirements set by the Directive 86/609/EEC and the PD 160/91 which was the legislation in force at the time of experimentation.
Animal preparation
Animals were anesthetized by intraperitoneal injection of ketamine (90 mg/kg) and placed at a supine position on a heated-surface operation table. After proper preparation of the surgical field (clipping of the abdomen and disinfection with 10 % povidone iodine solution), a 21G intravenous catheter was inserted intraabdominally through the umbilicus, connected to a insufflator tube and inflated the abdominal cavity with either room air (group Pne-Air) or CO2 (group Pne-CO2) up to a 8-mm Hg intraabdominal pressure for a 60-min period (Insufflator for Laparoscopy, Lemke Vision F103, World of Medicine A.G., Ludwigsstadt, Germany). Another 21G intravenous catheter was inserted intraabdominally through the midline to facilitate relief of gas and equilibration of intraabdominal pressure. No gas was insufflated in group Sham.
Oxidative state assessment
Tissue oxidative state was assessed on the basis of reduced glutathione-to-glutathione disulfide ratio (GSH/GSSG). The concentrations (µM) of GSH and GSSG were measured in tissues using a commercially available kit (GSH/GSSG Ratio Assay Kit, CALBIOCHEM, San Diego, CA) according to the manufacturer’s instructions. The assay utilizes glutathione reductase and allows quantitative assessment of GSSG by the use of the thiol-scavenging reagent 1-methyl-2-vinylpyridinium trifluoromethane sulfonate (M2VP, US Patent 5,543,298) that rapidly scavenges GSH without interfering with the glutathione reductase assay. Ileal segments, approximately 5 cm long, were excised and opened longitudinally to expose the mucosal epithelium which was rinsed with ice-cold normal saline (0.9 % NaCl). The mucosal layer was then harvested by gentle scraping of the epithelium with a glass slide. Tissue specimens were also harvested from the liver, kidneys and stomach. Homologous pieces of each tissue (weighing approximately 10 mg) were collected in pairs of preweighed Eppendorf tubes. One tube was empty, while the other contained the scavenger M2VP. The samples were homogenized therein before being snap-frozen in liquid nitrogen and stored at −75 °C until later analyzed. The tube which did not contain the scavenger was meant for quantification of GSH concentration, while the other was meant for quantification of GSSG concentration. The assay was performed measuring the rate of optical density change of 5,5′-dithiobis-(2-nitrobenzoic acid) (DTNB) used as a chromophore at 412 nm (DOD412/min). For each pair of homologous samples, the levels of GSH and GSSG were determined by reference to standard corresponding concentrations of GSH (supplied by the manufacturer) and were recalculated per mg of protein content of the corresponding samples. Finally, the GSH/GSSG ratio was calculated according to the formula: ratio = [(GSH)-2(GSSG)]/(GSSG).
Histopathology: immunohistochemistry
Tissue specimens excised from the liver, ileum, stomach and kidneys were fixed in 10 % formalin solution and embedded in paraffin according to standard procedures. Histopathologic examination was performed in 4 µm hematoxylin–eosin-stained sections under a Nikon Eclipse 50i microscope (Nikon/Kawasaki, Japan). The histopathologic endpoints evaluated for each organ tissue were the following: liver: hyperemia/distension of sinusoidal space, hepatocellular degeneration/steatosis, portal infiltration, necrosis; ileum: (a) mucosa: neutrophil granulocyte infiltration, lymphocyte/plasmacell infiltration, (b) intestinal crypts: hyperplasia, neutrophil granulocyte infiltration, lymphocyte/plasmacell infiltration, (c) stroma: edema, hyperemia, neutrophil granulocyte infiltration, lymphocyte/plasmacell infiltration, (d) submucosa: neutrophil granulocyte infiltration, lymphocyte/plasmacell infiltration, hyperemia/vascular dilatation, (e) serosa/mesenterium: hyperemia/vascular dilatation; stomach: hyperemia, distension, infiltration; kidneys: hyperemia/distension of parenchymal blood vessels, hyperemia/distension of renal corpuscles’ blood vessels, interstitial nephritis, tubular necrosis, perivascular infiltration; Stomach: hyperemia, distension of blood vessels. Severity of lesions was quantified according to the following scoring system: 0, none; 1, mild; 2, moderate; and 3, severe. Lesion severity scores were added to obtain the histopathologic score.
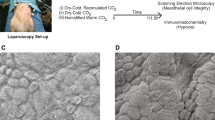
Four-micron (4 µm) sections of representative blocks from each case were obtained for immunohistochemical assessment. They were deparaffinized, rehydrated, and treated with 0.3 % H2O2 for 5 min in methanol to prevent endogenous peroxidase activity and were immunostained using the Chemicon IHC Select Immunoperoxidase secondary detection system (Chemicon International Inc/Temecula, CA, USA). They were then incubated for 60 min with the rabbit polyclonal antibody caspase-3-active (Acris Antibodies, San Diego, CA, USA), the rabbit polyclonal antibody caspase-8 (Acris Antibodies) or the mouse monoclonal antibody hypoxia-inducible factor-1α (HIF-1α, Santa Cruz Biotechnology, Dallas, Texas, USA) at 1:80, 1:80 or 1:250 dilutions, respectively. Control slides were incubated for the same period with nonimmunized rabbit serum (negative control). Positive controls were, also, set up during the process. Βound antibody complexes were stained for 10 min with freshly prepared 0.05 % diaminobenzidine (DAB). Sections were then briefly counterstained with Mayer’s hematoxylin, mounted, and examined under a Nikon Eclipse 50i microscope. Caspase-3, caspase-8 and HIF-1α tissue expression was graded in terms of density and extent of presence of positively stained cells in the entire slide, according to the following scoring system: 0, absence; 1, low; 2, moderate; and 3, high. The score for each histopathologic and immunohistochemical parameter was the average of scores obtained by two independent operators.
Statistical analysis
Before the beginning of the study, a sample size calculation was performed with 80 % power and α error set at 0.01 (two-sided). We estimated that a maximum of 6 rats per group would be required to detect a difference of 12 in GSH/GSSG ratio, 0.3 in caspase-8 expression score and 1.4 in histopathologic score with 10.0, 0.2 and 1.0 standard deviations, respectively. Data were expressed as means ± standard deviation. After normality of data was tested with the Kolmogorov–Smirnov test, those were subjected to analysis of variance (ANOVA). The Bonferroni test was used for multiple comparisons among groups. A p < 0.05 was considered statistically significant.
Results
All animals survived during the experimental period.
Oxidative state
Severe oxidative stress was induced in both pneumoperitoneum groups, as evidenced by a substantial decrease in GSH/GSSG ratio, in all organs studied. However, no difference was noted between pneumoperitoneum groups (Fig. 1).
HIF-1α
No significant changes in HIF-1α tissue expression were noted among groups in all tissues studied (data not shown).
Apoptosis
Immunohistochemical analysis revealed a mild upregulation of apoptosis markers in both pneumoperitoneum groups. Mild upregulation of caspase-8 expression was noted in both pneumoperitoneum groups in the liver, ileum and stomach, while it was noted only in group Pne-CO2 in the kidneys (Fig. 2). Expression score was lower in group Pne-Air compared to Pne-CO2 in the ileal tissue (Fig. 3). Μild upregulation of caspase-3 expression was also noted in both pneumoperitoneum groups in the liver, ileum and stomach, but not the kidneys. Expression score was lower in group Pne-Air compared to group Pne-CO2 in the ileal and stomach tissue (Fig. 4).
Representative caspase-8, caspase-3 and hematoxylin–eosin-stained slides from liver, kidneys, ileum and stomach tissues following room air (group Pne-Air) or CO2 pneumoperitoneum (group Pne-CO2). Caspase-8: mild expression in all organs; caspase-3: mild expression in liver, ileum and stomach, absence in kidneys; hematoxylin–eosin: liver, mild hyperemia/distension of sinusoidal space; kidneys, mild hyperemia/distension of parenchymal and renal corpuscles’ blood vessels; ileum, mild inflammatory cell infiltration of all layers and hyperemia of the intestinal crypts; stomach, mild hyperemia and distension of blood vessels
Caspase-8 immunohistochemical tissue expression score (mean, n = 6) following room air pneumoperitoneum (group Pne-Air), CO2 pneumoperitoneum (group Pne-CO2) or sham operation (group Sham). Error bars represent standard deviation. *p < 0.001 versus group Sham, & p < 0.05 versus group Pne-Air, # p < 0.001 versus group Pne-Air
Histopathology
Histopathologic lesions noted in each organ tissue are presented in Table 1. Histopathologic score was increased in both pneumoperitoneum groups in the kidneys and ileum, while only in group Pne-Air in the liver. In specific, the increase was attributed (a) in the kidneys to mild hyperemia/distension of parenchymal and renal corpuscles’ blood vessels, (b) in the ileum to mild inflammatory cell infiltration of all layers and hyperemia of the intestinal crypts, stroma and serosa/mesenterium and (c) in the liver to mild hyperemia/distension of sinusoidal space (Fig. 2). However, no differences were noted between pneumoperitoneum groups. No statistically significant change was noted in the stomach.
Discussion
While CO2 is considered the insufflation gas of choice in laparoscopy, room air is usually used in practice for the establishment of pneumoperitoneum in NOTES procedures. According to the results of the present comparative experimental study, both gases induced substantial oxidative stress, mild apoptosis and mild tissue injury in splanchnic organs. Room air yielded similar side effects to those of CO2 with regard to the oxidative state and histopathologic profile of splanchnic organs, while it had a less pronounced apoptotic effect.
Carbon dioxide is a nonflammable, quickly absorbed and excreted gas whose properties favor it over other gases in standard laparoscopic procedures. Nevertheless, it has been associated with respiratory, hemodynamic and metabolic problems [1]. On the other hand, room air, which is composed of N2 (78 %), O2 (21 %) and Ar (1 %), supports combustion, is slowly absorbed and carries a higher risk of venous embolism [1, 6]. There is accumulating evidence from experimental studies supporting the safe use of room air in laparoscopy. Intraabdominal insufflation of air caused similar cardiorespiratory [7] and peritoneal inflammatory responses to that of CO2 [8], setting under new debate the safety of those gases. Other gases to substitute CO2 in laparoscopic procedures are also under study; these include helium, argon and nitrogen which may increase the risk of venous gas embolism, as well as nitrous oxide which, however, supports combustion [1].
Pneumoperitoneum induces oxidative stress. Increased intraabdominal pressure (>8 mm Hg) in humans alters systemic and local hemodynamics, leading to ischemia of splanchnic organs [3]. In the present project, pneumoperitoneum-induced consequences were evaluated in our rat model at 8 mm Hg intraabdominal pressure which, according to experimental studies, correlates with high working pressures applied to humans [9]. Upon deflation, tissue reperfusion exacerbates oxidative stress-induced tissue injury. In CO2 pneumoperitoneum, there is also a gas-related effect. Extensive systemic absorption of CO2 may lead to hypercapnia and systemic and tissue acidosis with subsequent additional visceral vasoconstriction and reduction in splanchnic organs’ blood flow [4]. This condition places patients with already compromised respiratory and/or cardiac functions under risk since they may not efficiently counterbalance such an effect. It is also associated with tachycardia, cardiac arrhythmias and pulmonary edema. Furthermore, it may cause peritoneal irritation and subsequent postoperative pain, while its use is associated with immunological impairment [10].
Both clinical and animal studies show that CO2 pneumoperitoneum results in marked elevation of oxidative stress biomarkers [2, 3]. GSH/GSSG ratio is considered a sensitive marker of oxidative stress. Glutathione is the main nonenzymatic intracellular antioxidant that acts as a redox buffering system by scavenging reactive oxygen species. The latter are overproduced at oxidative stress and act as potent oxidizing and reducing agents that can directly damage cellular membranes by lipid peroxidation [11]. Peroxidation of endogenous lipids leads to conversion of GSH to GSSG with a decline of their ratio [12]. Tissue GSH/GSSG ratio, malondialdehyde concentration and superoxide dismutase activity were altered in the liver, kidneys, jejunum and stomach following insufflation of CO2 up to a 15-mm Hg intraabdominal pressure in rats [2]. In the present study, 8 mm Hg pneumoperitoneum by either tested gases caused substantial decrease in GSH/GSSG ratio, while there were no differences between insufflation gases.
The role of splanchnic ischemia–reperfusion on the effects noted was evaluated by assessing the expression of HIF-1α, a tissue oxygen deprivation marker. HIF transcription factors play an integral role in the metabolic changes that drive cellular adaptation to low oxygen availability [13]. According to our results, tissue expression of HIF-1α was not altered, highlighting the role of the insufflating gas per se on the side effects noted and making comparison between gases more objective.
Oxidative stress plays a pivotal role in apoptosis [5]. Reactive oxygen species and the resulting cellular redox change can be part of the signal transduction pathway during apoptosis. Caspases are a family of cysteine proteases that are central regulators of apoptosis. Upon receipt of apoptotic stimuli, cells activate initiator caspases, such as caspase-2, 8, 9 and 10, that proteolytically cleave and activate downstream effector caspases, such as caspase-3, 6 and 7. These, in turn, cleave a range of substrates, leading to the dismantling of the dying cell [14]. In the present study, induction of apoptosis was evidenced by mild upregulation of caspase-8 and caspase-3, reliable biomarkers of the early events of apoptosis, in the liver, ileum, stomach and kidneys. In the air pneumoperitoneum group, this effect was less prominent in the liver, ileum and stomach, while absent in the kidneys. Since equal intraperitoneal pressures, exerting the same mechanical effect on splanchnic organs, were applied in both study groups, the aforementioned differentiation represented a gas-related effect. Subsequently, pneumoperitoneum caused histopathologically evidenced mild tissue injury in the liver, ileum and kidneys, but not in the stomach, with no differences between insufflation gases.
Strategies to prevent a pneumoperitoneum-induced oxidative stress response and subsequent consequences are under investigation and have promising results. These include ischemic preconditioning [15], establishment of low intraabdominal pressure [16], insufflation with the inert gas helium [17], and pretreatment with erythropoietin [18] or the antioxidants melatonin [19] and mesna [2]. Furthermore, the issue of uncontrolled high intraabdominal pressures that could lead to adverse hemodynamic effects should be avoided in NOTES procedures. This could be accomplished by connecting a gas pressure monitoring system directly to the endoscope [20] or to a Veress needle that would deliver the insufflation gas transdermally [21]. Taking into account the property of room air in supporting combustion, safe use of this insufflating gas should be limited in laparoscopy or laparoscopic procedures that do not require electrocautery.
In conclusion, intraperitoneal insufflation with room air conferred similar effects with those of CO2 regarding pneumoperitoneum-induced oxidative stress and histopathologic lesions of splanchnic organs, while it had a less pronounced effect on apoptosis. These findings add novel evidence regarding the safety of these gases that should be taken into consideration when used in laparoscopic or NOTES procedures.
References
Menes T, Spivak H (2000) Laparoscopy: searching for the proper insufflation gas. Surg Endosc 14:1050–1056
Ypsilantis P, Tentes I, Anagnostopoulos K, Kortsaris A, Simopoulos C (2009) Mesna protects splanchnic organs from oxidative stress induced by pneumoperitoneum. Surg Endosc 23:583–589
Sammour T, Mittal A, Loveday BP, Kahokehr A, Phillips AR, Windsor JA, Hill AG (2009) Systematic review of oxidative stress associated with pneumoperitoneum. Br J Surg 96:836–850
Grabowski JE, Talamini MA (2009) Physiological effects of pneumoperitoneum. J Gastrointest Surg 13:1009–1016
Kannan K, Jain SK (2000) Oxidative stress and apoptosis. Pathophysiology 7:153–163
Swanström LL (2009) Natural orifice transluminal endoscopic surgery. Endoscopy 41:82–85
von Delius S, Sager J, Feussner H, Wilhelm D, Thies P, Huber W, Schuster T, Schneider A, Schmid RM, Meining A (2010) Carbon dioxide versus room air for natural orifice transluminal endoscopic surgery (NOTES) and comparison with standard laparoscopic pneumoperitoneum. Gastrointest Endosc 72:161–169
Trunzo JA, McGee MF, Cavazzola LT, Schomisch S, Nikfarjam M, Bailey J, Mishra T, Poulose BK, Lee YJ, Ponsky JL, Marks JM (2010) Peritoneal inflammatory response of natural orifice translumenal endoscopic surgery (NOTES) versus laparoscopy with carbon dioxide and air pneumoperitoneum. Surg Endosc 24:1727–1736
Avital S, Itah R, Szomstein S, Rosenthal R, Inbar R, Sckornik Y, Weinbroum A (2009) Correlation of CO2 pneumoperitoneal pressures between rodents and humans. Surg Endosc 23:50–54
Cheng Y, Lu J, Xiong X, Wu S, Lin Y, Wu T, Cheng N (2013) Gases for establishing pneumoperitoneum during laparoscopic abdominal surgery. Cochrane Database Syst Rev 1:CD009569
Toyokuni S (1999) Reactive oxygen species-induced molecular damage and its application in pathology. Pathol Int 49:91–102
Brivida K, Sies H (1994) Non enzymatic antioxidant defense system. In: Frei B (ed) Natural antioxidants in human health and disease. Academic Press, San Diego, pp 107–128
Palazon A, Goldrath AW, Nizet V, Johnson RS (2014) HIF transcription factors, inflammation, and immunity. Immunity 41:518–528
Li J, Yuan J (2008) Caspases in apoptosis and beyond. Oncogene 27:6194–6206
Yilmaz S, Ates E, Polat C, Koken T, Tokyol C, Akbulut G, Gokce O (2003) Ischemic preconditioning decreases laparoscopy induced oxidative stress in small intestine. Hepatogastroenterology 50:979–982
Cevrioglu AS, Yilmaz S, Koken T, Tokyol C, Yilmazer M, Fenkci IV (2004) Comparison of the effects of low intraabdominal pressure and ischaemic preconditioning on the generation of oxidative stress markers and inflammatory cytokines during laparoscopy in rats. Hum Reprod 19:2144–2151
Yilmaz S, Polat C, Kahraman A, Koken T, Arikan Y, Dilek ON, Gokce O (2004) The comparison of the oxidative stress effects of different gases and intra-abdominal pressures in an experimental rat model. J Laparoendosc Adv Surg Tech A 14:165–168
Ates E, Yilmaz S, Ihtiyar E, Yasar B, Karahuseyinoglu E (2006) Preconditioning-like amelioration of erythropoietin against laparoscopy- induced oxidative injury. Surg Endosc 20:815–819
Cay A, Imamoglu M, Unsal MA, Aydin S, Alver A, Akyol A, Sarihan H (2006) Does anti-oxidant prophylaxis with melatonin prevent adverse outcomes related to increased oxidative stress caused by laparoscopy in experimental rat model? J Surg Res 135:2–8
Bergström M, Swain P, Park PO (2007) Measurements of intraperitoneal pressure and the development of a feedback control valve for regulating pressure during flexible transgastric surgery (NOTES). Gastrointest Endosc 66:174–178
Ko CW, Shin EJ, Buscaglia JM, Clarke JO, Magno P, Giday SA, Chung SS, Cotton PB, Gostout CJ, Hawes RH, Pasricha PJ, Kalloo AN, Kantsevoy SV (2007) Preliminary pneumoperitoneum facilitates transgastric access into the peritoneal cavity for natural orifice transluminal endoscopic surgery: a pilot study in a live porcine model. Endoscopy 39:849–853
Acknowledgments
The authors wish to thank Dr Theodora—Eleftheria Deftereou for her assistance in the histopathogical and immunohistochemical co-evaluation of tissue specimens.
Disclosures
Petros Ypsilantis, Maria Lambropoulou, Ioannis Tentes, Maria Chryssidou, Themistoklis Georgantas and Constantinos Simopoulos have no conflict of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ypsilantis, P., Lambropoulou, M., Tentes, I. et al. Room air versus carbon dioxide pneumoperitoneum: effects on oxidative state, apoptosis and histology of splanchnic organs. Surg Endosc 30, 1388–1395 (2016). https://doi.org/10.1007/s00464-015-4341-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4341-4