Abstract
Breath-hold divers train and compete in maximal apnea performance. Glossopharyngeal inhalation (GI) is commonly used to increase lung volume above vital capacity (VC) prior to apnea. We investigated the hypothesis that this practice would increase apnea performance and relaxed airway pressure. Seven well-trained breath-hold divers performed maximal bouts of apnea at three different lung volumes (85% VC, VC and VC + GI) both at rest (dry static apnea) and during underwater swimming (dynamic apnea). Heart rate, apnea time and end tidal PCO2 and PO2 (P ET CO2 and P ET O2) were recorded. In addition, relaxed airway pressure was measured after GI. Maximal GI increased lung volume by 1.59±0.57 l above VC and increased relaxed airway pressure to from 3.5±0.5 to 8.7±1.7 kPa. Dry static apnea time was higher at VC + GI (346±46 s) than at VC (309±38 s, P<0.05) and 85% VC (297±48 s, P<0.01). Likewise, dynamic apnea time was higher at VC + GI (97±27 s) than at VC (78±14 s, P<0.05) and 85% VC (71±17 s, P<0.05). P ET O2 values reached 3.5±0.6 kPa at the end of dry static apnea bouts and this was not different from dynamic apnea when taking hydrostatic pressure at swimming depth into account (3.7±0.6 kPa, P=0.48). In conclusion, GI increases lung volume, relaxed airway pressure and apnea performance in well-trained breath-hold divers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breath-hold divers train for and compete in static apnea (maximal breath holding at rest) and dynamic apnea (maximal underwater swimming distance). Performance in both these events is limited by the factors that determine when a maximal apnea bout ends (breaking point). Among these, arterial CO2 and O2 tensions (P aCO2 and P aO2, respectively) are considered to be the most potent regulators of ventilatory drive at rest (Ferretti et al. 1991). A reduction in P aO2 and a rise in P aCO2 during apnea is inevitable, but this will proceed more slowly at larger lung volumes. Therefore, it seems logical that breath-holding performance should be positively related to lung volume as suggested by Lin (1982). It is also common practice among breath-hold divers to engage in glossopharyngeal inhalation (GI) prior to a bout of apnea in order to increase their lung volume above what can be obtained with conventional breathing (Lindholm and Nyren 2005). However, it has so far not been documented that increasing the inspired volume above vital capacity (VC) is beneficial for breath-holding performance, and it could be speculated that the extra muscular work and time required for GI prior to apnea would obliterate the advantages of the increased amount of air in the lungs. In addition to this, Andersson and Schagatay (1998) observed that in well-trained divers and underwater rugby players, breath-hold performance was similar when inspiring 85 or 100% of VC prior to a bout of apnea.
Therefore, this study was undertaken with the primary purpose of investigating the effects of three inspired lung volumes (85% VC, VC and VC + GI) on performance in dry static and dynamic apnea in well-trained breath-hold divers.
Second, the relaxed airway pressure was measured during GI to establish the relation between these parameters. In addition, the heart rate responses during dry static and dynamic apnea were recorded in order to evaluate the possible effects of GI-induced increases in relaxed airway pressure on the bradycardic response during apnea. Finally, end tidal PO2 (P ET O2) and PCO2 (P ET CO2 ) were measured after dry static and dynamic apneas to establish the relative importance of these ventilatory stimuli in breath-hold performance at different lung volumes.
Methods
Subjects
Seven young well-trained male breath-hold divers volunteered for the study. The subjects were 30±2 years of age, measured 1.82±0.06 m and weighed 80±11 kg. The subjects had at least 2 years of apnea training experience and during the investigation period all subjects trained for dynamic and static apnea two times per week in a 25-m pool. In addition, several of the subjects performed apnea training at home on a daily basis and one subject trained for depth diving as well as apnea. The study conformed to the principles of the Declaration of Helsinki and was approved by the ethical committee of Aarhus County.
Protocol
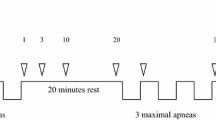
Subjects were tested on three separate occasions in the lab and on three separate occasions at the swimming stadium. The first lab visit included measurements of VC, GI volume and relaxed airway pressure during GI. During the second visit to the lab, the residual volume (RV) of the subjects was measured and during the third visit, dry static apnea performance at three different lung volumes, heart rate and end tidal O2 and CO2 fractions were measured. During each of the visits to the swimming stadium one maximal dynamic apnea bout was performed with one of the three predetermined lung volumes. The sequence of the three lung volumes used in both dynamic and dry static apnea was varied between the subjects in a counterbalanced fashion. As a safety precaution a medical doctor was present during all experimentation involving maximal apneas or maximal GI.
VC, GI volume and relaxed airway pressure
The subjects were lying in supine position and breathed through a mask connected to a spirometer (Brand, Germany). VC was measured during inspiration and expiration. After a maximal conventional inhalation, the subjects performed the GI technique, which consists of repeatedly sucking in mouthfuls of air and pressing them down into the lungs with a “swallowing” movement. The mask was fitted with a one-way valve allowing only inspiration and a small metal tube which protruded into the mouth was connected to a differential pressure transducer. A predetermined number of GI manoeuvres were performed and the volume was recorded. The subjects then relaxed their inspiratory muscles and opened their glottis while leaving the lips closed briefly to allow measurements of the pressure of the buccal cavity, which can be considered as representative of the relaxed airway pressure under these circumstances. This procedure was repeated with an increasing number of GI manoeuvres until the subjects reached their maximal GI ability. In this way, 6–7 corresponding data points for inhaled volume and buccal cavity pressure were obtained for each subject in the range from VC to VC + maximal GI.
Measurement of RV
RV was measured using a modified version of the oxygen dilution technique (Wilmore 1969): subjects expired to RV and were connected to a closed spirometer system containing a CO2 absorber. The closed system was initially filled with 100% oxygen. Following a 5-min equilibration period of re-breathing into the system, the subject again expired to RV and was disconnected from the closed system. The volume of the system was recorded from the spirometer and the oxygen fraction (FO2 ) of the system was measured with a respiratory gas analyser (Datex, Helsinki, Finland). Since only O2 and N2 were present in the system the N2 fraction (FN2 ) could be calculated as FN2=1 − FO2. Assuming that the fraction of nitrogen in the lungs was 0.79 when the subjects were connected to the system the RV was calculated by the equation:
where V sys is the volume of the closed system after the disconnection of the subject and FN2 is the fraction of N2 in the system at this time.
The subjects rested for 10–15 min and the measurement was repeated. If the calculated RV varied by more than 10% from the first trial a third trial was conducted. Since the method is sensitive to possible leakage of N2 into the system during connection and disconnection of the subject, which would overestimate RV, the lowest recorded RV value for each subject was chosen as the correct value.
Dry static apnea
Subjects were lying in supine position during the measurements. This procedure is slightly different from the competitive situation of static apnea, where apnea bouts are performed while floating in a pool with the face immersed. In order to distinguish between these situations, we have termed the presently used conditions “dry static apnea.” Two warm up maximal apneas were performed in order to utilize the short-term training effect (Sterba and Lundgren 1985). After this, the subjects performed three maximal apnea bouts at three different lung volumes in: 85% VC, VC and VC + GI. Each of the apnea bouts were preceded by at least 5 min of rest followed by 2 min of hyperventilation. The subjects then expired to RV and inspired to the previously determined volume. In order to mimic the competitive situation the subjects were allowed to use GI to a degree which was comfortable for the subject. The volume inspired with GI was recorded using a spirometer. End tidal CO2 and O2 concentrations were measured during the last expiration before all bouts of apnea and during the first expiration after the apnea bouts using a gas analyser (AMIS 2001, Innovision, Odense, Denmark), which was calibrated to gas mixtures made from commercial high-grade gases of known concentrations (AGA, Denmark). The apnea time and the time used for inspiring to the determined lung volume with or without GI were recorded with a stop-watch and heart rate was recorded with beat-to-beat resolution before and during the apnea bouts using a heart rate monitor (Polar S810i, Polar Electro OY, Kempele, Finland).
Dynamic apnea
The measurements were performed in a local municipal swimming facility in a 25-m long pool (water temperature 26°C, depth 2 m) after a light warm up including one or two submaximal dynamic apneas. The dynamic apnea bouts were performed without fins. Prior to the maximal apnea bout, the subjects, who were in the water at the pool edge, hyperventilated for 2 min. The subjects then expired to RV and inspired to the previously determined volume. End tidal CO2 and O2 concentrations were measured during the last expiration before all bouts of apnea and during the first expiration after the apnea bouts using a gas analyser (AMIS 2001). Only one maximal dynamic apnea bout was performed per subject on a given day. The subjects returned on two other occasions to complete all three dynamic apnea bouts. During the dynamic apnea bouts subjects dove to the bottom of the pool and remained at that water depth throughout the dive (about 1.8 m). The gas analyser was rolled on a cart next to the pool so that the subject could expire into the mouthpiece immediately upon emerging from their dive. The length of the dive was recorded to the nearest meter and heart rate, apnea and inspiration times were recorded as described in dry static apnea. Due to loss of signal from the heart rate monitor, heart rate data was only obtained in 16 of a total of 21 dynamic apnea bouts.
Data presentation and statistics
All lung volumes are expressed at BTPS conditions. Data are reported as means ± SD. To test for differences between conditions Student’s paired t-test was used. The level used for significance was P<0.05.
Results
Lung volumes
RV was measured to 2.53±0.45 l, VC was 7.20±1.00 l that yielded a total lung capacity (TLC) of 9.73±1.36 l. These values were all significantly higher (P<0.01) than the normal values estimated using population-derived equations based on the age, height and gender of our subjects (Quanjer et al. 1993). When using GI the subjects were able to inspire further 1.59±0.57 l of air yielding a TLC + GI volume of 11.33±1.61 l.
Relaxed airway pressure
As shown in Fig. 1 there was a progressive increase in the relaxed airway pressure with increasing lung volume inhaled. One of the seven subjects was not able to relax and keep his lips closed while at the same time opening the glottis. Therefore, the data presented on relaxed airway pressure are from six subjects only. At VC the average relaxed airway pressure was 3.5±0.5 kPa and this was increased to 8.7±1.7 kPa at the maximal level of GI.
Relationship between GI volume and relaxed airway pressure. Corresponding data points for GI volume and relaxed airway pressure measured in the buccal cavity during opening of the glottis were determined at several different levels of GI up to maximal GI in six subjects. GI was performed after inspiration to VC (GI volume=0)
Dry static apnea
As shown in Table 1, the recorded inspired lung volume was as expected significantly different between the three bouts of apnea with 85% VC being the lowest and VC + GI being the highest. The dry static apnea time was significantly longer with VC + GI than with VC and 85% VC. P ET O2 immediately before the apnea bout was slightly higher at VC + GI than at VC, but not significantly different from 85% VC. After apnea, no significant differences were observed in P ET O2 between lung volumes. P ET CO2 was at the same level before apnea at all three lung volumes. After the apnea bouts, P ET CO2 was significantly lower at 85% VC than at VC and VC + GI.
When plotting lung volume against apnea time for all apnea bouts in all subjects a significant linear correlation (r=0.57, P<0.01) was observed as shown in Fig. 2. This indicated that the amount of air in the lungs played a significant role in determining apnea time.
Relationship between lung volume and apnea duration of dry static apnea bouts. Individual corresponding data points for lung volume and apnea duration from seven subjects were plotted for dry static apnea bouts with 85% VC (triangles), VC (open circles) and VC + GI (filled circles). A linear regression line was constructed to fit the data points
The heart rate measured at the beginning of apnea was 74±14 bpm at, 79±12 bpm and 84±15 bpm at 85% VC, VC and VC + GI, respectively. The initial heart rate was significantly lower at 85% VC than at VC and VC + GI (P<0.05). At all lung volumes, heart rate decreased significantly from the beginning to the end of apnea (to 59±16, 56±15 and 51±11 bpm at 85% VC, VC and VC + GI, respectively).
Dynamic apnea
The duration of the dynamic apnea bouts was 82±22 s as an average of all three lung volumes, whereas dry static apnea bouts lasted considerably longer (319±47 s; P<0.001). The data recorded during the dynamic apnea bouts are presented in Table 2. As shown, the recorded inspiration volume was highest in the VC + GI bout and lowest in the 85% VC bout corresponding to the instructions given to the subjects. Diving distance was significantly longer in the VC + GI bout, than in the 85% VC bout, but no significant differences were found between VC and either VC + GI or 85% VC.
Before apnea, the P ET O2 was significantly lower and P ET CO2 was significantly higher in the dynamic apnea bouts than in dry static apnea at all lung volumes (P<0.001), indicating that the hyperventilation performed prior to dynamic apnea was less pronounced than the hyperventilation performed prior to dry static apnea. As in the dry static apnea bouts, no significant differences were found in P ET O2 after dynamic apnea on comparison of the three bouts. However, when pooling the data from all three dry static bouts and all three dynamic bouts of apnea a significantly lower P ET O2 was observed in the dynamic than in the dry static apnea (3.1±0.5 kPa versus 3.5±0.6 kPa, P<0.01), whereas P ET CO2 was significantly higher after dynamic than dry static apnea (7.3±0.8 kPa vs 6.5±0.7 kPa, P<0.001).
It should be remembered though, that dynamic apnea takes place at the bottom of a pool– in this case at about 1.8-m depth. Consequently, due to the increased hydrostatic pressure, P aO2 and P aCO2 will be at a higher level at the bottom than at the surface. Thus, the mean P ET O2 measured at the surface after dynamic apnea was actually an underestimation of the P aO2 that the subjects were exposed to at 1.8-m depth when they chose to rise to the surface. We calculated the corresponding P aO2 at 1.8-m depth to 3.7±0.6 kPa and this value was not significantly different from the P ET O2 measured after dry static apnea (3.5±0.6 kPa, P=0.48). A similar calculation was done for P ET CO2, and as shown in Fig. 3, there was a marked and significant difference (P<0.001) between the P ET CO2 after dry static apnea and after dynamic apnea. Also, from Fig. 3 it is evident that the P ET O2 and P ET CO2 values reached at the end of both dry static and dynamic apnea by these trained breath-hold divers is different from values of alveolar partial pressures for O2 and CO2 observed in untrained individuals at breaking point (Otis et al. 1948).
P ET CO2 and P ET O2 before apnea and after dry static and dynamic apnea. Average values for P ET CO2 and P ET O2 were obtained before apnea (grey symbols) and at breaking point (white symbols) in either dry static apnea bouts (circles) or dynamic apnea (squares). The black square indicates P ET CO2 and P ET O2 at breaking point after dynamic apnea corrected for hydrostatic pressure at diving depth (1.8 m). The curve represents breaking point values of P ET CO2 and P ET O2 for normal subjects redrawn from Otis et al. (1948). Symbols show means of seven subjects with error bars indicating ± SD
The heart rate recordings from the dynamic apnea bouts revealed no significant differences at the different lung volumes. When all dynamic apnea bouts were pooled together a decrease in heart rate from the beginning to the end of dynamic apnea from 97±20 to 69±29 bpm was found (P<0.01). The average heart rate of the dynamic apnea bouts was found to be significantly higher than that of the dry static apnea bouts (82±21 bpm vs 69±11 bpm, P<0.01).
Discussion
The main new findings of the present study were that trained breath-hold divers can increase their lung capacity considerably by GI and that this increases apnea time significantly under competition-like conditions. We also showed that increasing volumes of GI was associated with a progressive increase in relaxed airway pressure and finally we demonstrated that in well-trained breath-hold divers, apnea can be maintained until P ET O2 and P ET CO2 reaches levels beyond what has been found in untrained individuals.
Increased performance after GI
GI has been previously reported to be practiced among breath-hold divers (Lindholm and Nyren 2005). And a few reports have measured that on average between 1.5 and 3.5 l of air can be inspired by this technique in trained breath-hold divers (Örnhagen et al. 1998; Muth et al. 2003; Lindholm and Nyren 2005). This is in line with the present findings of an average GI volume of 1.6 l (range 1.0–2.8 l). No previous studies have determined the effect of GI on breath-holding performance. It could be argued that the time used for GI and the muscle work involved would add to the oxygen consumption during breath-holding. If this consumed amount of oxygen is similar to that taken into the lungs by GI, then no effect of GI on apnea time would be expected. However, we demonstrated here that dry static apnea time at VC + GI was increased by an average of 37 s compared with VC and by 49 s compared with 85% VC. Similarly, for the dynamic apnea the distance covered was 15 m longer at VC + GI than at 85% VC, and although the difference of 8 m between VC + GI and VC was not significant (P=0.15), there was a significantly increased diving time of 19 s at VC + GI compared with VC.
We found no significant differences in apnea time or distance covered between VC and 85% VC. This confirms earlier findings by Andersson and Schagatay (1998) who also did not observe a significant difference in dry static apnea performance at these two lung volumes in trained divers and underwater rugby players. On the other hand, the significant positive correlation between lung volume and apnea duration shown in Fig. 2, suggests that also a lowering of lung volume below VC should decrease apnea time.
During the maximal apnea bouts the subjects did not perform maximal GI, because this was perceived as uncomfortable by the subjects. The instructions given were to take in as much extra air by GI as they would do in a competitive situation. The GI volume was on average 0.6±0.4 l in the dry static apnea bouts, which was significantly lower than the 1.1±0.5 l measured in the dynamic apnea bouts (P<0.05). The time required to perform the GI manoeuvres was only about 5 s in both cases. The explanation for the larger GI volume tolerated in dynamic apnea is that when the divers perform the diving bout, they are exposed to increased hydrostatic pressure, which will reduce the lung volume and thereby minimize the discomfort of a high GI volume. This was confirmed by the subjects who reported that GI-induced discomfort was reduced upon diving.
GI and relaxed airway pressure
We showed not surprisingly that the GI manoeuvres caused a considerable progressive increase in relaxed airway pressure. A similar finding has previously only been published in a preliminary report concerning two subjects (Örnhagen et al. 1998).
The average relaxed airway pressure of 3.5 kPa at VC in our subjects was considerably higher than the average value of 2.7 kPa for normal subjects (Rahn et al. 1946). From the data of Rahn et al., the overall lung compliance from FRC (i.e. at a relaxed airway pressure equal to ambient pressure) to VC for normal subjects can be estimated to 1.1 l/kPa (their FRC corresponded to 35% of VC and mean VC was 4.84 l). Using the same procedure (i.e. FRC=35% of VC) on the present data the estimated overall lung compliance from FRC to VC for the six subjects turned out to be 1.4 l/kPa. The higher overall lung compliance of the breath-hold divers will of course reduce their inspiratory effort per litre of air inspired compared with their normal counterparts and it will of course also be beneficial to the divers when they practice GI.
The explanation for this difference in overall lung compliance may be quite simple. The breath-hold divers will operate at a much higher absolute lung volume at any possible percentage of TLC than normal subjects. What this really means is that for any given change in volume around a certain percentage of TLC the change in the linear dimension of the lungs will be less in the trained breath-hold divers compared with the normal subjects. In other words, the corresponding change in lung tension should also be less in the breath-hold divers solely due to their much higher TLC, all other things being equal.
Heart rate responses to apnea
Our measurements of heart rate responses during apnea confirmed the findings of earlier studies of a bradycardic response to apnea (Bergman Jr et al. 1972; Lin 1982; Andersson and Schagatay 1998). This response was not influenced significantly by lung volume or GI, since bradycardia developed to the same extent at all lung volumes. The heart rate was increased during dynamic apnea as compared with dry static apnea, but a significant bradycardic response was still observed during dynamic apnea, which is in line with earlier findings (Bergman Jr et al. 1972). There was a tendency for an increased heart rate with increasing lung volume at the beginning of dry static apnea. This may reflect a response to a decreased venous return at VC and VC + GI as compared with 85% VC because of an increased relaxed airway pressure at higher lung volumes and possibly because of stimulation of stretch receptors in the lung. A similar tendency was observed in a study by Andersson and Schagatay (1998). We did not observe any differences in heart rate at the end of dry static apnea between the three lung volumes. This may be because of the fact that the substantial amount of O2 taken up from the lungs during apnea is not replaced by an equal amount of CO2. The net loss of gas from the lungs during dry static apnea at VC + GI was about 1 l, which would reduce lung volume to below VC. Intrathoracical pressure and lung stretch receptor stimulation would therefore predictably decrease and thereby reduce any tachycardic response from these mechanisms towards the end of apnea.
Determinants of breaking point
Our results suggest a clear positive role of increased lung volume for apnea performance. In light of this, it is also interesting to note that this group of breath-hold divers had significantly larger VC, RV and TLC than the calculated normal values. In accordance with this, it has been reported previously in some studies that trained breath-hold divers have above normal VC and TLC (Schaefer et al. 1968; Lindholm and Nyren 2005). However, others have found values that were comparable with a normal population (Ferretti et al. 1991). Nevertheless, it may be speculated that the above normal lung volumes of our subjects could be partly an adaptation to breath-hold diving. In support of this a study of navy diving instructors showed that a period of apnea training increased VC from 5.2 to 5.6 l (Carey et al. 1956).
Whatever the reason for the large lung volumes, it is clear that this factor and the ability to perform GI provided our subjects with an extra amount of oxygen, which can be used during a bout of apnea. However, this is only one amongst the many possible factors that determine the duration of a bout of apnea. Other important factors include the ability to maintain a low oxygen consumption during apnea (during dynamic apnea a low oxygen cost of swimming) and the ability to tolerate a low P aO2 and a high P aCO2 . When we assume that P ET O2 corresponds to P aO2 and we take into account the effect of hydrostatic pressure at the diving depth, we find that the apneas are terminated when the P aO2 is close to 3.6 kPa in both dry static and dynamic apnea, with no apparent effects of lung volume. However, PET CO2 varies considerably more between dry static (6.1–6.7 kPa) and dynamic apnea (7.1–7.5 or 8.4–8.8 kPa when correcting for hydrostatic pressure). This indicates that the breaking point of trained breath-hold divers is determined by P aO2 rather than P aCO2 . This observation is at variance with several other reports that find evidence for a relation between the breaking point and a P ET CO2 of around 6.9 kPa (Hong et al. 1971; Sterba and Lundgren 1985; Andersson and Schagatay 1998). An important difference between the aforementioned studies and the present study is that we allowed subjects to hyperventilate prior to the apnea bouts. This hyperventilation induced a decrease in P ET CO2 and presumably P aCO2 to 3.7 kPa prior to dry static apnea and to 4.9 kPa prior to dynamic apnea. Particularly in the dry static apnea this hyperventilation will have delayed the build up of P aCO2 considerably, and therefore a critical level of P aO2 was reached before the P aCO2 was high enough to induce breaking point.
The maximal apnea experiments were performed in a way that closely resembled competitive and training procedures of the subjects. Preparation for the apneas included warm up bouts, hyperventilation and GI, which are all allowed in breath-hold competitions. These conditions allowed for breath-hold times above 300 s and swimming distances above 50 m in all subjects in dry static and dynamic apnea, respectively. Therefore, our results can be considered to be representative for the physiological responses that breath-hold divers experience during competition. In the 21 maximal dry static apnea bouts we observed three occasions of brief involuntary spasms occurring immediately after breaking point (this was not observed during dynamic apneas). This reaction is probably due to a reduction of P aO2 in parts of the CNS to critically low levels and these apneas did include the two lowest values for P ET O2 observed in dry static apnea. Since such adverse reactions would entail a disqualification in competition according to the rules of the international breath-hold diving association our subjects strive to avoid this. Nevertheless, all our subjects had previously experienced such spasms showing that they were able to hold their breath to a point, very close to loss of consciousness. This highlights the need for taking adequate safety measures during breath-hold training and competition to avoid accidents. In relation to this it has been reported that apnea after hyperventilation (Craig Jr 1976) and more recently also apnea after prolonged exercise (Lindholm and Gennser 2005) may increase the risk of apnea-induced syncope due to the attainment of low P aO2.
Conclusion
We conclude that the breath-hold performance of trained breath-hold divers is increased with increasing lung volumes up to VC and can be further increased by applying GI to increase lung volumes above VC. Employing GI leads to a build up of relaxed airway pressure which is related to the GI volume. However, the overall lung compliance of the breath-hold divers seems to be increased compared with the normal subjects. In addition to the importance of lung volume for breath-holding performance it can be concluded that trained breath-hold divers are able to tolerate apnea and ignore respiratory drive until their P ET O2 reaches values around 3.6 kPa, which in a clinical setting would be considered critically low and require immediate intervention.
References
Andersson J, Schagatay E (1998) Effects of lung volume and involuntary breathing movements on the human diving response. Eur J Appl Physiol Occup Physiol 77:19–24
Bergman SA Jr, Campbell JK, Wildenthal K (1972) Diving reflex in man: its relation to isometric and dynamic exercise. J Appl Physiol 33:27–31
Carey CR, Schaefer KE, Alvis HJ (1956) Effect of skin diving on lung volumes. J Appl Physiol 8:519–523
Craig AB Jr (1976) Summary of 58 cases of loss of consciousness during underwater swimming and diving. Med Sci Sports 8:171–175
Ferretti G, Costa M, Ferrigno M, Grassi B, Marconi C, Lundgren CE, Cerretelli P (1991) Alveolar gas composition and exchange during deep breath-hold diving and dry breath holds in elite divers. J Appl Physiol 70:794–802
Hong SK, Lin YC, Lally DA, Yim BJ, Kominami N, Hong PW, Moore TO (1971) Alveolar gas exchanges and cardiovascular functions during breath holding with air. J Appl Physiol 30:540–547
Lin YC (1982) Breath-hold diving in terrestrial mammals. Exerc Sport Sci Rev 10:270–307
Lindholm P, Gennser M (2005) Aggravated hypoxia during breath-holds after prolonged exercise. Eur J Appl Physiol 93:701–707
Lindholm P, Nyren S (2005) Studies on inspiratory and expiratory glossopharyngeal breathing in breath-hold divers employing magnetic resonance imaging and spirometry. Eur J Appl Physiol 94:646–651
Muth CM, Radermacher P, Pittner A, Steinacker J, Schabana R, Hamich S, Paulat K, Calzia E (2003) Arterial blood gases during diving in elite apnea divers. Int J Sports Med 24:104–107
Örnhagen H, Schagatay E, Andersson J, Bergsten E, Gustafsson P, Sandström S (1998) Mechanisms of buccal pumping (lung packing) and its pulmonary effects. Manuscripts for the XXIV annual scientific meeting of the European Underwater and Baromedical Society 1998
Otis AB, Rahn H, Fenn WO (1948) Alveolar gas changes during breath holding. Am J Physiol 152:674–686
Quanjer PH, Tammeling GJ, Cotes JE, Pedersen OF, Peslin R, Yernault JC (1993) Lung volumes and forced ventilatory flows. Report Working Party Standardization of Lung Function Tests, European Community for Steel and Coal. Official Statement of the European Respiratory Society. Eur Respir J Suppl 16:5–40
Rahn H, Otis AB, Chadwick LE, Fenn WO (1946) The pressure–volume diagram of the thorax and lung. Am J Physiol 146:161–178
Schaefer KE, Allison RD, Dougherty JH Jr, Carey CR, Walker R, Yost F, Parker D (1968) Pulmonary and circulatory adjustments determining limits of depths in breathhold diving. Science 162:1020–1023
Sterba JA, Lundgren CE (1985) Diving bradycardia and breath-holding time in man. Undersea Biomed Res 12:139–150
Wilmore JH (1969) A simplified method for determination of residual lung volumes. J Appl Physiol 27:96–100
Acknowledgments
We thank M.D. Henrik Staunstrup for acting as a clinically responsible supervisor for the project and for being present during all the experiments requiring clinical surveillance. We thank the divers of Aarhus free-diving club for their participation in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Overgaard, K., Friis, S., Pedersen, R.B. et al. Influence of lung volume, glossopharyngeal inhalation and P ET O2 and P ET CO2 on apnea performance in trained breath-hold divers. Eur J Appl Physiol 97, 158–164 (2006). https://doi.org/10.1007/s00421-006-0156-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-006-0156-2