Abstract
Competitive breath-hold divers use glossopharyngeal breathing in order to increase their performance. Glossopharyngeal inhalation (GI) increases the volume of air in the lungs above the total lung capacity, thereby increasing the volume of gas available for pressure equalization at great depth. The reverse procedure, glossopharyngeal exhalation (GE), is used to suck air out of the lungs at great depth when the lungs are compressed, thus providing air in the mouth for equalization of pressure in the middle ear. Five Swedish apnea athletes were tested. Their vital capacity (VC) and the volume of air exhaled after GI were measured with a turbine spirometer, while the residual volume (RV), and the volume of gas in the lungs following GE was determined using a helium dilution procedure. Thereafter subjects performed these maneuvers during magnetic resonance imaging (MRI) of the thorax. All subjects exhibited a higher VC + GI (7.8–11.9l) than VC (6.2–9.5l) and lower RV–GE (1.16–1.77l) than RV (1.37–2.40l). MRI revealed pronounced changes in the volume of intrathoracic blood, with a small heart and compressed vessels following GI and the opposite, i.e., enlarged vessels during GE. MRI also showed an invagination of the posterior wall of the trachea, in connection with GE in certain subjects.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Breath-hold diving has become increasingly popular as a competitive sport in recent years. In this sport, often referred to as “apnea”, the athletes compete by diving as deep into the ocean as they can, or by holding their breath as long as possible. To perform deep dives, it is, of course, advantageous to have a large volume of air in the lungs. To fill their lungs with extra air, some divers perform glossopharyngeal breathing (GPB) prior to diving. Furthermore, certain divers use a reverse form of GPB, in which air is drawn out of the lungs for equalization of pressure in the inner ear and sinuses.
Glossopharyngeal breathing is a technique which allows the lungs to be ventilated without the use of the respiratory muscles. Such breathing was initially described by Dail (Dail 1951), who observed its use by post-poliomyelitic patients with weakened respiratory muscles and very low vital capacities (VC). These patients used the muscles of the mouth and pharynx to swallow air into the lungs, thereby inhaling a larger breath and increasing their VC from 100 ml to 600 ml to a VC + GPB of 600 ml to 1710 ml (Dail 1951; Dail et al. 1955). This technique can also be employed by patients with tetraplegia as a result of spinal cord injuries in order to survive for shorter periods (as long as a day) without the aid of a ventilator (Bianchi et al. 2004).
It is also possible to reverse this procedure and thus exhale air. We have chosen to refer to these two maneuvers as glossopharyngeal inhalation (GI) and glossopharyngeal exhalation (GE). For purposes of training, such breathing can be performed starting at FRC (functional residual capacity), but the investigation described here concerns the use of GI as a complement to a full inhalation to total lung capacity (TLC), a procedure referred to as TLC + GI for the sake of clarity. In addition, we have examined the technique of using GE following full exhalation to residual volume (RV), defined here as RV − GE. The techniques of GI and GE have been known and practiced for some time among elite breath-hold divers, but except for a few case studies (Andersson et al. 1998; Muth et al. 2003; Simpson et al. 2003), little research has been carried out in this area. To our knowledge, no previous report on the technique of RV − GE has been published.
Our hypothesis was that these maneuvers result in extraordinarily high and low volumes, respectively, of air in the lungs and bronchi and that this would also influence the thoracic blood volume. An additional hypothesis was that during RV − GE, when the lungs are almost completely emptied of air, the trachea would also be affected.
Material and methods
Subjects
Five male volunteers (age 20–35 years, height 179–187 cm, and weight 68–84 kg) were selected from elite Swedish apnea athletes on the basis of their ability to perform GI and GE. All subjects were nonsmokers. After observing a demonstration of the experimental procedures to be applied, each subject gave his informed consent. Our experimental protocol was approved by the Ethics Committee of Karolinska Institutet and performed in accordance with the Helsinki declaration.
Protocol
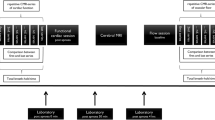
All measurements were performed in the supine position. Subjects were first monitored by spirometry and approximately one hour later repeated the same maneuvers for magnetic resonance imaging (MRI). For each subject three measurements of VC were first performed and thereafter two determinations of glossopharyngeal inhalation (VC + GI). Subsequently, the normal residual volume was measured twice, followed by two determinations of glossopharyngeal exhalation (RV-GE). The subjects exhaled maximally and then inhaled and rebreathed the mixture of helium and oxygen. The spirometric volumes are presented in body temperature pressure saturated (BTPS).
Magnetic resonance imaging was performed using a standard clinical scanner (1.5 Tesla, Philips Intera magnetic resonance scanner, Philips, the Netherlands) located in the Department of Radiology at Karoliska Hospital. The subjects lay down on the camera couch and were fitted with a dedicated SENSE body coil. Following initial prescans and localizing scan, the thorax of each subject was imaged during breath-holds lasting approximately 30 s under conditions of FRC, TLC + GI and RV − GE.
All five subjects were also examined utilizing a specific scan of the trachea under conditions of FRC and RV − GE. The trachea was imaged during TLC + GI in 3 subjects only (Table 2); while on the other two subjects, A and D, coronal series were performed during TLC + GI and RV − GE (Fig. 2). Axial and coronal series with a slice thickness of 10 mm and a 2 mm gap were performed. A gradient echo sequence with repetition times of 131, an echo of 4.6 and a flip angle of 80° was employed. These parameters varied slightly between scans and subjects. Pulse or ECG gating was not utilized.
The tracheal volume was calculated by first manually drawing a line around the edges of lumen in each slice (MR Dimview 2.5, Nycomed Amersham Imaging). The area of each luminal trace was then multiplied by 12 mm (the slice thickness of 10 mm + the 2 mm gap), and the volumes, thus calculated for the individual slices from the glottis to the tracheal bifurcation, were added together to obtain the total volume of the trachea.
Measurements
A standard helium dilution procedure (5% He; 95% O2) was employed to obtain measurements of RV and RV − GE has been described previously (Lindholm and Linnarsson 2002). Briefly, the system utilized rebreathing of preset volumes of gas from a bag and analysis of gases using a mass spectrometer (QMG 420, Balzer, Lichtenstein) modified for respiratory measurements (Innovision AS, Odense, Denmark). This gas analyzer was calibrated against mixtures of known concentrations (AGA-Linde Gas AB, Lidingö, Sweden).
Vital capacity and glossopharyngeal inhalation (VC+GI) were determined with an infrared interruption flow sensor (SpirobankG, http://www.spirometry.com, MIR, Italy).
Statistics
Paired t-test for dependent samples was used to correlate the studied parameters. Significance was accepted at the 5% level (Sigma Plot 8.0).
Results
Spirometry
As illustrated schematically in Fig. 1, and documented in detail in Table 1, GI enabled subjects to fill their lungs with a volume of air 25% greater than their total lung capacity; whereas GE reduced the amount of air in the lungs to 21% less than the residual volume. It is noteworthy that these subjects all have lungs which are larger than normal (P<0.05 TLC vs predicted TLC, n=5). When some subjects filled their lungs completely using TLC + GI, they developed the “barrel chest” appearance typical of a patient with emphysema. Subject C, with a predicted vital capacity of 5.5 l, based on clinical reference values, released almost 12 l of gas in one exhalation, indicating that the volume of air in his lungs was 100% greater than normal. Predicted values of TLC, VC and RV are from the ATS workshop on lung volume measurements (Stocks and Quanjer 1995).
Magnetic resonance imaging
MRI scan of the thorax during GI maneuvers revealed that the thoracic blood volume was markedly reduced with emptying of the vessels and heart, and that even the thoracic portions of the aorta were affected. During TLC+GI the diaphragm also shifted downward. On the other hand, during RV − GE the vessels of the lungs were engorged, and the heart dilated, as shown in Fig. 2.
The diameter of the trachea and volume of air present in this structure was also affected by these maneuvers (Table 2). During GE, the subjects suck air out of their lungs, thereby reducing both the diameter and area of the trachea and decreasing the volume of tracheal air by an average of 50%. A horse-shoe shaped piece of cartilage creates stability in the ventral and lateral walls of the trachea but the posterior wall consists of soft tissue only. The tracheal area and volume were reduced all the way from the glottis down to the tracheal bifurcation (Table 2). Some subjects exhibited a clear invagination of the posterior wall, thereby reducing the internal area of the trachea even further. The greatest such invagination was observed in subject D at a level just above the top of the sternum (Fig 3c).
Axial MRI of a cross-section of the trachea a at functional residual capacity (FRC) and b following residual volume with glosspharyngeal exhalation (RV − GE). c An invagination of the posterior wall of the trachea at a level immediately above the top of the sternum is clearly shown in this enlargement of the image of the trachea shown in b
Discussion
In the present investigation we have examined healthy human subjects who use glossopharyngeal breathing in order to empty or fill their thorax with an extraordinary volume of air, a volume greater than that which is achieved by regular inspiratory and expiratory efforts.
The use of GI in breath-hold diving
The duration of a breath-hold is limited in part by the oxygen stores present at the beginning of apnea and by the oxygen consumption. By performing GI, divers are able to fill their lungs with extra air and thus increase the amount of oxygen available (Muth et al. 2003). Furthermore, when diving deep, the air is compressed according to Boyle’s law and the diver must be able to equalize the pressure in the inner ear and sinuses with the available air. GI provides an increased volume of air for such equalization. It has been used by spear fishing divers in the Mediterranean Sea for many years (örnhagen et al. 1998). This technique was also used by Robert Croft when he set the world record in 1968 by breath-hold diving to 73 m (personal communication with Croft 2002).
The use of GE in breath-hold diving
When the thorax is completely compressed in connection with diving to great depth, it is impossible to push air from the lungs into the mouth using the respiratory muscles. With GE a diver can suck air into his mouth and then close the glottis and utilize this air to equalize the pressure in the middle ear, allowing him to dive deeper. Furthermore, GE is employed as a training method to simulate the thoracic compression at great depth. In this connection GE is used to empty the lungs of as much air as possible prior to diving to a depth of 4–5 m in a swimming pool, thereby producing a compression of the thorax and lungs that is otherwise available only at great depth.
Patients with dysfunctional respiratory muscles also utilize GBP to increase the volume of air in their lungs, but in this case the volume achieved is still well below the individual’s predicted TLC, when in full health (Dail et al. 1955). A healthy subject can also perform these maneuvers within the range of their VC. The most interesting feature of the present study was that our subjects employed these maneuvers starting at a full VC or after a complete exhalation to residual volume, thereby achieving volumes both greater and smaller than those previously measured by spirometry.
A possible explanation of where the extra volume of air was located during TLC + GI is provided by the MRI, which reveals a pronounced shift in thoracic blood volume, so that very little blood remains in this region of the body following this maneuver. The MR images suggested that both the venous return and thoracic blood volume were reduced and indeed, the heart was very small (Fig. 2a). It has been reported that performance of maximal GPB by patients increases the intrathoracic pressure (oesophageal pressure) and that this causes the arterial blood pressure to drop; in fact, in one subject the pulse pressure was completely eliminated for a period of 15 s (Collier et al. 1956). This explains why divers practicing TLC + GI sometimes experience syncope, especially while standing or sitting on land (personal observation). In a case study on one elite breath-hold diver, TLC + GI was shown to increase intrapleural and mouth pressure as determined by relaxation of the open airway against a pressure gauge, whereas there was no difference in the transpulmonary pressure during TLC and TLC + GI (Simpson et al. 2003). Relaxed airway pressure (mouth pressure) during VC + GI was increased by 53–103% in comparison to a normal VC in a study on three subjects (örnhagen et al. 1998).
We were unable to obtain exact quantitations of the thoracic blood volume in this study but MRI indicated that the thoracic blood volume increased in connection with RV − GE. The mean difference between RV and RV − GE was 0.4 dm3 of air, a volume which we suggest was balanced to a large extent by a shift of blood from the rest of the body into the thorax, since the reduction in tracheal volume was only 0.017 dm3 . During breath-hold diving from the surface to a great depth, a shift of blood into the thorax has been demonstrated and estimated to be around 1 l of blood (Schaefer et al. 1968).
Cases of hemoptysis caused by alveolar hemorrhage during breath-hold diving, reflected as blood in the lungs as revealed by a CT-scan, have been described (Boussuges et al. 1999; Kiyan et al. 2001). The underlying mechanism (Kiyan et al. 2001) is suggested to involve a capillary stress failure (West 2000) as a consequence of the intrathoracic pressure drop, with rupture of pulmonary capillaries occurring due to the large difference between alveolar and pulmonary capillary pressures. Moreover, many divers report small bleedings “spitting blood”, after deep diving and some even maintain that their tolerance to deep diving without such bleeding has increased with training, allowing them to dive ever deeper without bleeding (personal communication and experience with competitive breath-hold divers). Many of these bleedings were not of the magnitude reported by Boussuges et al. (1999).
Our findings indicate that the strain on tracheal tissue is severe during compression, leading us to the alternative suggestion that at least some of the bleeding associated with deep breath-hold diving is due to the rupture of tracheal vessels as well. Breath-hold divers of both sexes have achieved depths below 160 m, surfacing in full health. One speculation as to how divers might be able to reach such extraordinary depths without undue pulmonary damage is that a gradual increase in the flexibility of the trachea occurs, enabling greater and greater pulmonary compression without rupture of blood vessels.
The maneuvers characterized in this paper have not been described in detail and we suggest that these should be learned and performed with caution. GI may cause orthostatic syncope as a consequence of reduced venous return. Apnea for too long a period following GE may lead to syncope from hypoxemia, due to the reduction in pulmonary oxygen stores. Furthermore, the medical risks associated with these maneuvers are not yet known in detail.
References
Andersson J, Schagatay E, Gustafsson P, Örnhagen H (1998) Cardiovascular effects of “buccal pumping” in breath-hold divers. In: 29th annual scientific meeting of the European underwater and baromedical society on diving and hyperbaric medicine
Bianchi C, Grandi M, Felisari G (2004) Efficacy of glossopharyngeal breathing for a ventilator-dependent, high-level tetraplegic patient after cervical cord tumor resection and tracheotomy. Am J Phys Med Rehabil 83(3):216–219
Boussuges A., Pinet C, Thomas P, Bergmann E, Sainty JM, Vervloet D (1999) Haemoptysis after breath-hold diving. Eur Respir J 13(3):697–699
Collier CR, Dail CW, Affeldt JE (1956) Mechanics of glossopharyngeal breathing. J Appl Physiol 8(6):580–584
Dail CW (1951) Glossopharyngeal breathing by paralyzed patients: preliminary report. Calif Med 75:217–218
Dail CW, Affeldt JE, Collier CR (1955) Clinical aspects of glossopharyngeal breathing; report of use by one hundred postpoliomyelitic patients. J Am Med Assoc 158(6):445–459
Kiyan E, Aktas S, Toklu AS (2001) Hemoptysis provoked by voluntary diaphragmatic contractions in breath-hold divers. Chest 120(6):2098–2100
Lindholm P, Linnarsson D (2002) Pulmonary gas exchange during apnoea in exercising men. Eur J Appl Physiol 86(6):487–491
Muth CM, Radermacher P, Pittner A, Steinacker J, Schabana R, Hamich S, Paulat K, Calzia E (2003) Arterial blood gases during diving in elite apnea divers. Int J Sports Med 24(2):104–107
Örnhagen H., Schagatay E, Andersson J, Bergsten E, Gustafsson P, Sandström S (1998) Mechanisms of “buccal pumping” (“lung packing”) and its pulmonary effects. 29th annual scientific meeting of the European underwater and baromedical society on diving and hyperbaric medicine
Schaefer KE, Allison RD, Dougherty JH Jr, Carey CR, Walker R, Yost F, Parker D (1968) Pulmonary and circulatory adjustments determining the limits of depths in breathhold diving. Science 162(857):1020–1023
Simpson G, Ferns J, Murat S (2003) Pulmonary effects of “lung packing” by buccal pumping in an elite breath-hold diver. SPUMS J 2003(33):122–126
Stocks J, Quanjer PH (1995) Reference values for residual volume, functional residual capacity and total lung capacity. In: ATS workshop on lung volume measurements. Official statement of the European respiratory society. Eur Respir J 8(3):492–506
West JB (2000) Invited review: pulmonary capillary stress failure. J Appl Physiol 89(6):2483–2489;discussion 2497
Acknowledgments
This study was supported by the Swedish National Centre for Research in Sports. The assistance of Roberto Vargas, RT (MR, R), is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lindholm, P., Nyrén, S. Studies on inspiratory and expiratory glossopharyngeal breathing in breath-hold divers employing magnetic resonance imaging and spirometry. Eur J Appl Physiol 94, 646–651 (2005). https://doi.org/10.1007/s00421-005-1358-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-005-1358-8