Abstract
Although blood is the reference medium in the field of forensic toxicology, alternative matrices are required in case of limited, unavailable or unusable blood samples. The present review investigated the suitability of bone marrow (BM) as an alternative matrix to characterize xenobiotic consumption and its influence on the occurrence of death. Basic data on BM physiology are reported in order to highlight the specificities of this matrix and their analytical and toxicokinetic consequences. A review of case reports, animal and human studies involving BM sample analysis focuses on the various parameters of interpretation of toxicological results: analytic limits, sampling location, pharmacokinetics, blood/BM concentration correlation, stability and postmortem redistribution. Tables summarizing the analytical conditions and quantification of 45 compounds from BM samples provide a useful tool for toxicologists. A specific section devoted to ethanol shows that, despite successful quantification, interpretation is highly dependent on postmortem interval. In conclusion, BM is an interesting alternative matrix, and further experimental data and validated assays are required to confirm its great potential relevance in forensic toxicology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although blood is the reference medium in the field of postmortem analytical toxicology, the use of other biological matrices has for decades been described in cases of limited, unavailable or unusable blood samples. Bone marrow (BM) is one such alternative matrix. According to a number of reports [1–3], BM may act as a repository for drugs, by virtue of its rich vascularization, a high lipid content and a bone protection against contamination, that make it potentially suitable for forensic toxicology. BM may therefore be a relevant alternative tissue, especially when remains are skeletonized, bloodless or in extreme putrefaction. BM is already used in forensic science for genetic analysis [4], to estimate postmortem interval [5–8], in the diatom test for diagnosis of drowning [9, 10] and in histopathology to establish certain malignancies postmortem [11–13]. In forensic toxicology, the first report of BM analysis was in 1943, to document the kinetics of alcohol [14]. In the 1980s, Winek et al. [3, 15–24] intensively studied the correlation between blood and BM in both animal and human models. During the following decade, few toxicological data on BM were published, except for some case reports. Recently, there has been renewed interest in BM, in particular with the work on skeletal remains by the Laurentian University (Ontario, Canada) [25–30].
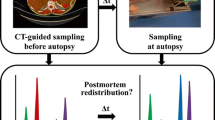
The main aim of postmortem toxicology analysis is to determine possible consumption of xenobiotics by the victim and its relevance to the occurrence of death. Achieving this objective when only BM is available raises two kinds of question: (1) Can xenobiotics be detected in BM from a pharmacokinetic and analytical point of view? (2) Are drugs levels in BM samples representative of blood concentrations at time of death, i.e., are BM results quantitatively interpretable? The purpose of the present review was to determine whether the international literature provides any answers to these questions, and more generally to present a survey of the published data on BM analysis in forensic toxicology. A systematic PubMed review was performed, using the search term ‘marrow’ combined with ‘toxicology’, ‘forensic’, ‘post mortem’, ‘postmortem’ and ‘chromatography’ and cross-checked with the references in each article retrieved. Basic data on BM physiology are reviewed, to explain the specificities of this matrix and their implications for analytical and toxicokinetic aspects. The various parameters of interpretation (analytical limits, sample collection, pharmacokinetics, stability and postmortem distribution) are then examined.
Physiology
Composition
As of birth, hematopoiesis is essentially confined to BM. One of the largest organs in the body, BM constitutes approximately 4% of total body weight (3,000 and 2,600 g in adult males and females, respectively). It is encased in the medullary cavities of bone, with 15% in trabecular bone [31]. Histologically, BM is a highly organized and complex vascular connective tissue (Fig. 1). Its cellular components include adipocytes, hematopoietic cells (from stem to mature cells) and reticuloendothelial cells, supported by a trabecular framework. On gross examination, BM is red (hematopoietic marrow, Fig. 1a) or yellow (fatty marrow, Fig. 1b) depending on its predominant components. In a middle-aged adult, red marrow comprises 60% hematopoietic cells; chemically, it consists of 40–60% lipids, 30–40% water and 10–20% protein. Yellow marrow is almost entirely composed of adipocytes (95%); chemically, it consists of 80% lipids, 15% water and 5% protein [32]. The proportion of adipocytes and hematopoietic cells can vary diffusely or focally (isolated island), resulting in a normal heterogeneity [31, 33].
Hematoxylin–eosin-stained histologic sections of bone marrow (original magnification ×25). a Normocellular BM with a cellularly around 40% (Ad adipocyte, Hem hematopoietic cells). b Fatty BM in an old subject. c Transversal section of a nutrient arteriole (Ar arteriole, Tb trabecular bone). d Sinusoïd with intra-sinusoïdal red blood and hematopoietic cells (Si sinusoid)
Vascularization
BM has a dual blood supply, consisting of a periosteal capillary network and nutrient arteries that penetrate the bone and branch within the medullary tissue (Fig. 1c) [31, 34, 35]. In red marrow, an abundantly ramified network of sinusoids is formed (Fig. 1d). The sinusoids, with discontinuous endothelial cells and a disrupted basal lamina, are highly permeable to protein and mature blood cells. On the other hand, the vascular network of yellow marrow is much less abundant, and is constituted of capillaries [33]. Estimated BM blood flow is approximately 10 ml/min/100 cm3 in healthy adults [31] and is reduced in older subjects [36].
Age-related involution
The proportion of fatty and cellular components of BM changes with age in a physiological conversion of red to yellow marrow. The transition occurs over the first two decades of life, in a predictable monotonous sequence. During fetal growth, hematopoiesis takes place in all skeletal compartments as in liver and spleen. At birth, splenic and hepatic hematopoiesis has already ceased, and red marrow is present throughout the entire skeleton. After birth, marrow conversion starts in the terminal phalanges and extends in a symmetric centripetal manner in the peripheral skeleton. Additionally, in long bones, marrow conversion occurs in diaphyses and progresses both distally and proximally toward metaphyses (Fig. 2). The adult pattern of marrow distribution is generally achieved by the age of 25 years, when red marrow is localized in the axial skeleton (skull, spine, sternum, clavicles, scapulas, pelvis, ribs) and proximal femora and humeri. From then on, the proportion of fatty cells increases in the remainder of the skeleton, at a speed depending on individual parameters and medical conditions [31, 32, 37]. Studies showed an increase in fat fraction of around 7% per decade [38]. Hematopoietic marrow decreases to around 30% of total BM at 80 years of age [37]. Several mechanisms of red-to-yellow conversion have been studied. Some assume that it is related to thermal conditions [39] or to the proportion of mesenchymal stem cells within the marrow cavities [40]. According to Bigelow and Tavassoli [41], it follows a programmed design defined by the location of adipose and hematopoietic precursor at birth.
Diagrammatic representation of the distribution of red marrow (in black) in tubular bones from birth until 25 years. At birth, unossified epiphyses do not contain red marrow. From Blebea et al. [31], with permission
Pathological BM conversion
Various benign or malignant disorders and therapeutic events can alter BM composition. In normal adults, yellow marrow may be reconverted into red marrow to increase blood cell production, in case of hemolytic anemia or certain malignant processes, for example. Reconversion proceeds in exactly the reverse sequence to the initial conversion, and occurs quickly in flat bones since these retain hematopoietic marrow throughout life [32, 37]. Benign BM hyperplasia has been observed under various physiopathological processes of chronic tissue hypoxia, including obesity, long-distance running or heavy smoking, and in chronic disorders resulting in anemia, such as hemoglobinopathy or chronic infection [31–33]. It is characterized by an increase in red marrow within the distal metaphyseal region of long bones. Although not fully established [37, 38], a few studies reported that benign hyperplasia was more frequent in females than males [31, 33, 38, 42], likely due to menstruation and female hormonal specificities. BM fat content increases to compensate for hypocellularity (aplastic anemia, inhibition of hematopoiesis by certain tumors, etc.) or trabecular thinning (osteopenia) [43–45]. In contrast, cancer cell infiltration results in replacement of fatty marrow by cancer cells, increasing the cellular content of BM, with a focal, multifocal or diffuse distribution [43–45]. Angiogenesis, which facilitates malignancy perfusion, has been described in BM [46–48]. In certain specific malignancies, BM necrosis can occur, resulting in loss of myeloid tissue and marrow fat without trabecular destruction [43]. Finally, medical treatment can also modify BM contents: e.g., hematopoietic factor increases red marrow contents while anticancer radiation therapy and chemotherapy increase the proportion of yellow marrow [43, 45].
Postmortem changes of BM
BM is encased either in the medullary cavity of long bones or in the trabecular tissue of cancellous bones [28]. This shield of solid bony tissue provides great mechanical stability. Therefore, as long as bone integrity is preserved, BM can be assumed to be better protected than any other organ sample against maggot infestation and postmortem contamination and damage (trauma, animal predators or fungus, bacteria and parasites) [2, 3, 49]. Once the bone is broken, however, the BM is no longer protected and may even be non-recoverable [26, 50]. Specific local protection seems to delay putrefaction [3]. Roll et al. [11] investigated the histopathology of 225 BM samples from autopsies performed between 12 and 140 h postmortem: they found few autolytic changes in BM specimens, compared to major alterations in other organ samples from the same corpse. A retrospective report of 20 years’ experience of exhumation [51] estimated BM histologic preservation to be at least 3 months.
As described above, normal human BM is roughly red or yellow, with a firm gelatinous consistency [2, 3, 21]. With increasing postmortem interval and depending on conservation conditions, BM samples can become dark and lose integrity [3, 21], resulting in a brown oily liquid. They can also become adipocerous by saponification [52, 53] or dry into brownish or yellowish powder [54–56]. Overall, BM has been found suitable for toxicological analysis in human corpses up to 5 years after death [57].
BM analysis
Due to the complexity of BM composition, in particular its high lipid content, as well as variability in sample quality, BM analysis remains complex. Tables 1 and 2 report sampling location, sample pre-treatment methods, analytic assays and findings from publications concerning targeted analysis and screening on BM samples, respectively.
Sample collection and storage
No standardized procedures of BM collection and storage have been proposed. BM can be sampled postmortem from different locations: in the femur after section of the cortical bone [19], squeezed out of the ribs using pliers [49], or by trocar aspiration in vertebral bodies as in vivo [58]. The resulting samples present different properties: femoral BM is fattier than rib BM, while aspirates are in liquid form rich in hematopoietic cells. Few works considered stability during storage. As described later, Winek et al. studied in vitro stability of some drugs at varying temperature [15, 18, 24] as well as the influence of the nature of container (glass or polyethylene) and the use of preservative on ethanol conservation [20]. These investigations showed that BM samples should be analyzed as soon as possible due to concentration variation during storage. Overall, as for classical samples used in toxicology and without specific data on drug stability, storage at low temperature should be privileged. Preservatives, such as sodium fluoride, should be added for certain drugs (e.g., ethanol) even if homogenization in BM lipid may be difficult [20].
Sample preparation
Distinctive features were reported regarding sample preparation, related to the connective and highly lipid contents of BM. One-step preparations were reported only for particular applications involving immunologic assay [1] or headspace injection [58]. Two steps were usually added to conventional pre-treatment protocols: BM dissolution and a lipid removal step. Dissolution is needed to obtain a homogenous liquid suitable for further extraction. Various methods were described involving mechanical techniques (ultrasonication or homogenizer) or agitation, heating, and maceration in extraction medium. Lipid removal can be achieved by an additional hexane wash of the final extract [3, 22, 24, 59, 60] or by multi-step extraction as proposed by Guillot et al. for the quantification of morphine and 6-acetylmorphine (6-AM) [54]. A solid-phase extraction process was successfully applied to BM analysis in other studies [29, 30, 49, 56, 61].
Analytical methods
Several analytical techniques have been described as suitable and relevant for BM analysis. In most cases, forensic analysis of BM uses chromatographic approaches similar to those for other matrices. Chromatographic separation is principally performed by gas chromatography (GC) rather than liquid chromatography (LC). This can be easily explained by the fact that mass spectrometry (MS) is the detection system of choice for toxicological analysis of such complex matrices, and GC/MS systems were in more widespread use than LC/MS systems until a few years ago; recently, however, liquid chromatography tandem mass spectrometry has also been applied to BM [29, 30, 49]. While mass spectrometry remains the main detection system, as reported in Table 1, other detection systems have been used, such as flame ionization detection for volatile molecules (e.g., ethanol, methanol, isopropanol). Various publications highlighted the suitability of immunological assay for qualitative [25–27, 29, 30, 62] and quantitative purposes [1, 50, 63, 64].
Case reports
In at least six case reports [55, 57, 65–68], toxicological findings were restricted to skeletal tissue analysis. They concerned corpses discovered in skeleton state, 7 months to 5 years after their disappearance. The remains consisted of bones, sometimes with putrefied adhering tissue, and containing BM in various stages of decomposition. During investigation, toxicological analysis was required to shed light on the circumstances of death or the state of consciousness of the victim at time of death. As only BM was available for analysis, the authors attempted to detect, quantify and interpret the presence of xenobiotics in this matrix. Findings and case contexts are summarized in Table 3.
Acetaminophen and dextropropoxyphen were detected by Bal et al. [65] on skeletal remains found in a forest. The body was attributed to a man who disappeared 20 months previously, leaving a suicide note in his car. He had been prescribed Distalgesic (dextropropoxyphene and paracetamol) and Tranxene (chlorazepate potassium). The authors drew no conclusions regarding possible intoxication, due to lack of data for drug levels in unusual matrices.
In another case, the body of a 47-year-old woman was discovered, virtually skeletonized in a deserted area of her family ranch. By BM identification, Noguchi et al. [66] suggested that amitriptyline was present in antemortem circulation. However, several uncertainties concerning the fate of compounds in BM matrix (e.g., stability, drug distribution) made any quantitative interpretation unreliable. The police conducted a systematic search in the pharmacies of the region and found a prescription for amitriptyline for the presumed decedent.
In a third case, triazolam was detected in two BM samples and in one decomposed muscular fragment from two victims found buried, pointing to antemortem administration [67]. These analytical data were in agreement with statements by the suspects, who confessed they had administered triazolam to sedate the victims before burying them alive. BM triazolam concentrations were similar in both victims (0.36 and 0.37 ng/g), suggesting that both had received similar triazolam doses before death.
Maeda et al. [55] were able to detect bromisovalum in BM after the discovery of a skeleton on a bushy hill slope. Near the remains, three empty medication vials of bromovalerylurea (which would represent a maximum 30 g of bromisovalum) were discovered. Concentrations of 36.4 and 139.7 μg/g were measured in BM from the right and the left femur, respectively. When compared to the lethal concentrations reported in blood (44–114 μg/ml), the higher BM concentration suggested a possible contribution to the fatality. The authors stressed that drug accumulation in BM lipids, previously described by Winek et al. [3, 22], could not be excluded in this case. Moreover, the discrepancy in BM concentration between right and left femurs suggested postmortem redistribution and/or degradation.
Higuchi et al. [68] reported a very similar case of bromisovalum impregnation in BM (95.4 μg/g), suggesting an overdose in the light of the circumstances of death and the bromisovalum level found in the BM samples compared with previous reports in other matrixes.
Finally, Kojima et al. [57] quantified amphetamine and methamphetamine in the BM of a methamphetamine abuser killed by strangulation and whose corpse lay buried for 5 years. Referring to a published schedule of effects according to amphetamine plus methamphetamine blood level, the authors suggested that the victim was, at the moment of his death, in an intermediate state of intoxication with mental disorder, if not a more severe state, given that some studies showed that amphetamine levels are usually lower in fatty tissue than in blood.
Taken together, these case reports highlight the relevance of analyzing BM tissue as an alternative matrix for xenobiotic detection, up to 5 years after death. Nevertheless, the lack of data about BM pharmacokinetics and postmortem changes limits interpretation of BM findings.
Interpretation
Qualitative approach
At least 45 compounds of forensic interest, including psychoactive and illicit drugs, volatiles, pesticides and herbicides, have been detected either by selective analysis (Table 1) or by targeted and general screening (Table 2). Using the General Unknown Screening approach, Bévalot et al. [60] detected 18 compounds in BM out of 32 identified in human blood. According to the authors, this low detection rate in BM was directly related to the restricted performance of the analytical method, especially in terms of detection limit and non-optimized procedures for certain drug families. McIntyre et al. [2], in two studies comparing drugs detected in blood and in the corresponding BM, found respectively 45% and 70% concordance; the discrepancy between the two studies may have been due to differences in sampling location (femur vs. rib BM) or time of storage (more than 3 years in the first study). After standardized drug administration to rats, Watterson and colleagues reported the sensitivity of enzyme-linked immunosorbent assays (ELISAs) on BM samples for fentanyl, ketamine and diazepam; this sensitivity varied from 66% to 100% depending on the analyte, dose administered, and interval between administration and death [25–27, 29, 30].
Correlation between BM and blood concentrations
Several studies investigated correlations between BM and blood drug concentrations that might enable extrapolation. Such correlations are more or less significant depending on the xenobiotic, as reported in Table 4. Winek et al. demonstrated that extrapolation of blood level from BM level was possible in a rabbit model, for desipramine [24], flurazepam [22], isopropanol [18], methanol [23], nortriptyline [3] and pentobarbital [16].
Discrepancies in pharmacokinetic processes between blood and BM are observed for some compounds. Winek et al. [15] demonstrated that, in rabbits, peak ethchlorvynol blood level occurs 10–30 min after intraperitoneal injection and peak BM level between 15 and 60 min. In rats, diazepam clearance appears to be slower in BM than in blood, resulting in higher and longer BM impregnation [64]. This phenomenon was also reported in rats by Watterson et al. for diazepam [29] and fentanyl [26]: they assumed that accumulation occurred in BM and then in bone, followed by slow redistribution from bone to blood via BM. Benzodiazepine accumulation was also established in human autopsy specimens, where levels in BM were nearly 2.5 times as high as in blood (8.5 times for diazepam specifically) [2].
Where BM/blood correlations prove non-significant, various reasons have been suggested: death occurring before the steady-state was reached as described for heroin overdose by Guillot et al. [54], difference in sampling location, age and BM lipid/water ratio, storage conditions, and postmortem changes as proposed by Winek et al. [15, 18]. The last of these factors is fully described below.
Postmortem changes and stability of xenobiotics in BM
After death, various processes occur in corpses, including postmortem redistribution, degradation or evaporation and neo-formation. These phenomena can affect xenobiotic concentrations compared to at-death levels. Moreover, the toxicologist has to solve analytical problems directly related to the putrefied matrix and the compounds’ fate during sample storage. Several experimental models have been developed to estimate the impact of postmortem alteration in corpore on xenobiotic levels in BM. Studies have also been conducted to assess in vitro stability in BM samples.
After chronic administration of midazolam for 10 days, mice were sacrificed [62]. Bodies were stored for 21 days under three different conditions: frozen, or buried in sterilized or unsterilized soil (three mice per condition). Midazolam from serum, BM and viscera was quantified by ELISA. Levels were similar in BM samples stored frozen and in sterilized soil but were undetectable in unsterilized soil storage. The authors did not exclude that response based on immunological assay may be decreased due to analytical interference associated with putrefaction.
To study the stability of amphetamine compounds, i.v. methamphetamine was administered to five rabbits [69]. After sacrifice, bone samples were collected and stored for 2 years at room temperature, either in a dry environment or in water. Quantification was undertaken at 3, 6, 12 and 24 months postmortem. Methamphetamine was shown to be stable in samples from the dry environment, while large variability in concentrations was observed in samples stored in water.
Several studies estimated the postmortem behavior of certain herbicides and pesticides in BM. Ito et al. [56] studied the fate of paraquat orally administered to rabbits (n = 3). Animals were buried and samples from various tissues were analyzed regularly over a 2-year period. Paraquat was detectable in BM samples over the entire period, with relatively stable levels throughout the first year. However, these conclusions are to be taken with caution due to the limited population size and the great heterogeneity of results. In another study, 12 rabbits received lethal per os doses of diazinon or endosulfan [61]. Each animal acted as its own control: BM from the right tibia and femur were analyzed immediately, then remains were buried for a 1-month period. At exhumation, diazinon concentrations were around 25-fold higher than in samples at the moment of death (mean = 1,783 vs. 71 mg/kg). Undetected in controls, alpha and beta endosulfan isomers were found 1 month later. Conversely, the sulfate metabolite of endosulfan was detected at death but not 1 month later. The authors impute these phenomena to postmortem biotransformation or redistribution by diffusion and/or vascular transport.
Two studies of opioids showed concordant findings. First, morphine was injected into nine rabbits; BM samples were collected at death, and after 1 and 2 weeks’ burial [1]. A decrease in morphine concentration of 21% and 38% was observed during respectively the first and second week of inhumation. The authors suggested that this may have been due to back-diffusion from BM to putrefied tissue and soil. During the second week, the process was probably enhanced by increased putrefaction. In the same toxicological field, lethal injections of heroin were administered to 12 mice. Levels of morphine and 6-AM were compared between BM collected immediately after death and frozen until analysis and BM stored for 2 months at room temperature in buried bone. The experiment showed a 71% decrease in 6-AM, while morphine became undetectable [54]. Other metabolites could not be tested, due to lack of BM samples.
Several short-term studies monitored the BM xenobiotic levels in rabbits stored at room temperature for less than 48 h after sacrifice. Such experiments tended to prove the stability of isopropanol [18], methanol [23] and nortriptyline [3] over a 24-h period. Conversely, the concentration of acetone decreased, probably due to its volatility. Pentobarbital underwent a slight increase between 6 and 12 h postmortem, inducing an increase in the BM/blood ratio and a decrease in the correlation between blood and BM levels [16].
Finally, some studies assessed in vitro stability in BM by reanalyzing samples over time after storage under various conditions. Isopropanol was shown to be stable up to 24 h at both room temperature and +4°C [18]. Other compound samples were also studied: ethchlorvynol (from 0 to 24 h, frozen) [15], acetone (from 0 to 24 h, at +3.5°C or at room temperature) [18], methanol (from 24 h to 21 days, frozen) [23] and desipramine (from 7 to 22 days, frozen) [24]. For each substance, significant reductions (or, in some cases, increases) in BM concentration were reported. The authors suggested that these variations may be related to various processes such as evaporation, degradation, compound release from protein binding sites, or fat distribution heterogeneity in the samples.
Analysis of ethanol in BM
Ethanol has a special place in forensic toxicology due to the high morbidity and mortality associated with its toxicity and widespread consumption. Numerous studies have focused on its quantification in BM in both animal models and human samples (Table 5). In 1943, the first quantification of ethanol from BM samples was performed in five fresh corpses [70]. Several decades later, again from fresh corpses, correlation was established between blood and BM levels in an animal model [21] and human samples [17, 19]. Greater blood/BM ratio variability was found in rabbits than in humans. According to the authors, this variability could be related to biological differences, postmortem redistribution or varying lipid levels in BM samples from rabbit femurs and human ribs [19]. To avoid the last of these biases, Winek et al. [17] recommended, for the first time, correcting BM concentration taking into account the water content of the sample. This aqueous portion was calculated as the weight difference between BM sample and lipid content; the latter was evaluated by weighting the residue after evaporation of BM ether extract [17]. This correction factor enhanced the correlation and improved estimation of blood level from BM assay. Recently, Maeda et al. [58] also observed an excellent correlation between the levels in blood and BM aspirate collected between 5 and 48 h after death. Aspiration of BM in liquid form from vertebrae, however, is not available in most cases involving elderly victims, death from blood loss or multiple trauma. Overall, BM seems to be a useful alternative matrix for the interpretation of ethanol level when corresponding blood samples are not available in fresh corpses.
Samples from human BM collected up to 9 days after death matched blood results only in terms of presence vs. absence [71]: this lack of correlation led the authors to conclude that BM assay allows detection of ethanol but not assessment of impregnation. In the same study, six femoral samples (three ethanol-positive and three negative BMs) were stored at room temperature for 1 year. Contradictory findings were obtained, and it was impossible to determine whether alcohol had been present at time of death. Supporting data were reported by Winek et al. [21] on a control group (n = 30) and ethanol-treated group (n = 60) of rabbits, stored after sacrifice at room temperature for 1 month. Up to 78.3 mg% neo-formation of ethanol was observed at 7 days in the control group; in the ethanol-treated rabbits, ethanol levels decreased gradually with time to a mean loss of 89.3% after a 28-day period of storage. Thus, the estimation of ethanol blood levels at death from BM data is uncertain (46.7% error at 28 days). Similarly, an in vitro study, performed on BM samples stored over 3 months at −6°C under various conditions, reported large variations in ethanol level: either decreases due to collection tube porosity or enzymatic oxidation during the time of analysis at room temperature, or increases caused by yeast and bacterial synthesis [20]. Ethanol neo-formation may lead to false positives in BM as in blood, either in vitro or in corpore.
Ethyl glucuronide is a minor direct metabolite of ethanol, produced by enzymatic conjugation with glucuronic acid. Since its neo-formation has never as yet been demonstrated postmortem, this compound may constitute a relevant marker of ethanol consumption [49, 72]. Schloegl et al. [49] demonstrated that ethyl glucuronide can be detected in BM, suggesting that BM may be a helpful matrix when classical materials are not available. However, ethyl glucuronide’s stability in BM has yet to be established. Some studies suggested that ethyl glucuronide concentrations in blood and urine decline during putrefaction, long term storage at room temperature or in case of bacterial urinary infection [72–74], while others described a post collection formation of ethyl glucuronide in urine under experimental condition using bacteria [75, 76]. Ethyl sulfate is another non-oxidative metabolite of ethanol. This compound seems to be a promising marker due to its stability [75, 77], even if its bacterial degradation has also been described during standardized degradation test [78]. The simultaneous determination of these both metabolites, in urine and blood, seems to be more relevant than quantification of ethyl glucuronide alone and should help to verify or disprove a postmortem formation of ethanol [76, 79]. However, ethyl sulfate has not yet been investigated in BM.
In conclusion, various processes, including postmortem redistribution, enzymatic degradation, volatility and bacterial neo-formation, hinder interpretation of BM ethanol results.
Discussion and conclusion
In forensic toxicology, although blood is the reference sample for qualitative and quantitative interpretation, various tissues may be available for analysis according to the circumstances of death. In the case of skeletonized remains, severe putrefaction or extreme multiple trauma, BM may be the only alternative tissue for toxicological investigation. It presents several advantages, such as protection against contamination and putrefaction due to its location within bones, rich vascularization and large amount of lipid constituents. The present review gives an overview of case reports and animal and human studies involving BM analysis. This survey investigated the suitability of BM analysis for characterizing xenobiotic consumption and its influence on the occurrence of death, answering two main questions.
The first question was: can xenobiotics be detected in BM from a pharmacokinetic and analytical standpoint? Since BM is highly vascularized by a large sinusoid network, each compound circulating in the blood is assumed to be present in BM. Therefore BM detection of xenobiotics depends essentially on the performance of the analytical method. Nevertheless, the latter can be limited by the sample pre-treatment required for such a complex and fatty matrix. As few full validations have been made of assay sensitivity, negative results must be interpreted with caution. Furthermore, stability is a significant parameter in postmortem toxicology and is even more essential in BM analysis since this matrix comes into its own as an alternative to blood in case of long postmortem interval or aggressive phenomena (bloodless cadaver, fragment of corpse, etc.). In vitro and in corpore stability in BM has been occasionally studied, with varying results depending on drug class and time and condition of conservation, providing some clues for the interpretation of negative BM results.
To the second question—Are the drug levels in BM samples representative of the blood levels at time of death? —the literature does not provide any general answer. Although pharmacokinetic data for BM are limited, specific processes were occasionally described, such as BM accumulation of benzodiazepines and fentanyl. The mechanisms involved in BM drug distribution should therefore be investigated in animal experiments. Correlation between blood and BM concentrations was demonstrated for a wide range of compounds, allowing extrapolation from BM to blood results, which are more easily interpretable. However, the application of these data, mostly obtained on animal models with standardized protocols, to human autopsy cases, subject to uncontrollable and often unknown postmortem conditions, requires further study. When correlation with blood is not established, a statistical approach could be interesting to determine either a toxicity threshold or the likelihood that a drug level, quantified in an alternative matrix, corresponds to overdose rather than therapeutic use [59, 80]. Another aspect to consider for quantitative interpretation is the postmortem changes of BM concentration. Beyond drug stability, postmortem redistribution of diazinon and endosulfan was shown to involve increase as well as decline in BM levels. Finally, as a result of varying BM composition (i.e. fatty and cellular proportion) in different bones according to age, sampling location was claimed by Winek et al. [15] and McIntyre et al. [2] to be a relevant factor that should be investigated. Likewise, hydrophilic or lipophilic behavior of molecules should be considered: Winek et al showed that blood/BM correlation of water soluble compound, such as methanol [23], ethanol [17], isopropanol and acetone [18], was improved correcting their concentration for water content, whereas other authors described accumulation in BM of lipophilic drugs like diazepam [2, 29, 64].
In conclusion, we consider that BM matrix is of great potential interest in forensic toxicology. Further experimental data and validated analytical assays are required to enable reliable qualitative determination and, eventually, quantitative interpretation from human BM samples.
References
Cengiz S, Ulukan O, Ates I, Tugcu H (2006) Determination of morphine in postmortem rabbit bone marrow and comparison with blood morphine concentrations. Forensic Sci Int 156:91–94
McIntyre LM, King CV, Boratto M, Drummer OH (2000) Post-mortem drug analyses in bone and bone marrow. Ther Drug Monit 22:79–83
Winek CL, Morris EM, Wahba WW (1993) The use of bone marrow in the study of postmortem redistribution of nortriptyline. J Anal Toxicol 17:93–98
Frank WE, Llewellyn BE (1999) A time course study on STR profiles derived from human bone, muscle, and bone marrow. J Forensic Sci 44:778–782
Dmitrienko Iu A, Kononenko VI, Lakiza BS (1983) Postmortem changes in bone marrow tissue as a criterion of time of death. Sud Med Ekspert 26:19–21
Findlay AB (1976) Bone marrow changes in the post mortem interval. J Forensic Sci Soc 16:213–218
Hao LG, Deng SX, Zhao XC (2007) Recent advancement in relationship between DNA degradation and postmortem interval. Fa Yi Xue Za Zhi 23:145–147
Luo GH, Chen YC, Cheng JD, Wang JF, Gao CL (2006) Relationship between DNA degradation and postmortem interval of corrupt corpse. Fa Yi Xue Za Zhi 22:7–9
Gruspier KL, Pollanen MS (2000) Limbs found in water: investigation using anthropological analysis and the diatom test. Forensic Sci Int 112:1–9
Pollanen MS (1997) The diagnostic value of the diatom test for drowning: II. J Forensic Sci 42:286–290
Roll P, Beham A, Beham-Schmid C (2009) Post-mortem histopathological investigations of the bone marrow in forensic medicine: an important issue for both the forensic and clinical pathologist. Forensic Sci Int 186:e17–e20
Sakai K, Takatsu A, Shigeta A, Abe S, Ikegami M, Takagi K (2007) Sudden death due to undiagnosed acute promyelocytic leukemia: a case report. Int J Leg Med 121:311–314
Umezawa A, Yamada T, Ogawa Y, Kuramochi S, Watanabe Y (1990) Postmortem diagnosis of acute megakaryocytic leukemia. Usefulness of immunohistochemistry and tissue hemogram. Acta Pathol Jpn 40:693–698
Casier H, Thomas F, Delaunois AL (1943) La répartition de l'alcool chez l'homme et les animaux au cours de l'intoxication éthylique. Arch Int Pharmacodyn 69:186–204
Winek CL, Cibulas W Jr, Wahba WW (1981) A comparative study of ethchlorvynol levels in blood versus bone marrow. Forensic Sci Int 17:197–202
Winek CL, Costantino AG, Wahba WW, Collom WD (1985) Blood versus bone marrow pentobarbital concentrations. Forensic Sci Int 27:15–24
Winek CL, Esposito FM (1981) Comparative study of ethanol levels in blood versus bone marrow, vitreous humor, bile and urine. Forensic Sci Int 17:27–36
Winek CL, Janssen JK (1982) Blood versus bone marrow isopropanol concentrations in rabbits. Forensic Sci Int 20:11–20
Winek CL, Jones T (1980) Blood versus bone marrow ethanol concentrations in rabbits and humans. Forensic Sci Int 16:101–109
Winek CL, Luhanik JM (1981) A storage study of ethanol in rabbit and human bone marrow. Forensic Sci Int 17:191–196
Winek CL, Matejczyk RJ, Buddie EG (1983) Blood, bone marrow and eye fluid ethanol concentrations in putrefied rabbits. Forensic Sci Int 22:151–159
Winek CL, Pluskota M, Wahba WW (1982) Plasma versus bone marrow flurazepam concentration in rabbits. Forensic Sci Int 19:155–163
Winek CL, Susa D (1982) Blood versus bone marrow methanol concentrations in rabbits. Forensic Sci Int 19:165–175
Winek CL, Westwood SE, Wahba WW (1990) Plasma versus bone marrow desipramine: a comparative study. Forensic Sci Int 48:49–57
Lafreniere NM, Watterson JH (2009) Detection of acute fentanyl exposure in fresh and decomposed skeletal tissues. Forensic Sci Int 185:100–106
Lafreniere NM, Watterson JH (2010) Detection of acute fentanyl exposure in fresh and decomposed skeletal tissues: Part II. The effect of dose-death interval. Forensic Sci Int 194:60–66
Vandenboer TC, Grummett SA, Watterson JH (2008) Utility of immunoassay in drug screening in skeletal tissues: sampling considerations in detection of ketamine exposure in femoral bone and bone marrow following acute administration using ELISA. J Forensic Sci 53:1474–1482
Watterson J (2006) Challenges in forensic toxicology of skeletonized human remains. Analyst 131:961–965
Watterson JH, Botman JE (2009) Detection of acute diazepam exposure in bone and marrow: influence of tissue type and the dose-death interval on sensitivity of detection by ELISA with liquid chromatography tandem mass spectrometry confirmation. J Forensic Sci 54:708–714
Watterson JH, Vandenboer TC (2008) Effects of tissue type and the dose-death interval on the detection of acute ketamine exposure in bone and marrow with solid-phase extraction and ELISA with liquid chromatography-tandem mass spectrometry confirmation. J Anal Toxicol 32:631–638
Blebea JS, Houseni M, Torigian DA, Fan C, Mavi A, Zhuge Y et al (2007) Structural and functional imaging of normal bone marrow and evaluation of its age-related changes. Semin Nucl Med 37:185–194
Hwang S, Panicek DM (2007) Magnetic resonance imaging of bone marrow in oncology, Part 1. Skeletal Radiol 36:913–920
Vande Berg BC, Malghem J, Lecouvet FE, Maldague B (2001) Normal bone marrow: dynamic aspects in magnetic resonance imaging. J Radiol 82:127–135
Derrickson B, Tortora GJ (2007) Principes d'anatomie et de physiologie. De Boeck, Bruxelles
Kierszenbaum AL (2006) Histologie et Biologie Cellulaire: Une introduction à l'anatomie pathologique. De Boeck, Bruxelles
Griffith JF, Yeung DK, Antonio GE, Lee FK, Hong AW, Wong SY et al (2005) Vertebral bone mineral density, marrow perfusion, and fat content in healthy men and men with osteoporosis: dynamic contrast-enhanced MR imaging and MR spectroscopy. Radiology 236:945–951
Fan C, Hernandez-Pampaloni M, Houseni M, Chamroonrat W, Basu S, Kumar R et al (2007) Age-related changes in the metabolic activity and distribution of the red marrow as demonstrated by 2-deoxy-2-[F-18]fluoro-d-glucose-positron emission tomography. Mol Imaging Biol 9:300–307
Liney GP, Bernard CP, Manton DJ, Turnbull LW, Langton CM (2007) Age, gender, and skeletal variation in bone marrow composition: a preliminary study at 3.0 Tesla. J Magn Reson Imaging 26:787–793
Maniatis A, Tavassoli M, Crosby WH (1971) Factors affecting the conversion of yellow to red marrow. Blood 37:581–586
Gurevitch O, Slavin S, Feldman AG (2007) Conversion of red bone marrow into yellow—cause and mechanisms. Med Hypotheses 69:531–536
Bigelow CL, Tavassoli M (1984) Fatty involution of bone marrow in rabbits. Acta Anat Basel 118:60–64
Chen WT, Shih TT, Chen RC, Lo SY, Chou CT, Lee JM et al (2001) Vertebral bone marrow perfusion evaluated with dynamic contrast-enhanced MR imaging: significance of aging and sex. Radiology 220:213–218
Hwang S, Panicek DM (2007) Magnetic resonance imaging of bone marrow in oncology, Part 2. Skeletal Radiol 36:1017–1027
Rosen BR, Fleming DM, Kushner DC, Zaner KS, Buxton RB, Bennet WP et al (1988) Hematologic bone marrow disorders: quantitative chemical shift MR imaging. Radiology 169:799–804
Daldrup-Link HE, Henning T, Link TM (2007) MR imaging of therapy-induced changes of bone marrow. Eur Radiol 17:743–761
Aguayo A, Giles F, Albitar M (2003) Vascularity, angiogenesis and angiogenic factors in leukemias and myelodysplastic syndromes. Leuk Lymphoma 44:213–222
Panteli K, Zagorianakou N, Agnantis NJ, Bourantas KL, Bai M (2005) Clinical correlation of bone marrow microvessel density in essential thrombocythemia. Acta Haematol 114:99–103
Zetterberg E, Lundberg LG, Palmblad J (2004) Characterization of blood vessels in bone marrow from patients with chronic myeloid leukemia and polycythemia vera. Scand J Clin Lab Invest 64:641–647
Schloegl H, Rost T, Schmidt W, Wurst FM, Weinmann W (2006) Distribution of ethyl glucuronide in rib bone marrow, other tissues and body liquids as proof of alcohol consumption before death. Forensic Sci Int 156:213–218
Raikos N, Tsoukali H, Njau SN (2001) Determination of opiates in postmortem bone and bone marrow. Forensic Sci Int 123:140–141
Grellner W, Glenewinkel F (1997) Exhumations: synopsis of morphological and toxicological findings in relation to the postmortem interval. Survey on a 20-year period and review of the literature. Forensic Sci Int 90:139–591
Rothschild MA, Schmidt V, Schneider V (1996) Adipocere—problems in estimating the length of time since death. Med Law 15:329–335
William D, Haglund MHS (eds) (1997) Forensic taphonomy: the postmortem fate of human remains. CRC Press
Guillot E, de Mazancourt P, Durigon M, Alvarez JC (2007) Morphine and 6-acetylmorphine concentrations in blood, brain, spinal cord, bone marrow and bone after lethal acute or chronic diacetylmorphine administration to mice. Forensic Sci Int 166:139–144
Maeda H, Oritani S, Nagai K, Tanaka T, Tanaka N (1997) Detection of bromisovalum from the bone marrow of skeletonized human remains: a case report with a comparison between gas chromatography/mass spectrometry (GC/MS) and high-performance liquid chromatography/mass spectrometry (LC/MS). Med Sci Law 37:248–253
Ito S, Kudo K, Imamura T, Jitsufuchi N, Kimura K (1997) Detection of drugs and poisons in postmortem tissues—determination of paraquat in tissues of rabbits buried underground. Nihon Hoigaku Zasshi 51:83–88
Kojima T, Okamoto I, Miyazaki T, Chikasue F, Yashiki M, Nakamura K (1986) Detection of methamphetamine and amphetamine in a skeletonized body buried for 5 years. Forensic Sci Int 31:93–102
Maeda H, Zhu BL, Ishikawa T, Oritani S, Michiue T, Li DR et al (2006) Evaluation of post-mortem ethanol concentrations in pericardial fluid and bone marrow aspirate. Forensic Sci Int 161:141–143
Bévalot F, Dujourdy L, Fanton L, Cartiser N, Magné L, Besacier F et al (2008) Statistic interpretation of meprobamate concentrations in bone marrow, vitreous and bile. Proceedings of International Meeting of The International Association of Forensic Toxicologists, February 18–23, Washington, United States of America. Abstract K59, p 431
Bévalot F, Fanton L, Le Meur C, Malicier D (2005) Analysis of bone marrow in post mortem toxicology. Proceedings of XVII International Congress of the International Association of Forensic Sciences, August 21–26, Hong Kong, China. Abstract A0847, p 246
Akcan R, Hilal A, Daglioglu N, Cekin N, Gulmen MK (2009) Determination of pesticides in postmortem blood and bone marrow of pesticide treated rabbits. Forensic Sci Int 189:82–87
Gorczynski LY, Melbye FJ (2001) Detection of benzodiazepines in different tissues, including bone, using a quantitative ELISA assay. J Forensic Sci 46:916–918
Rochdi M, Sabouraud A, Baud FJ, Bismuth C, Scherrmann JM (1992) Toxicokinetics of colchicine in humans: analysis of tissue, plasma and urine data in ten cases. Hum Exp Toxicol 11:510–516
Takatori T, Tomii S, Terazawa K, Nagao M, Kanamori M, Tomaru Y (1991) A comparative study of diazepam levels in bone marrow versus serum, saliva and brain tissue. Int J Leg Med 104:185–188
Bal TS, Hewitt RW, Hiscutt AA, Johnson B (1989) Analysis of bone marrow and decomposed body tissue for the presence of paracetamol and dextropropoxyphene. J Forensic Sci Soc 29:219–223
Noguchi TT, Nakamura GR, Griesemer EC (1978) Drug analyses of skeletonizing remains. J Forensic Sci 23:490–492
Kudo K, Sugie H, Syoui N, Kurihara K, Jitsufuchi N, Imamura T et al (1997) Detection of triazolam in skeletal remains buried for 4 years. Int J Leg Med 110:281–283
Higuchi T, Kogawa H, Satoh M, Tatsuno M, Tsuchihashi H (1996) Application of high-performance liquid chromatography/mass spectrometry to drug screening. Am J Forensic Med Pathol 17:21–23
Nagata T, Kimura K, Hara K, Kudo K (1990) Methamphetamine and amphetamine concentrations in postmortem rabbit tissues. Forensic Sci Int 48:39–47
Casier HT, Delaunois AL (1943) La répartition de l'alcool chez l'homme et les animaux au cours de l'intoxication éthylique. Arch Int Pharmacodyn 69:186
Isokoski M, Alha A, Laiho K (1968) Bone marrow alcohol content in cadavers. J Forensic Med 15:9–11
Hoiseth G, Karinen R, Johnsen L, Normann PT, Christophersen AS, Morland J (2008) Disappearance of ethyl glucuronide during heavy putrefaction. Forensic Sci Int 176:147–151
Helander A, Dahl H (2005) Urinary tract infection: a risk factor for false-negative urinary ethyl glucuronide but not ethyl sulfate in the detection of recent alcohol consumption. Clin Chem 51:1728–1730
Schloegl H, Dresen S, Spaczynski K, Stoertzel M, Wurst FM, Weinmann W (2006) Stability of ethyl glucuronide in urine, post-mortem tissue and blood samples. Int J Leg Med 120:83–88
Helander A, Hagelberg CA, Beck O, Petrini B (2009) Unreliable alcohol testing in a shipping safety programme. Forensic Sci Int 189:e45–e47
Helander A, Olsson I, Dahl H (2007) Postcollection synthesis of ethyl glucuronide by bacteria in urine may cause false identification of alcohol consumption. Clin Chem 53:1855–1857
Baranowski S, Serr A, Thierauf A, Weinmann W, Grosse Perdekamp M, Wurst FM et al (2008) In vitro study of bacterial degradation of ethyl glucuronide and ethyl sulphate. Int J Leg Med 122:389–893
Halter CC, Laengin A, Al-Ahmad A, Wurst FM, Weinmann W, Kuemmerer K (2009) Assessment of the stability of the ethanol metabolite ethyl sulfate in standardised degradation tests. Forensic Sci Int 186:52–55
Hoiseth G, Karinen R, Christophersen A, Morland J Practical use of ethyl glucuronide and ethyl sulfate in postmortem cases as markers of antemortem alcohol ingestion. Int J Legal Med 124:143–148
Fanton L, Bevalot F, Gustin MP, Paultre CZ, Le Meur C, Malicier D (2009) Interpretation of drug concentrations in an alternative matrix: the case of meprobamate in bile. Int J Leg Med 123:97–102
Sato Y, Kondo T, Takayasu T, Ohshima T (2000) Detection of methamphetamine in a severely burned cadaver—a case report. Nihon Hoigaku Zasshi 54:420–424
Acknowledgements
The authors would like to express their gratitude to Dr. Martine French for providing the pictures of histologic sections of bone marrow (Fig. 1).
Figure 2 was reprinted from Seminars in Nuclear Medicine, 37(3), Judy S. Blebea, Mohamed Houseni, Drew A. Torigian, Chengzhong Fan, Ayse Mavi, Ying Zhuge, Tad Iwanaga, Shipra Mishra, Jay Udupa, Jiyuan Zhuang, Rohit Gopal, and Abass Alavi, Structural and Functional Imaging of Normal Bone Marrow and Evaluation of its Age-Related Changes, pages 186, Copyright (2010), with permission from Elsevier.
Nathalie Cartiser is grateful to ‘Association Nationale de la Recherche et de la Technologie, Service CIFRE’ for the PhD grant.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cartiser, N., Bévalot, F., Fanton, L. et al. State-of-the-art of bone marrow analysis in forensic toxicology: a review. Int J Legal Med 125, 181–198 (2011). https://doi.org/10.1007/s00414-010-0525-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-010-0525-6