Abstract
Investigating toxicological causes of death may require alternative matrices when the usual ones are lacking. Whereas forensic toxicology uses bile almost only for xenobiotic screening, a diagnostic test interpreting postmortem bile concentrations of meprobamate is reported. Based on 128 sets of autopsy data, its intrinsic qualities were good, with 0.95 sensitivity and 0.93 specificity. In a French forensic population, the positive and negative predictive factors were 0.90 and 0.97, respectively. It is a useful means of revealing overdoses where blood samples are not available or of confirming blood tests when postmortem redistribution is suspected.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Postmortem toxicology is part of the arsenal systematically deployed in investigating causes of death [1]. Analysis is usually based on blood sampling, as providing the best toxicological profile of the victim at the time of death. The interpretation of blood concentrations is, however, subject to postmortem redistribution effects and is obviously impossible when no blood is available [2, 3]. Alternative matrices are then useful, the main drawback being the lack of standard tables defining therapeutic, toxic, and lethal thresholds such as are available for blood [4, 5]. Interpretation has therefore been empirical, with typical intoxication data found in the literature serving as benchmarks [6]. The relative unreliability of such an approach has meant that therapeutic and intoxication levels are difficult to distinguish. Quantitative statistical comparisons of data from alternative matrices are required; therefore, concentration distributions concomitantly observed in blood and bile were investigated. Bile is a xenobiotic elimination compartment providing a matrix of choice for screening [7, 8]. Except in the case of alcohol [9–11], most studies concerning bile have focused on the simple detection of xenobiotics rather than the interpretation of the concentrations detected. A preliminary study assessed the interest of bile as a matrix for revealing overdose of a three-molecule therapy often encountered in forensic toxicology [12], and the bile thresholds for meprobamate and cyamemazine were determined graphically. These encouraging results were therefore followed up, in the light of the forensic importance of meprobamate [13–15], with the present methodologically rigorous assessment.
Materials and methods
Study population
A retrospective study was performed in the Lyon (France) Forensic Institute between June 1st 2004 and August 31st 2007. Sampling respected the Council of Europe Circular R99 [1]. All cases in which meprobamate had been detected in at least one matrix (blood, gastric content, and/or urine) and from which a bile sample had been taken were included. Meprobamate was detected in 5.9% (n = 185) of the 3,116 autopsies performed over the study period. Simultaneous blood and bile samples were taken in 67% of the positive cases (n = 124). For these 124 cases included in the statistic analysis, postmortem times varied from a few hours to several days. The male to female ratio was 1.2. For the men, the mean age was 50 years (range, 18–91 years); for the women, it was 48 years (range, 24–80 years).
Analytical methods
Toxicological screening on biological samples was performed by high-performance liquid chromatography with photodiode array detection (HPLC/DAD) and gas chromatography with mass spectrometry detection (GC/MS) as previously described [16]. The samples (blood and urine, 1 ml; gastric content and bile, 0.5 ml), spiked with phenazine (750 ng) as internal standard, were extracted using Toxitube A from Varian (Les Ulis, France). For HPLC/DAD analysis, the dry residue was dissolved in 100 μl HPLC initial mobile phase (described below), and 60 μl was injected. The HPLC chain was an 1100 series from Agilent (Massy, France). The analytical column was a 250 × 4.6 mm ID Uptisphère C8 Interchrom, 5 μm particle size from Interchim (Montluçon, France). The solvent gradient program, composed of a 50 mmol mixture of acetonitrile/phosphate buffer, pH 3.6, was as follows: initial acetonitrile was held at 15% for 2 min, linearly increased to 65% for 13 min and to 80% for 10 min. Compounds were identified using the “UV spectra of toxic compounds” version 2001 library (Authors: Pragst, Herzler, Herre, Erxleben and Rothe) commercially available (FILT Forschungsgesellschaft mbH, Berlin-Buch, Germany) and a home-made library. For GC/MS, the dry residue was acetylated by the method described by Maurer [17] and modified as follows: 200 μl of pyridine/acetic anhydride mixture (40/60, v/v) was added to dry residue for 30 min at 60°C then evaporated and re-dissolved in 100 μl ethyl acetate, and 1 μl was injected. The GC/MS chain was an Agilent 6890 GC with a 5973 mass spectrum detector. The column was an HP5MS (length, 30 m; 0.25 mm ID; film thickness, 0.25 μm). The gas vector was helium at 1 ml/min flow. Injector temperature was 260°C. The oven temperature gradient program was as follows: initial temperature 90°C held 1 min, linearly increased to 200°C (20°C/min), and then to 300°C (15°C/min). Compounds were identified using three commercial libraries from Agilent: Wiley, NIST 02, Pfleger Maurer Weber V3, and a home-made library. The meprobamate assay of calibration points, standards, and unknowns was performed as follows: 850 μl distilled water and 50 μl methanol solution at 1 mg/ml in carisoprodol (internal standard) were added to 100 μl bile or 500 μl blood. The mixtures were diluted in 2 ml ammoniac buffer (pH = 9.5) and extracted with 3 ml of a chloroform–isopropanol (9:1) mixture. After 20 min agitation and 10 min centrifugation at 2,700 rpm, the organic phase was collected and evaporated on warm (40°C) nitrogen. The dry residue was dissolved in 500 μl methanol and centrifuged for 10 min at 12,000 rpm. Aliquots of 1 μl were injected into the GC/MS system, using Gaillard’s method modified as follows [14]: The gas chromatograph was a Hewlett Packard 6890 series (Les Ulis, France), with HP 7683 automatic injector and HP 5973 detector. The analytic column was an HP-5MS capillary column (30 m × 0.25 mm i.d.; 0.25 μm film thickness). Helium was used as vector at a constant flow rate of 1.4 ml/min. A splitless injection mode was adopted at a temperature of 193°C. The initial oven temperature of 150°C was maintained for 1 min then increased to 200°C at 25°C/min then to 295°C at 30°C/min and maintained for 16 min. The mass spectrometer scanned ions of mass m/z 40–200.
Statistics
Bile detection threshold for a given blood concentration
Concentrations detected in blood but not in bile-enabled meprobamate bile detection threshold to be defined as the upper limit of the 95% unilateral dispersion interval for the blood concentration values.
Correlation between bile and blood concentrations
Correlation coefficient for subjects in whom meprobamate was detected in bile showed a linear relationship between bile and blood concentration values. We estimate the significance level of the correlation coefficient when computing the p value of the usual two-tailed Student’s t test with (n − 2) degrees of freedom, with n the sample size.
Meprobamate overdose test
It is generally agreed that an overdose can be suspected for a blood meprobamate concentration in excess of 50 mg/l [4, 5]. Our meprobamate overdose diagnosis test was based on determining the bile meprobamate concentration threshold above which a subject will be considered overdose-positive, i.e., as likely to have a blood meprobamate concentration >50 mg/l. As in a biological test, sensitivity was based on the proportion of positive results for subjects presenting a blood meprobamate concentration >50 mg/l and specificity on the proportion of negative results for subjects presenting a blood meprobamate concentration <50 mg/l. Denoting α the risk of obtaining a false-positive result in a subject with a non-toxic blood concentration and β the risk of a false negative in a subject with a toxic blood concentration, the specificity can be expressed as (1 − α) and the sensitivity as (1 − β). The optimal bile concentration threshold for the test was thus derived from the specificity (1 − α) and sensitivity (1 − β) and specificity (1 − α) values for bile concentrations between 0 and 373 μg/ml. The risks α and the β were calculated for each bile concentration. The optimal bile concentration threshold was that at which these two risks were minimal, defining the test threshold and corresponding sensitivity and specificity values. Bayes’ formula gave the positive and negative predictive values of the test by applying it to a population known to have meprobamate in the blood and in which the proportion of toxic concentrations was known. As with all methods of diagnostic test, we gave the receiver operating characteristics (ROC) [18] curve.
Results
Calibration curve and validation
Calibration curves were linear for blood (r 2 = 0.997; six calibration points, 12.5, 25.0, 50.0, 100.0, 200.0, and 400.0 mg/l; in triplicate) and for bile (r 2 = 0.994; six calibration points, 10.0, 25.0, 50.0, 100.0, 125.0, and 250.0; in triplicate). For each curve, the intercept did not significantly differ from zero (Student’s t test). Homogeneity of variances was confirmed on Cochran’s test over the whole test range. Repeatability, reproducibility, and recovery were tested at low (blood = 25 mg/l, bile = 25 mg/l) and high concentration levels (blood = 200 mg/l, bile = 125 mg/l). The repeatability study (each of the two concentration levels analyzed ten times) gave variation coefficients for blood of 2.0% and 3.1% and for bile of 5.2% and 4.9% for the low and high levels, respectively. The reproducibility study (each of the two concentration levels analyzed ten times 3 days consecutively) gave variation coefficients for blood of 5.0% and 9.2% and for bile of 4.8% and 9.1% for the low and high levels, respectively. Mean recovery was 82% and 73% for blood and 94% and 101% for bile for the low and high levels, respectively. The limit of detection (LOD, three standard deviations from the mean concentration measured on ten blank blood and bile samples) was 1.2 and 2.9 mg/l for blood and bile, respectively. The lower limit of quantitation (LOQ, ten standard deviations from the mean concentration measured on ten blank bile and blood samples) was 2.0 and 5.9 mg/l for blood and bile, respectively.
Statistics
Detection threshold
Those cases in which meprobamate was detected in blood but not in bile (n = 13) provided an estimate of the blood meprobamate concentration threshold for bile detection: 95% of blood concentration values lower than 7.9 mg/l failed to be detected in bile at an analytic threshold of 2.9 mg/l.
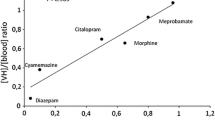
Correlation study
Figure 1 shows the pairs of values found in those cases (n = 111) in which bile meprobamate was quantifiable. There was a significant linear correlation between bile and blood meprobamate concentrations (r = 0.66, p < 10−14). For strong blood concentrations (≥100 mg/l), however, the relative bile concentrations were more variable. Two subjects presented high relative bile concentrations (two and four times the mean, respectively).
Overdose test
Table 1 shows the sensitivity and specificity values and summed α + β error risks for bile concentration thresholds ranging between 0 and 373 mg/l by 10 mg/l steps. Estimates were based on 124 subjects with concentrations above (n = 49) and below (n = 75) the overdose blood concentration threshold of 50 mg/l. Figure 2 shows the summed α + β error risks per threshold value. The threshold associated with the minimal total risk was 53 mg/l and was therefore taken as the test detection threshold, with an associated sensitivity of 0.95 and specificity of 0.93. The ROC curve has an usual shape and could be compared with subsequent ROC curves obtained from biological tests performed in different matrices (Fig. 2). Applying the test to the parent population of the sample, where the intoxication rate for subjects presenting blood meprobamate was 40%, the positive and negative predictive values were 90% and 97%, respectively.
Discussion
This original study concerned the rigorous development of a simple diagnostic test in forensic toxicology, based on a significant correlation established between blood and bile meprobamate concentrations in a representative sample (n = 124) drawn from a French forensic autopsy population. A bile concentration threshold of 53 mg/l was found to be statistically equivalent to the blood concentration threshold of 50 mg/l distinguishing overdose from therapeutic use. The test showed good intrinsic qualities of sensitivity and specificity and excellent predictive values when applied to a forensic population. It can be used where blood sampling is not feasible or to confirm blood sample findings when postmortem redistribution may be suspected.
The greater dispersion of bile as compared to blood concentrations may be explained by antemortem elimination and/or postmortem redistribution. The bile/blood concentration ratio at the moment of death is influenced by individual variation in pharmacokinetic and toxicokinetic elimination models. Influencing factors include hepatic perfusion status [19], liver pathologies such as cirrhosis and cholestasis [20], and drug interactions [21, 22]. The interval between meprobamate ingestion and death is also a factor: A short interval could account for a low bile as compared to blood concentration due to limited excretion; conversely, prolonged agony would tend to augment the bile concentration. The postmortem redistribution mechanisms liable to affect bile concentrations are not clearly understood, although methylendioxymetamphetamine studies showed them not to be greatly significant [23]. Such antemortem and postmortem variation factors are not readily controlled, but seem to be particularly relevant to high blood concentrations: It is noteworthy that variation in bile-to-blood concentrations was fairly low in the regions involved in determining the test’s overdose threshold, limiting the influence of these factors on the exact threshold value. Thus, a threshold can be set with good sensitivity and specificity.
Determining the bile meprobamate concentration overdose threshold corresponding to a blood threshold is directly inspired by the methodology for constructing clinical biology diagnostic tests based on measurable values. Meprobamate overdose is diagnosed on the basis of a reading greater or lesser than a certain value. The biological variable establishing diagnosis is thus the bile concentration of meprobamate. This rigorous approach raises the question of the quality of the estimation of sensitivity and specificity values and of α and β risks. Two arguments, however, suggest reasonable estimation fluctuation. The first concerns the narrow sensitivity and specificity confidence intervals for the selected threshold with a precision coefficient of about 7%. The second is based on the regularity of the total risk (α + β) calculated for the various bile thresholds, which was such that a minimum total risk proved easy to determine. Should one be preferentially seeking high specificity, as in a case where an alternative cause of death might be envisaged, Table 1 would enable a threshold with higher specificity to be selected.
The test enables an overdose threshold to be detected in the bile statistically corresponding to a blood concentration greater than 50 mg/l. Being based on blood concentration data, the test is subject to the associated limits of interpretation. Two issues arise: The first is the statistical problem of determining a blood toxicity threshold not found in the literature. The second concerns the interpretation of overdose, which must be seen in the forensic context. Sample recruitment involved all the common forensic situations, in terms of cause of death, postmortem time, age, etc. The sample being highly representative, the test can be taken as having a broad field of application. Applying our proposed threshold to four cases found in the literature did indeed confirm the relevance of our test [24–26].
Carisoprodol, which is metabolized to meprobamate, is frequently detected during forensic autopsies in the countries where it is commercialized [27]. We use it as internal standard since this molecule is not disposable as therapeutic in France. If despite this limitation a subject would have ingested this substance, we would have detected it during the screening procedure by GC/MS. None of the included cases being carisoprodol positive, we cannot extrapolate our results to cases for which meprobamate is the result of carisoprodol intake.
It would be of future interest to model the postmortem evolution of the biliary compartment to explore some of the hypotheses put forward in this paper.
References
Mangin P (2002) Autopsie médico-légale. Rev Prat 52:723–728
Pounder DJ, Jones GR (1990) Post-mortem drug redistribution—a toxicological nightmare. Forensic Sci Int 45:253–263
De Letter EA, Lambert WE, Bouche MP, Cordonnier JA, Van Bocxlaer JF, Piette MH (2007) Postmortem distribution of 3,4-methylenedioxy-N,N-dimethyl-amphetamine (MDDM or MDDA) in a fatal MDMA overdose. Int J Legal Med 121:303–307
Flanagan RJ (1998) Guidelines for the interpretation of analytical toxicology results and unit of measurement conversion factors. Ann Clin Biochem 35(Pt 2):261–267
TIAFT reference blood level list of therapeutic and toxic substances (2005) Available from: http://www.tiaft.org/. Cited July 2007 (database on the Internet)
Musshoff F, Padosch S, Steinborn S, Madea B (2004) Fatal blood and tissue concentrations of more than 200 drugs. Forensic Sci Int 142:161–210
Agarwal A, Lemos N (1996) Significance of bile analysis in drug-induced deaths. J Anal Toxicol 20:61–63
Vanbinst R, Koenig J, Di Fazio V, Hassoun A (2002) Bile analysis of drugs in postmortem cases. Forensic Sci Int 128:35–40
Winek CL, Esposito FM (1981) Comparative study of ethanol levels in blood versus bone marrow, vitreous humor, bile and urine. Forensic Sci Int 17:27–36
Kugelberg FC, Jones AW (2007) Interpreting results of ethanol analysis in postmortem specimens: a review of the literature. Forensic Sci Int 165:10–29
Kass K, Szlavik N, Klausz G, Rona K (2006) Epebol torteno etilalkohol meghatarozas jelentosege az igazsagugyi orvostani gyakorlatban (in Hungarian). Acta Pharm Hung 76:133–137
Bévalot F, Fanton L, Le Meur C, Malicier D (2005) Interpretation of biliary drug concentrations: case of cyamemazine, meprobamate and nordazepam. Proceeding of the 17Th Meeting of International Association of Forensic Sciences, Hong Kong, China p. 467
Felby S (1970) Concentrations of meprobamate in the blood and liver following fatal meprobamate poisoning. Acta Pharmacol Toxicol (Copenh) 28:334–337
Gaillard Y, Billault F, Pepin G (1997) Meprobamate overdosage: a continuing problem. Sensitive GC-MS quantitation after solid phase extraction in 19 fatal cases. Forensic Sci Int 86:173–180
Osvath P, Fekete S (2003) A pszichofarmakonvalasztas jellemzoi ongyilkossagi kiserletekben (in Hungarian). Orv Hetil 144:121–124
Fanton L, Bevalot F, Schoendorff P, Le Meur C, Gaillard Y, Malicier D (2007) Fatal mephenesin intoxication. J Forensic Sci 52:221–223
Maurer HH (1992) Systematic toxicological analysis of drugs and their metabolites by gas chromatography-mass spectrometry. J Chromatogr 580:3–41
Fink H, Luppa P, Mayer B, Rosenbrock H, Metzger J, Martyn JA et al (2003) Systemic inflammation leads to resistance to atracurium without increasing membrane expression of acetylcholine receptors. Anesthesiology 98:82–88
Peeters MY, Aarts LP, Boom FA, Bras LJ, Tibboel D, Danhof M et al (2008) Pilot study on the influence of liver blood flow and cardiac output on the clearance of propofol in critically ill patients. Eur J Clin Pharmacol 64:329–334
Delco F, Tchambaz L, Schlienger R, Drewe J, Krahenbuhl S (2005) Dose adjustment in patients with liver disease. Drug Safety 28:529–545
Angelin B, Arvidsson A, Dahlqvist R, Hedman A, Schenck-Gustafsson K (1987) Quinidine reduces biliary clearance of digoxin in man. Eur J Clin Invest 17:262–265
Shitara Y, Sato H, Sugiyama Y (2005) Evaluation of drug-drug interaction in the hepatobiliary and renal transport of drugs. Annu Rev Pharmacol Toxicol 45:689–723
De Letter EA, Clauwaert KM, Belpaire FM, Lambert WE, Van Bocxlaer JF, Piette MH (2002) Post-mortem redistribution of 3,4-methylenedioxymethamphetamine (MDMA, “ecstasy”) in the rabbit. Part I: experimental approach after in vivo intravenous infusion. Int J Legal Med 116:216–224
Maes R, Hodnett N, Landesman H, Kananen G, Finkle B, Sunshine I (1969) The gas chromatographic determination of selected sedatives (ethchlorvynol, paraldehyde, meprobamate, and Carisoprodol) in biological material. J Forensic Sci 14:235–254
Kintz P, Tracqui A, Mangin P, Lugnier AA (1988) Fatal meprobamate self-poisoning. Am J Forensic Med Pathol 9:139–140
Hoizey G, Canas F, Binet L, Bernard MH, Lamiable D (2007) Concentrations tissulaires post-mortem du méprobamate. Proceedings of the XVth meeting of the French Society of Analytical Toxicology (SFTA), Paris p. 72
Hoiseth G, Bramness JG, Christophersen AS, Morland J (2007) Carisoprodol intoxications: a retrospective study of forensic autopsy material from 1992–2003. Int J Legal Med 121:403–409
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fanton, L., Bevalot, F., Gustin, M.P. et al. Interpretation of drug concentrations in an alternative matrix: the case of meprobamate in bile. Int J Legal Med 123, 97–102 (2009). https://doi.org/10.1007/s00414-008-0259-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-008-0259-x