Abstract
The postmortem redistribution (PMR) phenomenon complicates interpretation in forensic toxicology. Human data on time-dependent PMR are rare and only exist for blood so far. A new method for investigation of time-dependent PMR in blood as well as in alternative body fluids and tissues was developed and evaluated using automated biopsy sampling. At admission of the bodies, introducer needles were placed in liver, lung, kidney, muscle, spleen, adipose tissue, heart, femoral vein, and lumbar spine using a robotic arm guided by a computed tomography scanner (CT). Needle placement accuracy was analyzed and found to be acceptable for the study purpose. Tissue biopsies and small volume body fluid samples were collected in triplicate through the introducer needles. At autopsy (around 24 h after admission), samples from the same body regions were collected. After mastering of the technical challenges, two authentic cases were analyzed as a proof of concept. Drug concentrations of venlafaxine, O-desmethylvenlafaxine, bromazepam, flupentixol, paroxetine, and lorazepam were determined by LC-MS/MS, and the percentage concentration changes between the two time points were calculated. Concentration changes were observed with both increases and decreases depending on analyte and matrix. While venlafaxine, flupentixol, paroxetine, and lorazepam generally showed changes above 30 % and more, O-desmethylvenlafaxine and bromazepam did not undergo extensive PMR. The presented study shows that CT-controlled biopsy collection provides a valuable tool for systematic time-dependent PMR investigation, demanding only minimal sample amount and causing minimal damage to the body.

New strategy for time-dependent postmortem redistribution studies by CT guided biopsy sampling prior to autopsy and comparison of drug concentrations at these two time points using validated LC-MS/MS quantitation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In postmortem toxicology, the severity of a given intoxication is generally assessed in the light of the blood concentration of a pharmacologically or toxicologically active compound, for which reference values in living people such as “therapeutic,” “toxic,” or “lethal” levels are consulted [1]. However, numerous biochemical and biological processes such as pH changes, lysis of cells and membranes begin immediately after death and may render the calculated drug concentration unreliable. Blood concentration changes can be observed in both directions, e.g., due to degradation or formation by bacteria and drug instability or due to postmortem redistribution (PMR), thus leading to decreased or increased blood concentration levels. Therefore, interpretation of blood concentrations as “therapeutic,” “toxic,” or even “lethal” cannot simply be translated from living reference values to postmortem cases. The often described and studied issue resulting in changing blood concentrations after death is the so-called PMR. It is believed to occur by diffusion of drug from tissue-bound stores with higher concentrations adjacent to blood vessels into blood after death, thus leading to increasing blood concentrations [1–3]. It seems to be strongly dependent on analyte characteristics and the individual case circumstances such as the distribution of the analyte at time of death [1]. Although the presence of PMR is a well-recognized phenomenon in forensic toxicology, it is still under-explored. Systematic studies on PMR are rare and the postmortem concentration changes are still unpredictable for the majority of analytes. Estimations were made based on physicochemical properties of substances such as pKa or lipophilicity. It appears that lipophilic drugs that have an apparent volume of distribution (Vd) > 3 L/kg are candidates for PMR [4–7]. However, prediction of PMR cannot be done only based on Vd as the correlation is not very strong [8]. Basic drugs are believed to be prone to PMR due to their increased ionization in the more acidic environment after death. Drugs with a high concentration ratio between central and peripheral blood (C/P ratio) are believed to undergo PMR more likely than others [3]. Blood from peripheral sites—usually obtained from the femoral vein—is mostly agreed to be the matrix of choice for postmortem quantitation of xenobiotics because of its distance from central organs and gastrointestinal tract [4, 9]. However, recent studies have shown that the extent of PMR also depends on the postmortem interval (PMI) and does not reliably correlate with physicochemical or pharmacodynamical properties of the drugs [10–13]. Even peripheral blood was shown to exhibit massive time-dependent PMR with drug concentrations decreasing or increasing up to 300 % [4, 11, 14]. Time-dependent changes in femoral or central blood were assessed only in a few human studies [4, 10–18]. The most important quantitative changes seem to occur very rapidly during the first 24 h after death, as could be shown in animal models, where sampling could be performed at defined times [19, 20]. A thorough investigation on redistribution in humans was that by Prouty and Anderson [4], where blood samples from the subclavian vein, heart chambers, and femoral vein were obtained at autopsy, and then again at least 2 h later. They found that blood drug concentrations are site-dependent and increase with time, but that blood from peripheral sites appeared to be less affected by these changes. From the available human data on redistribution over time, it also appears that it mainly occurs in the early postmortem period, prior to the putrefaction stage [4, 21].
In addition, blood is not always available in death cases due to, e.g., putrefaction processes or exsanguination. In these cases, alternative matrices such as muscle, liver, or kidney have to be considered for toxicological analysis [22]. However, the interpretation of quantitation results in alternative postmortem matrices provides even more pitfalls due to lacking reference values and/or unpredictable PMR processes. Various publications (mainly case reports) exist that investigated the site-dependent differences within and between human tissues [23–25]. However, time-dependent studies on postmortem concentration changes in organs and tissues that might provide better insights into possible distribution processes are not available at all, as usually organ and tissue samples can only be collected after opening of the corpse. PMR within solid tissues can only be assumed based on site-dependent concentration differences in samples taken at autopsy. Nevertheless, information about time-dependent redistribution in tissues and organs is needed in forensic toxicology as these matrices are used for forensic investigations and such information will further improve understanding of diffusion and distribution processes.
The ultimate challenge in systematic time-dependent redistribution studies is the appropriate sampling at two or more different time points, assuring that, e.g., blood is actually collected twice from the femoral vein. Until recently, collection of tissue and organ samples at various different time points seemed to be impossible without opening of the body. Postmortem biopsy sampling under computed tomography (CT) control should overcome this problem. Therefore, the aim of the presented study was to develop and evaluate a new sampling technique using CT-controlled biopsy sampling of various body fluids and tissues at two time points after death for more thorough time-dependent PMR studies. This new technology combined with a recently published advanced LC-MS/MS method [26] should pave the way for further studies on time-dependent PMR.
Materials and methods
Chemicals and reagents
Methanolic or acetonitrilic solutions (1 mg/mL) of bromazepam, flupentixol, lorazepam, paroxetine, venlafaxine, and O-desmethylvenlafaxine (ODMV) and methanolic solutions of the deuterated internal standards (IS, 0.1 mg/mL) alprazolam-d5, aripiprazole-d8, lorazepam-d4, paroxetine-d6, and venlafaxine-d6 were obtained from Lipomed (Arlesheim, Switzerland) or Cerilliant (delivered by Sigma-Aldrich, Buchs, Switzerland). Water was purified with a Purelab Ultra millipore filtration unit (Labtech, Villmergen, Switzerland) and acetonitrile of HPLC grade was obtained from Fluka (Buchs, Switzerland). All other chemicals used were from Merck (Zug, Switzerland) and of the highest grade available.
Postmortem samples
Samples from the femoral veins (peripheral blood, pB) and the heart (heart blood, HB), cerebrospinal fluid (CSF) from the lumbar spine, urine, muscle, liver, kidney, lung, spleen and adipose tissue (AT) were obtained from postmortem cases that were submitted to the authors’ laboratory and autopsied by order of the state attorneys.
Virtobot system
The Virtobot system consists of a Siemens Somatom Definition Flash Dual Source computed tomograph (CT) (Siemens Healthcare, Erlangen, Germany) coupled to a robotic arm (Staeubli TX90L, Staeubli AG, Pfaeffikon, Switzerland) which is fixed to the ceiling of the CT room. The robotic arm can be extended with different modules such as a surface scanner, digital cameras, or a navigated biopsy module. The biopsy module is equipped with passive retroreflective trackers (CamBar B2, Axios 3D, Oldenburg, Germany) which can be tracked by the wall-mounted optical tracking system (CamBar B2, Axios 3D, Oldenburg, Germany) to confirm positioning. The custom-made biopsy module (Integrated Microsystems Austria GmbH, Wiener Neustadt, Austria) enables precise placement of introducer needles into specific areas of a human body based on the CT data. The Virtobot system is displayed in Fig. 1.
The planning of needle trajectories is performed on a custom made navigation system. On the navigation computer, the CT dataset is loaded into the planning and navigation software to create a performance plan. For each desired needle trajectory, a target point and an entry point on the body as well as the rotation of the robotic head are defined. Once the performance plan is completed, it is transferred to the robot control software for execution. For each needle trajectory in the performance plan, the robot executes a biopsy cycle. It fetches a coaxial introducer needle (13 gauge × 10.3 cm, Argon Medical Devices, Athens, TX, USA) from the needle magazine and aligns the introducer needle with the planned needle trajectory with the tip of the needle at the entry point of the needle trajectory. The needle position is verified with help of the optical tracking system and corrected if necessary. The needle is inserted up to the target point by extending the linear pneumatic actuator of the biopsy end-effector and released from the gripper. After the placement, the introducer needles can be used to collect body fluids by attaching a syringe or as channels for placing biopsy core needles as described below. A detailed description of the process can be found under [27].
Evaluation of the Virtobot system for biopsy sampling
To evaluate the accuracy of robotic needle placement in two authentic cases, the coordinates that were defined on the navigation computer were compared to the effective needle coordinates determined in the CT control scans. The used biopsy needles remove a 22-mm-long cylinder of tissue. The top of the introducer needle was therefore placed with an offset of 11 mm in order to gather the tissue sample from the exact position defined as target point during planning. The absolute distances between the target points of the planned and the effective needle positions were compared, as well as the components of the distances orthogonal and longitudinal to the planned trajectory.
Analyte distribution within sampling target area
The homogeneity of drug distribution within the sampling target area was investigated in preliminary experiments. From liver and kidney tissue, five samples of approximately 20 mg weight were collected within a region of 2 × 2 × 1 cm in four different cases each. Drug concentrations of all analytes detected were determined by liquid-chromatography mass spectrometry (LC-MS/MS) as described below and in detail in Ref. [26] and relative standard deviations (RSD) were calculated.
Final sampling procedure
Biopsy sampling at first time point (t1)
After a routine CT imaging procedure, introducer needles were placed into the right heart ventricle, the right lung, the right lobe of the liver, the right kidney, the spleen, the subcutaneous adipose tissue of the waist, the muscle tissue at the upper left thigh, the right femoral vein, and the dural sac at the level of the lumbosacral junction. The needles were placed in supine position of the body except for the dural sac, kidney, and spleen, which were placed in prone position if the distance from the body surface exceeded the length of the introducer needle. After placement of the introducer needles, another CT scan was performed to verify the needle positions. From the right heart ventricle and the femoral vein, 1 mL blood and from the lumbar spine, 1 mL CSF was collected using a 5-mL syringe. Biopsies from tissues and organs were collected using a Bard® Magnum® reusable core biopsy pistol (Bard Magnum, Bard Biopsy Systems, Tempe, AZ, USA) with a biopsy core needle (14 gauge × 16 cm, Argon Medical Devices, Athens, TX, USA) with a throw length of 22 mm. The introducer needles were used as guidance tubes for the biopsy collection system. Therefore, the collected tissue was located approx. 22 mm below the introducer needle. Biopsies were collected in triplicates from all matrices. Directly after sample collection, the biopsies were weighted into 2-mL Metal Bead Lysing Matrix tubes (MP Biomedicals, Illkirch, France). The body fluids were aliquoted in triplicates of 20 μL into 2-mL Eppendorf Safe Lock Tubes (Schoenenbuch, Switzerland). All samples were stored at −20 °C until analysis.
Sampling at second time point (t2)
At autopsy, samples from the same locations were collected where biopsies had been taken the day before. From tissues and organs approx. 1 cm3 was collected and from the body fluids 1 mL each. After autopsy, the tissues and organs were aliquoted into triplicates of approx. 20 mg and body fluids into triplicates of 20 μL. All samples were stored at −20 °C until analysis.
Applicability and proof of concept
Two cases with suspected poisoning were chosen for an initial applicability study. Sampling was performed as described above, with dural sac, kidney, and spleen collected in prone position, as the distance from the body surface exceeded the length of the introducer needle. Autopsy was performed the day after biopsy sampling which lead to time intervals of 22 and 21 h between the first and the second sampling time point for cases 1 and 2, respectively. Heart blood was routinely screened for drugs using a different LC-MS/MS screening method including enhanced product ion scans and comparison of the mass spectra with an in-house library. Identified drugs were quantified with the LC-MS/MS method as described below in all fluids, tissues, and organs (78 analyses per case). Percent concentration differences between t1 and t2 were calculated setting mean of t1 to 100 %. A nonparametric Mann–Whitney test (p < 0.05) was applied for statistical evaluation between time points using GraphPad Prism 6.0 (GraphPad Software, La Jolla, CA, USA).
Sample preparation and LC-MS/MS procedure
All samples belonging to the same case were extracted and analyzed in the same batch on the same day. Sample preparation and analysis were performed according to Staeheli et al. [26]. Briefly, organ and tissue samples were homogenized using a Fast Prep®-24 Instrument (MP Biomedicals, Illkirch, France). To each sample, 50 μL IS mixture was added. Two liquid-liquid extractions (LLE) with butyl acetate/ethyl acetate (1:1, v/v) were performed, one at pH 7.4 and one at pH 13.5. The extracts were combined and evaporated to dryness. The sample was reconstituted in mobile phase and analyzed by LC-MS/MS. The analysis was performed using a Thermo Fischer Ultimate 3000 UHPLC system (Thermo Fisher, San Jose, California, USA) coupled to a Sciex 5500 QTrap linear ion trap quadrupole mass spectrometer (Sciex, Darmstadt/Germany). The MS was operated in the advanced scheduled multiple reaction monitoring (MRM) mode using three transitions for each analyte. The MS was controlled by Analyst® 1.6.2 software and quantitation was performed with MultiQuant® 2.1.1 software. The method was validated in terms of selectivity, crosstalk, matrix effects, extraction efficiency, accuracy, precision, and calibration model in postmortem femoral blood, HB, CSF, muscle, liver, kidney, spleen, lung, and AT for 83 analytes.
Results and discussion
Although forensic toxicologists are aware of the PMR effect, it is still under-explored. To provide better insight into time-dependent PMR processes in blood and especially in different postmortem tissues, a new sampling strategy using biopsy samples should be developed and evaluated for its usefulness in time-dependent PMR studies. Samples taken at admission of the corpse at the mortuary and again during autopsy should be collected and compared for concentration differences. Reliable conclusion of results can only be drawn if the applied sampling strategy is able to sample fluids and tissues in an accurate way, so that repeated sampling can be performed at close-by locations without opening of the corpse for the first sample collection.
Development of biopsy sampling strategy
The ultimate challenge for rather systematic human time-dependent redistribution studies is the appropriate sampling at two or more different time points, assuring that, e.g., blood is actually collected twice from the femoral vein. Until recently, collection of tissue and organ samples at various different time points seemed to be impossible without opening of the body. To the best of our knowledge, there is no literature on postmortem biopsy sampling for toxicological analysis. The Virtobot system should finally allow collecting biopsy samples in postmortem cases under CT control. Thus, the actual collection site is known without opening of the corpse. This procedure should enable accurate placement of introducer needles into specific areas of a human body based on the CT image coordinate system. Accuracy of the needle placement was tested exemplarily in two cases. All CT-guided introducer needle placements were executed successfully by the robotic arm. The mean absolute distance between the planned and effective target points of all introducer needles was 6.5 mm (range 1.7–9.6 mm, SD ± 2.2 mm). The component of the placement accuracy orthogonal to the planned needle location averaged at 6.2 mm (range 1.1–12.5 mm, SD ± 2.4 mm), longitudinal to the planned location at 1.8 mm (range 0.1–7.7 mm, SD ± 2.1 mm). Solid tissue samples with a diameter of approx. 2 mm and a length ranging from 10 to 20 mm as well as 1 mL of fluid each from the heart, the femoral vein, and the dural sac of the spine were successfully obtained. For all tissue biopsies, the complete biopsy needle length of 22 mm was located inside the target organs except for the kidney in case 1, where 87 % of the throw length was located inside the kidney and 13 % in the perirenal fat. These results indicate that each biopsy should be checked visually for homogeneity before processing. The deviation between planned and effective needle positions might have been caused by shifting of organs or needle bending during introduction of the needles into the body. A faster introduction velocity or needles with thinner diameter might reduce organ movement during needle introduction. However, needles with thinner diameter might worsen the needle bending. Needles which were located close to the body surface might have shifted because their balance point was located outside the body. This phenomenon was observed for the needle placed in the femoral vein in one of the cases. However, placement bias of less than 10 mm was acceptable for the study purpose. Of course, biopsies can also be collected manually, without a robotic arm. However, manual placement would probably be less accurate and more time consuming, as after placement, the CT room would have to be abandoned for control scans repeatedly. At autopsy, samples were collected from the same regions as at t1. After opening of the body, entry marks of the introducer needles were visible on the organ or tissue surfaces and could together with the CT information be used as guidance for the second sampling. Heart blood was collected with a syringe from the right heart chamber before removal of the heart. In conclusion, the automated biopsy sampling technique should be sufficiently accurate and can be used for postmortem sampling at two times points without opening of the body. This is important, as after opening of the body, redistribution processes might be altered and not reliable anymore. Therefore, the application of biopsy sampling is a major advantage for PMR investigations in alternative matrices.
Analyte distribution within sampling target area
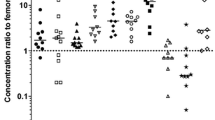
The ideal approach to investigate PMR would be to analyze the same sample at several time points. Due to practical reasons, the same sample can only be analyzed once, and therefore, the second sample has to be collected as near as possible to the first one. Inhomogeneous distribution of a drug might lead to different concentrations in these samples which are not time-dependent and makes it more difficult to detect effective concentration changes. The distribution of drugs within different regions of greater distance within an organ or tissue has already been shown to be inhomogeneous in previous studies, where samples of 5.0 g were collected from different locations in liver and lung. Redistribution processes from adjacent organs or tissues are believed to be responsible for these concentration differences [5, 28]. However, in our study, samples are compared within a much smaller organ area, where no data about the distribution of drugs is available so far. To investigate the distribution in our sample target area, five samples from liver and kidney were collected at once within a 2 × 2 × 1 cm area in four cases. This area approximately corresponds to the area where samples are taken at both time points (t1 and t2). Measured concentrations (relatively shown to the mean of n = 5 determinations set to 100 %) of different drugs in liver samples of three individual cases are exemplarily shown in Fig. 2. In case A, all analytes seemed to be distributed rather inhomogeneously with RSD from 35 to 65 %. In cases B and C, all analytes showed RSD below 10 % except for EDDP, which had an RSD of 40 %. Diazepam and nordazepam showing large deviations in case A gave good results in case B. In the fourth case, all analytes showed comparable RSD of approx. 20–30 %. In kidney, the RSD of the analyte concentrations were higher compared to liver in all four cases. They differed from case to case and from analyte to analyte, ranging from 10 to 45 %. These results indicate that analytes can be distributed very inhomogeneously with inter-individual differences. Different reasons may be responsible for the inhomogeneity such as different anatomical substructures in liver (e.g., blood vessels, bile ducts, or adipose regions) or differences between the medulla and cortex of the kidney. Unfortunately, these substructures cannot be differentiated during biopsy sampling. Furthermore, the shown variations should represent a combination of sampling and also analytical imprecision. Although the validated LC-MS/MS method showed acceptable results with intra-day precision data below 20 % for the majority of the analytes, it still can contribute to the observed variations. To take these variations into account and to avoid concentration changes falsely attributed to time difference, triplicate samples should be taken and analyzed for the final study. Triplicate measurements represent the compromise between indication for inhomogeneity and feasibility in routine analysis already leading to up to 78 samples for one case.
Drug distribution and variation within a region of 2 × 2 × 1 cm in liver tissue from three cases. Data points represent individual measurements of n = 5 determinations given relatively to the mean of the drug set to 100 %. Dotted lines indicate variation of ±20 %. EDDP 2-ethylidene-1,5-dimethyl-3,3-diphenylpyrrolidine, ODMV O-desmethylvenlafaxine, BEC benzoylecgonine, MDMA, 3,4-methylenedioxymethamphetamine
Applicability and proof of concept
The newly developed sampling strategy together with the recently published analytical method [26] should provide acceptable variation both from sampling as shown above and also from the analytical side for the majority of the analytes, thus enabling detection of relevant time-dependent concentration changes postmortem. Those with large sampling variations and/or precision values outside the acceptance criteria of ±20 % need to be interpreted with even more care, if possible at all. As a proof of concept, the described method was applied to two authentic cases.
Case 1
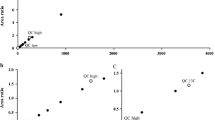
Case 1 was a 61-year-old woman who died after food aspiration. Time between death and first sampling was 15 h and further 22 h until the second sampling. At t1, all matrices were collected in supine position except for kidney, spleen, and CSF. CT control scans of the placed introducer needles are given in Fig. 3. The initial screening in HB showed the presence of venlafaxine, its pharmacologically active metabolite O-desmethylvenlafaxine (ODMV), and bromazepam. The analyte concentrations differed between the matrices, and the distribution pattern was analyte-dependent as displayed in Fig. 4. C/P and liver to peripheral blood (L/P) ratios at t1 of all analytes are given in Table 1. Comparison of the mean concentrations at time points 1 and 2 showed concentration increases and decreases depending on analyte and matrix.
Concentration of (a) venlafaxine, (b) ODMV, and (c) bromazepam in case 1 at t1 in green and t2 in blue (upper panels). Error bars indicate the concentration range. Lower panels show the mean percent concentration changes between the two time points. Gray bars indicate overlapping concentration ranges between t1 and t2
Venlafaxine concentrations at t1 were lowest in CSF and highest in spleen. C/P and L/P ratios were in the same range as reported in previous cases [8, 29]. Mean increases in concentration ranged between 20 and 30 % in pB, HB, CSF, and muscle. In kidney, an increase of 40 % and in lung, AT, and spleen, a decrease of 20–60 % was observed. As the given intra-day precision of venlafaxine was less than 10 % in all matrices [26] and variation of triplicate measurements were in the range of ±15 % of the mean, the observed concentration changes can be considered as redistribution processes and should not be caused by methodological imprecision. In liver tissue, ranges for triplicate measurements at t1 ranged from −60 to +30 % of the mean and ranges between t1 and t2 were overlapping. Although mean concentrations seemed to increase by 20 % from t1 to t2, this cannot reliably be classified as a time-dependent PMR effect. The concentration increase in pB matches expectations of 20–50 %, which were similarly observed by Gerostamoulos et al. [11].
ODMV concentration was lowest in AT and highest in lung (6.5 times higher than in pB). C/P and L/P ratios were in the same range as observed by Rodda et al. [29]. ODMV did not show any concentration changes >10 % in all body fluids or muscle tissue. In liver, AT, and spleen, a mean concentration increase of 30–50 % was observed. However, concentration ranges measured at t1 and t2 were clearly overlapping in most matrices, so that mean concentration changes are likely to be rather random. These high concentration ranges may have been caused by analytical imprecision, which was up to 30 % in the solid matrices as shown during the method validation process [26]. Only in lung tissue a decrease of 50 % with acceptable—not overlapping concentration ranges between t1 and t2 were observed that actually could be a time-dependent PMR.
Bromazepam showed highest concentration in liver and lowest in CSF, although the distribution between the matrices was rather homogeneous compared to the other analytes. The C/P ratio was in the same range as described by Dalpe et al. [30] but higher than reported by Pos Pok et al. [31]. Bromazepam did not show any concentration changes above 10 % except for a 30 % decrease in HB and a 30 % increase in AT. However, concentration ranges in HB and AT between t1 and t2 were overlapping and most likely by chance.
The data for venlafaxine, ODMV, and bromazepam could support the current opinion that drugs with high lipophilicity or Vd such as venlafaxine are more likely susceptible to PMR than drugs with lower LogP or Vd like ODMV and bromazepam (Table 1) [1].
Case 2
Case 2 was a 50-year-old woman who took several drugs deliberately to commit suicide. At t1, all matrices were collected in supine position except for kidney. Spleen was not available and aspiration of CSF was not successful, although the CT control scan indicated correct position of the needle. The initial LC-MS/MS screening in HB showed the presence of flupentixol, lorazepam, and paroxetine. The time between death and first sampling was 12 h and further 21 h until the second sampling which is similar to case 1. Again, drug concentrations differed between the matrices and the distribution patterns were drug-dependent as already shown above and depicted in Fig. 5. C/P and L/P ratios at time point 1 are given in Table 1. Comparison of the mean concentrations at time points 1 and 2 showed concentration increases and decreases depending on analyte and matrix.
Concentration of (a) flupentixol, (b) paroxetine, and (c) lorazepam in case 2 at t1 in green and t2 in blue (upper panels). Error bars indicate the concentration range. Lower panels show the mean percent concentration changes between the two time points. Gray bars indicate overlapping concentration ranges between t1 and t2
Flupentixol concentration at t1 was highest in lung (70 times higher than in pB), where the lowest concentrations were measured. A mean increase in concentration of 80 % in pB and a 50 % decrease in HB until t2 was observed. However, it should be noted that rather high variation was observed in t2 concentrations in pB and t1 in HB. In muscle, concentrations were rather similar between the two time points considering that a difference of only 15 % may be explainable by methodological variation. In liver, kidney, and AT, an increase of 30–45 % and in lung, a decrease of 30 % was observed. PMR of flupentixol has not yet been described in the literature. Only zuclopentixol, a structurally related thioxanthene was described with a mean increase of 62 % in pB [10] which is similar to our data in pB.
Paroxetine occurred with lowest mean concentration in HB and highest in lung (45 times higher than in pB). A C/P ratio below 1 could not be observed in previous studies, but the L/P ratio was within the published ranges [25, 29]. Mean concentrations increased 45 % in pB and HB and 20–30 % in liver and kidney and decreased 15 % in muscle and AT, while no changes were observed in lung tissue. A study in rats observed similar results for blood also showing increased concentrations, while contrary results were obtained in lung tissue with decreasing levels in rat lung tissue [32].
Lorazepam showed lowest concentration in pB and highest in liver. Although it belongs to the same substance class as bromazepam in case 1, it was distributed more inhomogeneously between the matrices. However, logP and Vd of lorazepam are higher compared to bromazepam. Lorazepam decreased 15 % in pB, HB and lung and 20–40 % in muscle, liver, and kidney. An increase of 30 % was observed in AT.
The presented cases proved the general applicability of the new sampling strategy in detection of postmortem concentration changes coming to similar results as already published for those analytes and matrices where reference data had been available. Of course, more data will be necessary and should be collected in the future to gather more knowledge on the phenomenon of PMR. In general, statistical significance of the concentration differences between the two time points is of interest. However, although concentration differences were clearly observed in the two presented cases, the power of an unpaired nonparametric test with data sets of only three replicates per time point was too low. Application of a parametric test with higher power was ineligible, as Gaussian distribution of the analyte concentrations within the biopsy target area could not be assumed. The collection of more than three replicates per matrix and time points was not practicable due to the resulting high number of samples and a time consuming collection procedure. But, as already stated, findings of concentration changes in only one case would not allow general statements anyway as each case differs from another [10]. More cases will be necessary, allowing statistical analysis on concentration differences, e.g., through ANOVA analysis.
Limitations
PMR is believed to occur to a great extent in the early postmortem period. As samples can be collected at the earliest after admission of the body at the institute, it will be difficult to obtain data about the first few hours after death. Additionally, the time between first and second sampling is limited to a maximum of 3 days, as the sampling must take place during routine investigation, which does not allow longer time periods between admission and autopsy. Therefore, longer postmortem intervals cannot be investigated. Human studies with controlled postmortem intervals are not feasible also due to ethical reasons. Investigation of PMR in the first few hours after death could be investigated in animal experiments. However, data on PMR in animal models can only be transferred to humans in a limited way. Thus, human studies still are indispensable. However, there are two prerequisites to actually detect PMR in human samples: the drug of interest is distributed homogeneously in the sampling area and the precision of the analytical method is high. The presented method employing CT-guided biopsy and reliable LC-MS/MS analytics showed that relevant extents of PMR can actually be detected. Therefore, it will be used for further investigations on PMR in humans.
Conclusions
CT-guided collection of biopsies was shown to be a valuable strategy for systematic studies on time-dependent PMR. The presented data showed that not only blood can be affected by postmortem concentration changes but also organs and tissues, where relevant concentration increases as well as decreases were observed. However, as large inter-individual differences are known to occur, more data are needed before conclusions, interpretation, and predictions for time-dependent PMR in alternative matrices can be done. With the presented strategy, we now have the tools for more “systematic” human time-dependent PMR studies for the first time.
References
Pelissier-Alicot AL, Gaulier JM, Champsaur P, Marquet P. Mechanisms underlying postmortem redistribution of drugs: a review. J Anal Toxicol. 2003;27(8):533–44.
Skopp G. Postmortem toxicology. Forensic Sci Med Pathol. 2010;6(4):314–25.
Yarema MC, Becker CE. Key concepts in postmortem drug redistribution. Clintoxicol. 2005;43(4):235–41.
Prouty RW, Anderson WH. The forensic science implications of site and temporal influences on postmortem blood-drug concentrations. J Forensic Sci. 1990;35(2):243–70.
Pounder DJ, Adams E, Fuke C, Langford AM. Site to site variability of postmortem drug concentrations in liver and lung. J Forensic Sci. 1996;41(6):927–32.
Leikin JB, Watson WA. Post-mortem toxicology: what the dead can and cannot tell us. J ToxicolClin Toxicol. 2003;41(1):47–56.
Hilberg T, Rogde S, Morland J. Postmortem drug redistribution—human cases related to results in experimental animals. J Forensic Sci. 1999;44(1):3–9.
Han E, Kim E, Hong H, Jeong S, Kim J, In S, et al. Evaluation of postmortem redistribution phenomena for commonly encountered drugs. Forensic Sci Int. 2012;219(1–3):265–71.
Jones GR, Pounder DJ. Site dependence of drug concentrations in postmortem blood—a case study. J Anal Toxicol. 1987;11(5):186–90.
Saar E, Beyer J, Gerostamoulos D, Drummer OH. The time-dependant post-mortem redistribution of antipsychotic drugs. Forensic Sci Int. 2012;222(1–3):223–7.
Gerostamoulos D, Beyer J, Staikos V, Tayler P, Woodford N, Drummer OH. The effect of the postmortem interval on the redistribution of drugs: a comparison of mortuary admission and autopsy blood specimens. Forensic Sci Med Pathol. 2012;8(4):373–9.
Robertson MD, Drummer OH. Postmortem distribution and redistribution of nitrobenzodiazepines in man. J Forensic Sci. 1998;43(1):9–13.
Martin A, Pounder DJ. Post-mortem toxico-kinetics of trazodone. Forensic Sci Int. 1992;56(2):201–7.
Yonemitsu K, Pounder DJ. Postmortem changes in blood tranylcypromine concentration: competing redistribution and degradation effects. Forensic Sci Int. 1993;59(2):177–84.
Gerostamoulos D, Drummer OH. Postmortem redistribution of morphine and its metabolites. J Forensic Sci. 2000;45(4):843–5.
Hargrove VM, Molina DK. Peripheral postmortem redistribution of morphine. Am J Forensic Med Pathol. 2014;35(2):106–8.
Logan BK, Smirnow D, Gullberg RG. Lack of predictable site-dependent differences and time-dependent changes in postmortem concentrations of cocaine, benzoylecgonine, and cocaethylene in humans. J Anal Toxicol. 1997;21(1):23–31.
Logan BK, Smirnow D. Postmortem distribution and redistribution of morphine in man. J Forensic Sci. 1996;41(2):221–9.
Quatrehomme G, Bourret F, Liao Z, Ollier A. An experimental methodology for the study of postmortem changes in toxic concentrations of drugs, using secobarbital as an example. J Forensic Sci. 1994;39(5):1300–4.
Brunet B, Hauet T, Hebrard W, Papet Y, Mauco G, Mura P. Postmortem redistribution of THC in the pig. Int J Legal Med. 2010;124(6):543–9.
Butzbach DM. The influence of putrefaction and sample storage on post-mortem toxicology results. Forensic Sci Med Pathol. 2010;6(1):35–45.
Skopp G. Preanalytic aspects in postmortem toxicology. Forensic Sci Int. 2004;142(2–3):75–100.
Cantrell FL, Ogera P, Mallett P, McIntyre IM. Fatal oral methylphenidate intoxication with postmortem concentrations. J Forensic Sci. 2014;59(3):847–9.
Levine B, Phipps RJ, Naso C, Fahie K, Fowler D. Tissue distribution of newer anticonvulsant drugs in postmortem cases. J Anal Toxicol. 2010;34(8):506–9.
Vermeulen T. Distribution of paroxetine in three postmortem cases. J Anal Toxicol. 1998;22(6):541–4.
Staeheli SN, Poetzsch M, Kraemer T, Steuer AE. Development and validation of a dynamic range-extended LC-MS/MS multi-analyte method for 11 different postmortem matrices for redistribution studies applying solvent calibration and additional (13)C isotope monitoring. Anal Bioanal Chem. 2015;407(29):8681–712.
Ebert LC, Ptacek W, Breitbeck R, Furst M, Kronreif G, Martinez RM, et al. Virtobot 2.0: the future of automated surface documentation and CT-guided needle placement in forensic medicine. Forensic Sci Med Pathol. 2014;10(2):179–86.
Langford AM, Taylor KK, Pounder DJ. Drug concentration in selected skeletal muscles. J Forensic Sci. 1998;43(1):22–7.
Rodda KE, Drummer OH. The redistribution of selected psychiatric drugs in post-mortem cases. Forensic Sci Int. 2006;164(2–3):235–9.
Dalpe-Scott M, Degouffe M, Garbutt D, Drost M. A comparison of drug concentrations in postmortem cardiac and peripheral blood in 320 cases. Can Soc Forensic Sci J. 1995;28(2):113–21.
Pos Pok PR, Haddouche D, Mauras M, Kuhlmann E, Burle J, Salmon T, et al. Cardiac and peripheral blood similarities in the comparison of nordiazepam and bromazepam blood concentrations. J Anal Toxicol. 2008;32(9):782–6.
Kupiec TC, Allen LV, Basmadjian GP, Canfield DV, Chaturvedi AK, Blank CL, Parker D Post mortem redistribution of paroxetine using the rat as a model. Presented at The American Academy of Forensic Sciences annual meeting San Francisco, California, USA (1998).
Baselt RC Disposition of toxic drugs and chemicals in man. 8th ed (2008).
Documed Kompendium Documed AG. www.compendium.ch (2015) Accessed 21.08.2015.
Acknowledgments
The authors would like to thank PD Dr. Frank T. Peters for the helpful discussion on statistical problems.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval was obtained by the cantonal ethics committee of Zurich, Switzerland (approval number 42.2005).
Conflicts of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Staeheli, S.N., Gascho, D., Fornaro, J. et al. Development of CT-guided biopsy sampling for time-dependent postmortem redistribution investigations in blood and alternative matrices—proof of concept and application on two cases. Anal Bioanal Chem 408, 1249–1258 (2016). https://doi.org/10.1007/s00216-015-9234-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00216-015-9234-9