Abstract
Purpose
Obstructive sleep apnea (OSA) is related to endothelin-1 (ET-1). Continuous positive airway pressure (CPAP) is an effective therapy for OSA. However, the effectiveness of CPAP on ET-1 levels in patients with OSA yielded contradictory results. We conducted a meta-analysis to assess the effect of CPAP on ET-1 levels in OSA.
Methods
The Embase, and Cochrane Library and PubMed were searched before March, 2018. The overall effects were measured by the standardized mean difference (SMD) with a 95% confidence interval (CI). Ten studies were included and the meta-analysis was conducted using Stata 14.0.
Results
10 studies involving 375 patients were included in the meta-analysis. The result showed that there was a significant reduction in ET-1 levels in OSA patients before and after CPAP therapy (SMD = − 0.74, 95% CI = − 1.30 to − 0.17, z = 2.56, p = 0.01). Further, subgroup analysis demonstrated that Apnea–Hypopnea Index (AHI), CPAP therapy duration, and sample size also affected CPAP therapy.
Conclusions
Our meta-analysis indicated that CPAP treatment among OSA patients was significantly was related to a decrease in ET-1 levels. Further prospective long-term studies with a larger number of patients are needed to evaluate and clarify this issue.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA), which can result in recurrent apneas and hypopneas during sleep, is the most common medical disease that characterized by upper airway obstruction and intermittent hypoxia [1]. It is associated mainly with affected cognitive function and daytime somnolence. Epidemiologic studies estimated that moderate-to-severe sleep-disordered breathing affects about 23.4% of females and 49.7% of males [2]. There has, for a long time, been a recognized link between OSA and cardiovascular diseases [3], including hypertension [4], and cardiovascular endothelial dysfunction [5].
Endothelin-1(ET-1) is a 21-amino acid powerful vasoconstrictor involved in the regulation of blood pressure, tissue perfusion and endothelial function [6]. Previous studies demonstrated that ET-1 can lead to cardiovascular risk and endothelial dysfunction because of the imbalance between vasodilator and vasoconstrictor endothelial mediators with overproduction of ET-1 [7]. Additionally, several studies on ET-1 circulation across OSA patients have reported significantly increased plasma levels [8,9,10]. Therefore, we hypothesized that elevated ET-1 levels could partly explain endothelial dysfunction in OSA patients.
Continuous positive airway pressure (CPAP) is considered as the first-line therapy for OSA, which is effective in decreasing inflammation and oxidative stress [11]. Evidence indicated that treatment of OSA patients with CPAP can significantly improve endothelial function [12], including flow-mediated dilation(FMD), venous occlusion plethysmography (VOP), nitric oxide(NO). However, whether ET-1 served as biomarkers of vascular function may be corrected or not by CPAP is unclear. Therefore, the meta-analysis in this paper is performed to quantitatively assess the effect of CPAP treatment on ET-1 among OSA patients.
Method
PRISMA Statement
This meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses(PRISMA) guidelines [13].
Literature search
We comprehensively searched Embase, Cochrane Library, and Pubmed for relevant studies published up to March 2018. Search terms included (obstructive sleep apnea OR ‘sleep apnea’ OR ‘sleep apnoea’ OR ‘apnea’) AND (‘endothelin-1’ OR ‘endothelin’ OR ‘ET-1’) AND (‘continuous positive airway pressure’ OR ‘cpap’ OR ‘ncpap’). The computerized search was complemented with a manual review of article bibliographies. In addition, we manually searched for review articles and relevant published studies.
Inclusion and exclusion criteria of the literature
The studies that met the following inclusion and exclusion criteria were selected: (1) all subjects in the study were adults(age ≥ 18) who were polysomnographically diagnosed with OSA based on the value of Apnea–Hypopnea Index (AHI) ≥ 5 events/h. (2) Using CPAP as an intervention. (3) The article must both have before and after CPAP ET-1 data reported. (4) Observational studies or randomized control trials; (5) The studies contained sufficient data to carry out a meta-analysis. (6) Abstracts, case reports, letters to the editor, reviews, non-English studies, and animal studies were excluded.
Data extraction
Two investigators independently assessed the eligible studies. Inconsistent decisions were solved through a consensus with a third investigator. The following variables were extracted from each article: name of first author, published year, nation of article, the number of patients, the number of males, mean age of patients, follow-up time of CPAP, mean daily duration, Apnea–Hypopnea Index (AHI), Body Mass Index (BMI), ET-1 measurement assays, study design, blood pressure, ET-1 level before and after CPAP therapy and lowest arterial oxygen saturation (LowSa\({{\text{O}}_2}\)).
Statistical analysis
All analyses were conducted using Stata version 14.0. Standardized mean difference (SMD) was performed for analysing the summary estimates, considering the outcome of ET-1 varied widely in some studies. Using the Chi square test determined statistical heterogeneity among individual studies. Heterogeneity amongst studies was assessed with the \({I^2}\) statistics(low: 25%, moderate: 50%, and high: 75%). Substantial heterogeneity was indicated by p < 0.10. If there was statistical heterogeneity among articles, a randomized-effects model was conducted. Otherwise, using a fixed-effects model estimated the pooled effects. Furthermore, we performed the subgroup analysis of CPAP treatment time (< 3 months, and ≥ 3 months), age of patients (< 50 year, and ≥ 50 year), AHI (< 30 events/h, and ≥ 30 events/h), body mass index (BMI < 30 kg/m2, and ≥ 30 kg/m2), sample size (< 20 and ≥ 20), method of detection (RIA and ELISA) to identify the possible sources of heterogeneity. Sensitivity analysis was conducted to assess the influence of the analysis results. Potential publication bias was shown by constructing funnel plot, using “Begg test” and “Egger test”. A value of p < 0.05 was considered as statistical significance.
Results
Characteristics of included studies
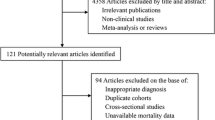
The detailed description of the steps of the article search was shown in Fig. 1. We initially identified 59 relevant articles; After reviewing the titles and abstracts, 43 articles were excluded because they were either reviews (n = 28), animal experiment (n = 1), conference abstract (n = 6), non-English articles (n = 6) or article from books (n = 2). 16 full texts were selected and further reviewed, among them, six articles were excluded for the following reasons: 1 lack of based data of AHI, 3 lack of before and after CPAP ET-1values; 2 do not study about the effect of CPAP on ET-1. Consequently, 10 studies involved 375 patients were included in the article. One study was randomized clinical trial (RCT), others were self-control trials (SCT). Information about the ten included articles showed the basic characteristics of the patients in Tables 1 and 2.
Pooled analysis
The test for heterogeneity showed that there were considerable differences across the studies [chi-squared = 98.40 (df = 9), p < 0.001; \({I^2}\) = 90.9%]. Therefore, meta-analysis conducted using a random effects model. The result indicated that there was a significant decrease in ET-1 in OSA patients before and after CPAP therapy (SMD = − 0.74, 95% CI = − 1.30 to − 0.17, z = 2.56, p = 0.01) (Fig. 2).
Subgroup analysis and sensitive analysis
To explore factors which may lead to heterogeneity in the effectiveness of CPAP treatment, we performed subgroup analysis based on CPAP treatment time, age of patients, AHI, mean BMI, sample size, method of detection. Subgroup analysis showed that, in the severe OSA (AHI ≥ 30 events/h), elevated ET-1 was significantly decreased after CPAP therapy (SMD = − 0.87, 95% CI = − 1.472 to 0.257, z = 2.79, p = 0.005); meanwhile, subgroup analysis demonstrated that ET-1 was significantly decreased after CPAP therapy duration < 3 months (SMD = − 1.933, 95% CI = − 2.981 to 0.884, z = 3.61, p < 0.001). Subgroup analysis also indicated that OSA subjects in studies with a sample size greater than 20 had an decreased ET-1 levels (SMD = − 1.12, 95% CI = 1.982 to 0.259, z = 2.55, p = 0.011). While the differences in age, mean BMI, method of detection, hardly affect CPAP efficacy. The detailed information on results of the subgroup analyses was showed in Table 3. Furthermore, sensitivity analysis indicated that the overall results were materially unchanged after deleting any one of the studies. (Fig. 3).
Publication bias
The funnel plot revealed that there was a small publication bias (Fig. 4), however, Egger’s tests (p = 0.118) and Begg’s tests (p = 0.152) demonstrated there was no evidence to confirm publication bias in the study. Furthermore, the trim and fill method was performed to show that no article was needed to correct for funnel plot asymmetry.
Discussion
This systematic review and meta-analysis assessed the efficacy of CPAP on ET-1 in patients with OSA. A remarkable finding from our meta-analysis is that CPAP may be an effective intervention for the reduction of ET-1 in patients with OSA (SMD = − 0.74, 95% CI= − 1.30 to − 0.17, z = 2.56, p = 0.01). The results were further confirmed by subgroup analysis, and the results showed that CPAP was associated with a statistically significant decrease on ET-1 in severe OSA patients (AHI ≥ 30 events/h, SMD = − 0.87, 95% CI= − 1.472 to 0.257, z = 2.79, p = 0.005), patients with therapeutic duration less than 3 months(SMD = − 1.933, 95% CI= − 2.981 to 0.884, z = 3.61, p < 0.001) and OSA subjects in studies with a sample size greater than 20(SMD = − 1.12, 95% CI = 1.982 to 0.259, z = 2.55, p = 0.011).
The endothelium plays a significant impact in the regulation of vascular function by secreting a large number of bioactive substances that are involved in the regulation of vascular tone, cells grown, inflammation, and thrombosis, such as ET-1 and NO [21]. The association between OSA and endothelial dysfunction has been demonstrated by several studies [22, 23], and earlier studies have shown that CPAP treatment results in an elevated NO levels [24]. However, it should be pointed that the effectiveness of CPAP on ET-1 levels is controversial. Previous studies had shown that there was a significant reduction in ET-1 after CPAP treatment [8, 9], particularly in OSA patients. Similar results were showed in Zhang’s study [17], CPAP therapy could play an important role in reducing ET-1 and vascular endothelial dysfunction. Wu found that CPAP results in a reduction in ET-1 levels, which contributes to endothelial function recovery by improving respiratory events at night [10]. Nevertheless, some investigators provided opposite results. Zamarronc showed a significant upregulation of ET-1, as compared with controls, but no change in ET-1 after CPAP treatment [20]. In agreement with previous study, Grimpen showed CPAP treatment can mitigate nocturnal hypoxaemia and reduce noradrenaline levels, while not affecting ET-1 plasma levels [15]. In concordance with Moller’s report, improvement of the nocturnal hypoxemia by CPAP therapy decreases BP, but not ET-1 [16]. In present meta-analysis, the results showed that levels of ET-1 are significantly decreased in subjects with OSA before and after CPAP therapy. The discrepancy in results is most likely due to differences in the severity of OSA、CPAP duration、 sample size and the measurement of ET-1. Therefore, we conducted subgroup analysis to identify the possible reason might contribute to the conflicting results.
ET-1 has been considered as an important cause in the development of cardiovascular risk and endothelial dysfunction [25]. Most studies reported higher ET-1 levels among OSA patients, especially in severe OSA patients. Previous study showed OSA patients had a higher ET-1 and a higher BP, and the mean nocturnal level of ET correlated significantly to the AHI [26]. Current studies reported that the degree to ET-1 affected was associated with the severity of the patients’ condition. Similarly, our subgroup analysis showed that elevated ET-1 was significantly decreased after CPAP therapy in the severe OSA [27]. The reason that may help explain the result could be that these severe patients have physiological abnormalities with more severe nocturnal hypoxemia, such as vascular endothelial dysfunction and inflammation [28].
However, the exact mechanism on the link between OSA and endothelial dysfunction was not fully understood. It is well known that OSA is the most common medical disease that characterized by intermittent hypoxia, which is related to increased reactive oxygen species (ROS) and oxidative stress response [29]. Some studies reported that intermittent hypoxia and increased production of ROS may accelerate endothelial injury [30]. In addition, excessive oxidative stress could reduce the activity of NO and accelerate endothelial dysfunction [31]. Moreover, in animal studies, Briancon reported that intermittent hypoxia exposure increases cardiac ET-1 and enhances myocardical sensitivity in rats [32]. Similarly, Wang demonstrated higher expression of ET-1 and ETA receptor in coronary vessels after intermittent hypoxia exposure, whereas expression of ETB receptor was decrease [33]. Therefore, we reasoned that intermittent hypoxia in OSA patients might promote endothelial dysfunction and it is closely related to ET-1.
As we all know, CPAP has been considered as the most common treatment for OSA patients, which can significantly improve OSA associated hypoxia condition and oxidative stress [11], as well as significantly improve endothelial dysfunction by reducing oxidative and inflammatory activities and improving endothelial capacity for repair [34]. Consistently, our present analysis showed that CPAP therapy could decrease the ET-1 level, especially in OSA patients with less than 3 months of CPAP duration. The results may be associated with CPAP treatment adherence of those patients [35]. In the studies of Baratta, adherence to CPAP was positively related to severity of OSA and negatively related to cigarette smoking and previous cardiac events [36]. It has been shown that better CPAP adherence was significantly related to a greater decrease in OSA patients with inattention [37]. Nevertheless, we are unable to determine if those patients have a greater adherence to treatment.
To our best knowledge, this meta-analysis is the first study investigating the effects of CPAP therapy on ET-1 in patients with OSA. However, there are some limitations to this study. First, most of the studies included were just observation studies and there was only one RCT, which may weaken the stringency of the study. Second, the heterogeneity test indicated that there were considerable differences among individual studies (chi-squared = 98.40 (df = 9), p < 0.001; \({I^2}\) = 90.9%), indicating that heterogeneity existed among the studies. Since there is difference existed in different countries and different study designs and it is impossible to carry out subgroup analysis eliminate such difference, inconsistent outcomes is obtained. Third, ET-1 was measured and mentioned differently, which might due to the short-life ET-1 whose activity is different measure [26]. Therefore, the results should be interpreted with caution. Finally, non-English studies were excluded, which may lead to potential publication bias.
Conclusions
In conclusion, our meta-analysis indicates that the CPAP therapy has a significant effect in reducing the ET-1 levels in OSA patients. However, the results need to be interpreted with caution due to a high heterogeneity. To further investigate whether CPAP can affect ET-1 in subjects with OSA, more long-term, large-scale interventional investigations are needed.
References
Strollo PJ, Rogers RM (1996) Obstructive sleep apnea. N Engl J Med 334(2):99–104. https://doi.org/10.1056/NEJM199601113340207
Heinzer R, Vat S, Marques-Vidal P, Marti-Soler H, Andries D, Tobback N, Mooser V, Preisig M, Malhotra A, Waeber G, Vollenweider P, Tafti M, Haba-Rubio J (2015) Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med 3(4):310–318. https://doi.org/10.1016/S2213-2600(15)00043-0
Drager LF, Togeiro SM, Polotsky VY, Lorenzi-Filho G (2013) Obstructive sleep apnea: a cardiometabolic risk in obesity and the metabolic syndrome. J Am Coll Cardiol 62(7):569–576. https://doi.org/10.1016/j.jacc.2013.05.045
Calhoun DA (2010) Obstructive sleep apnea and hypertension. Curr Hypertension Rep 12(3):189–195. https://doi.org/10.1007/s11906-010-0112-8
Shpilsky D, Erqou S, Patel S, Kip K, Ajala O, Aiyer A, Strollo P, Reis S, Olafiranye O (2018) Association of obstructive sleep apnea with microvascular endothelial dysfunction and subclinical coronary artery disease in a community-based population. Vasc Med. https://doi.org/10.1177/1358863X18755003
Olender J, Nowakowska-Zajdel E, Walkiewicz K, Muc-Wierzgon M (2016) Endothelins and carcinogenesis. Postepy Hig Med Dosw (Online) 70:872–880. https://doi.org/10.5604/17322693.1214386
Amiri F, Virdis A, Neves M, Iglarz M, Seidah N, Touyz R, Reudelhuber T, Schiffrin E (2004) Endothelium-restricted overexpression of human endothelin-1 causes vascular remodeling and endothelial dysfunction. Circulation 110(15):2233–2240. https://doi.org/10.1161/01.CIR.0000144462.08345.B9
Phillips BG, Narkiewicz K, Pesek CA, Haynes WG, Dyken ME, Somers VK (1999) Effects of obstructive sleep apnea on endothelin-1 and blood pressure. Journal of hypertension 17(1):61–66. https://doi.org/10.1097/00004872-199917010-00010
Liu J, Li Z, Liu Z, Zhu F, Li W, Jiang H, Wu X, Song Y, Li S, Bai C (2015) Exhaled nitric oxide from the central airway and alveoli in OSAHS patients: the potential correlations and clinical implications. Sleep Breath 20(1):145–154. https://doi.org/10.1007/s11325-015-1198-7
Wu K, Su X, Li G, Zhang N (2016) Antioxidant carbocysteine treatment in obstructive sleep apnea syndrome: a randomized clinical trial. PloS One 11(2):e0148519. https://doi.org/10.1371/journal.pone.0148519
Hoyos C, Melehan K, Liu P, Grunstein R, Phillips C (2015) Does obstructive sleep apnea cause endothelial dysfunction? A critical review of the literature. Sleep Med Rev 20:15–26. https://doi.org/10.1016/j.smrv.2014.06.003
Schwarz EI, Puhan MA, Schlatzer C, Stradling JR, Kohler M (2015) Effect of CPAP therapy on endothelial function in obstructive sleep apnoea: a systematic review and meta-analysis. Respirology 20(6):889–895. https://doi.org/10.1111/resp.12573
Moher D, Liberati A, Tetzlaff J, Altman D (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535. https://doi.org/10.1136/bmj.b2535
Saarelainen S, Seppala E, Laasonen K, Hasan J (1997) Circulating endothelin-1 in obstructive sleep apnea. Endothelium: J Endothelial Cell Res 5(2):115–118. https://doi.org/10.3109/10623329709079869
Grimpen F, Kanne P, Schulz E, Hagenah G, Hasenfuss G, Andreas S (2000) Endothelin-1 plasma levels are not elevated in patients with obstructive sleep apnoea. Eur Resp J 15(2):320–325. https://doi.org/10.1034/j.1399-3003.2000.15b17.x
Moller DS, Lind P, Strunge B, Pedersen EB (2003) Abnormal vasoactive hormones and 24-hour blood pressure in obstructive sleep apnea. Am J Hypertens 16(4):274–280. https://doi.org/10.1016/s0895-7061(02)03267-3
Zhang XL, Yin KS, Mao H, Wang H, Yang Y (2004) Effect of continuous positive airway pressure treatment on vascular endothelial function in patients with obstructive sleep apnea hypopnea syndrome and coronary artery disease. Chin Med J 117(6):844–847
Jordan W, Reinbacher A, Cohrs S, Grunewald RW, Mayer G, Ruther E, Rodenbeck A (2005) Obstructive sleep apnea: Plasma endothelin-1 precursor but not endothelin-1 levels are elevated and decline with nasal continuous positive airway pressure. Peptides 26(9):1654–1660. https://doi.org/10.1016/j.peptides.2005.02.012
Diefenbach K, Kretschmer K, Bauer S, Malzahn U, Penzel T, Roots I, Fietze I (2009) Endothelin-1 gene variant Lys198Asn and plasma endothelin level in obstructive sleep apnea. Cardiology 112(1):62–68. https://doi.org/10.1159/000137702
Zamarron C, Riveiro A, Gude F (2011) Circulating levels of vascular endothelial markers in obstructive sleep apnoea syndrome. Effects of nasal continuous positive airway pressure. Arch Med Sci: AMS 7(6):1023–1028. https://doi.org/10.5114/aoms.2011.26615
Sacerdoti D, Pesce P, Di Pascoli M, Brocco S, Cecchetto L, Bolognesi M (2015) Arachidonic acid metabolites and endothelial dysfunction of portal hypertension. Prostaglandins Other Lipid Mediat 120:80–90. https://doi.org/10.1016/j.prostaglandins.2015.05.008
Ip M, Tse H, Lam B, Tsang K, Lam W (2004) Endothelial function in obstructive sleep apnea and response to treatment. Am J Respir Crit Care Med 169(3):348–353. https://doi.org/10.1164/rccm.200306-767OC
Farooqui F, Sharma S, Kumar A, Soneja M, Mani K, Radhakrishnan R, Farooqui N (2017) Endothelial function and carotid intima media thickness in obstructive sleep apnea without comorbidity. Sleep Breath 21(1):69–76. https://doi.org/10.1007/s11325-016-1371-7
Alonso-Fernandez A, Garcia-Rio F, Arias MA, Hernanz A, de la Pena M, Pierola J, Barcelo A, Lopez-Collazo E, Agusti A (2009) Effects of CPAP on oxidative stress and nitrate efficiency in sleep apnoea: a randomised trial. Thorax 64(7):581–586. https://doi.org/10.1136/thx.2008.100537
Böhm F, Pernow J (2007) The importance of endothelin-1 for vascular dysfunction in cardiovascular disease. Cardiovasc Res 76(1):8–18. https://doi.org/10.1016/j.cardiores.2007.06.004
Gjorup PH, Sadauskiene L, Wessels J, Nyvad O, Strunge B, Pedersen EB (2007) Abnormally increased endothelin-1 in plasma during the night in obstructive sleep apnea: relation to blood pressure and severity of disease. Am J Hyper 20(1):44–52. https://doi.org/10.1016/j.amjhyper.2006.05.021
Jiang YQ, Xue JS, Xu J, Zhou ZX, Ji YL (2017) Efficacy of continuous positive airway pressure treatment in treating obstructive sleep apnea hypopnea syndrome associated with carotid arteriosclerosis. Exp Ther Med 14(6):6176–6182. https://doi.org/10.3892/etm.2017.5308
Shamsuzzaman AS, Gersh BJ, Somers VK (2003) Obstructive sleep apnea: implications for cardiac and vascular disease. JAMA 290(14):1906–1914. https://doi.org/10.1001/jama.290.14.1906
Budhiraja R, Tuder R, Hassoun P (2004) Endothelial dysfunction in pulmonary hypertension. Circulation 109(2):159–165. https://doi.org/10.1161/01.CIR.0000102381.57477.50
Lavie L, Lavie P (2009) Molecular mechanisms of cardiovascular disease in OSAHS: the oxidative stress link. Eur Respir J 33(6):1467–1484. https://doi.org/10.1183/09031936.00086608
Feng J, Zhang D, Chen B (2012) Endothelial mechanisms of endothelial dysfunction in patients with obstructive sleep apnea. Sleep Breath 16(2):283–294. https://doi.org/10.1007/s11325-011-0519-8
Briancon-Marjollet A, Monneret D, Henri M, Hazane-Puch F, Pepin JL, Faure P, Godin-Ribuot D (2016) Endothelin regulates intermittent hypoxia-induced lipolytic remodelling of adipose tissue and phosphorylation of hormone-sensitive lipase. J Physiol 594(6):1727–1740. https://doi.org/10.1113/JP271321
Wang JW, Li AY, Guo QH, Guo YJ, Weiss JW, Ji ES (2017) Endothelin-1 and ET receptors impair left ventricular function by mediated coronary arteries dysfunction in chronic intermittent hypoxia rats. Physiol Rep 5 (1). https://doi.org/10.14814/phy2.13050
Xu H, Wang Y, Guan J, Yi H, Yin S (2015) Effect of CPAP on endothelial function in subjects with obstructive sleep apnea: a meta-analysis. Respir Care 60(5):749–755. https://doi.org/10.4187/respcare.03739
Waradekar NV, Sinoway LI, Zwillich CW, Leuenberger UA (1996) Influence of treatment on muscle sympathetic nerve activity in sleep apnea. Am J Respir Crit Care Med 153(4 Pt 1):1333. https://doi.org/10.1164/ajrccm.153.4.8616563
Baratta F, Pastori D, Bucci T, Fabiani M, Fabiani V, Brunori M, Loffredo L, Lillo R, Pannitteri G, Angelico F, Del Ben M (2018) Long-term prediction of adherence to continuous positive air pressure therapy for the treatment of moderate/severe obstructive sleep apnea syndrome. Sleep Med 43:66–70. https://doi.org/10.1016/j.sleep.2017.09.032
Deering S, Liu L, Zamora T, Hamilton J, Stepnowsky C (2017) CPAP adherence is associated with attentional improvements in a group of primarily male patients with moderate to severe OSA. J Clin Sleep Med 13(12):1423–1428. https://doi.org/10.5664/jcsm.6838
Funding
This work was supported by Grant 81370182 from the Chinese National Natural Science Foundation. The sponsor had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Contributions
All authors directly participated in the study and have reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Rights and permissions
About this article
Cite this article
Lin, G., Chen, Q., Huang, J. et al. Effect of continuous positive airway pressure on endothelin-1 in patients with obstructive sleep apnea: a meta-analysis. Eur Arch Otorhinolaryngol 276, 623–630 (2019). https://doi.org/10.1007/s00405-018-5225-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-018-5225-8