Abstract
The aim of this review is to investigate whether changes in olfactory bulb volume relate to changes in specific olfactory functions. We studied currently available peer-reviewed articles on the volume of the human olfactory bulb that also included a psychophysical measure of olfactory function. In the present review, we observed a very clear and consistent correlation between general olfactory function and olfactory bulb (OB) volume. We were not able to find a clear relationship between a specific smell component and OB volume, even when analyzing pathologic conditions separately. In some cases, changes were observed for different subtests, but these changes did not significantly correlate with OB volume or had only a borderline correlation. In other cases, we found contradictory data. Several factors may contribute to the difficulties in finding correlations with the different components of smell: (1) the OB volume may be influenced by information from olfactory receptor neurons (bottom-up effect), information from central nervous system (top-down effect) and by direct damage; (2) most pathologic conditions affect more than one area of the olfactory pathway; (3) small sample sizes of hyposmic subjects were used. We believe that it is necessary to do further studies with larger numbers of subjects to answer the currently investigated question.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prevalence of olfactory dysfunction in the general population can be up to 20 % [1–3]. The most frequent causes of olfactory dysfunction are upper respiratory tract infection (URTI), inflammatory diseases of nose/paranasal sinuses, respiratory dysfunction, and trauma; often, however, a direct cause remains unknown [4, 5]. Frequency of each cause varies according to the population studied. Many studies have shown that there is a relationship between olfactory bulb (OB) volume assessed by MR imaging and olfactory function, in healthy subjects as well as in various pathological conditions [6–8].
Olfactory functions can be divided into at least three different components, namely, (1) perception of odors at the lowest possible concentration (odor threshold), (2) nonverbal distinction of different smells (odor discrimination), and (3) the ability to name or associate an odor (odor identification). Some psychophysical tests assessing olfactory performance include separate subtests for the assessment of each of these components [9] or some of them [10, 11], and others rely on one single component [12]. Previous work has shown that the three subtests tap into different olfactory functions [13, 14].
The aim of this short review is to evaluate whether changes in OB volume are related to a specific component of the sense of smell (threshold, identification, or discrimination).
It is tempting to separate olfactory loss into conductive and sensorineural dysfunction and relate conductive pathology to threshold changes, and sensorineural pathology to identification and discrimination. This should then differently impact in the OB. For example, according to the bottom-up hypothesis, meaning that OB volume is largely dependent on input from the olfactory epithelium [15], OB volume should be most strongly affected when the periphery is damaged. In contrast, assuming that higher central nervous system (CNS) structure determines OB volume [16], OB volume should be most affected in disorders presumably starting at the level of the CNS, e.g. Parkinson’s disease [17]. Fact is, that such differentiations are difficult to maintain, as OB volume seems to be affected in all groups of patients with different causes of olfactory loss.
Nevertheless, we tried to investigate whether OB volume reflects more odor thresholds or odor identification/discrimination.
Olfactory loss in chronic rhinosinusitis (CRS) is believed to be mainly conductive, although the OB could also be involved in the intranasal inflammatory process. In addition, the term “conductive” also does not cover the idea that in CRS inflammation alone produces a striking olfactory loss. However, provided that CRS affects the periphery of the nasal cavity to a higher degree than central-nervous structures, and that odor thresholds reflect peripheral functions to a higher degree than higher cognitive functions, then it can be hypothesized that OB volume changes in CRS are more strongly related to changes in odor threshold compared to changes in odor identification or odor discrimination.
In post-viral olfactory loss, the largest damage appears to be in the olfactory receptor neuron (ORN). Each ORN expresses one type of olfactory receptor (OR). Each “smell” is composed of various molecules, various odors. A certain combination of OR activation conforms an odor. Slight changes in the combination of OR activations may modify the perceived odorous impression [18]. Here, we would like to hypothesize that identification, threshold or both could be affected according to the extent or type of damage produced by viral infection.
In post-trauma olfactory loss, various structures can be affected namely axons of receptor neurons (shearing or “rupture”), OB, or cortex. Lesions of any of these structures could lead to a decrease in olfactory function and change in OB volume by a bottom-up effect, by a direct effect on the OB, or by a top-down effect of the CNS on the OB.
Materials and methods
We studied currently available peer-reviewed articles (until June 2014; English language; review based only on medline/pubmed as the most representative database in medical research) on the volume of the human olfactory bulb that also included a psychophysical measure of olfactory function, namely odor identification, odor discrimination, or odor threshold. We included 17 studies on patients (for a summary see Table 1) plus another three studies on healthy volunteers.
When describing the results, the term correlation will be used if a statistically significant correlation is present. If a correlation is not statistically significant, it will be specified.
Results
Changes in OB volume in patients are mainly related to odor identification and/or odor threshold—also because odor discrimination is rarely investigated. To better understand changes in patients, it is important to study these relationships in healthy subjects of different ages. In the following, results will be discussed for the various investigated groups—healthy subjects and patients with different causes of olfactory loss.
Healthy subjects
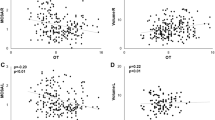
In healthy adults, Yousem et al. [19] observed peak olfactory function in the 3rd decade, followed by a plateau until the 7th decade, finally decreasing in the 7–8th decade. Olfactory bulb and tract (OBT) volume peaked in the 4th decade and decreased in the 7–8th decade paralleling olfactory function. Olfactory function was measured with the University of Pennsylvania Smell Identification Test (UPSIT [11]). Buschhüter et al. [6] also studied healthy adults (age range: 19–79 years) and observed that OB volume decreased with increasing age. Psychophysical testing was done with the Sniffin’ Sticks [9] comprising of three subtests for odor threshold (T), odor discrimination (D), and odor identification (I). OB volume correlated with overall olfactory function expressed in TDI score. Normative data were given for OB volume according to age and sex. Correlations with specific subtests did not produce a clear picture. When studying children and adolescents, Hummel et al. [7] observed that OB volume increased from age 1 to 17 years. Olfactory function was assessed in children 6-year-old and over, and an increase in overall olfactory function (expressed as TDI score) was observed from age 6 to 17 years. There was a clear correlation between specific olfactory functions (odor identification, odor discrimination, and odor threshold) and OB volume.
Patients
In patients with post-trauma olfactory loss, Yousem et al. [20] observed a decrease in OB volume and olfactory function, but no correlation between smell tests and OB volume. In a further study with a larger number of hyposmic patients, Yousem et al. [21] found that OB volume correlated with orthonasal odor identification whereas Rombaux et al. [22] observed a significant correlation between OB volume and odor threshold (T) and retronasal odor identification (RI). Orthonasal odor identification was greatly affected in the population studied by Rombaux et al. [16], but it exhibited no significant correlation with OB volume. There was also a relation between the degree of cortical damage and retronasal odor identification. Retronasal olfactory function was most compromised in patients in the frontotemporal group (damage to the frontal and anteroinferior temporal lobes) and least affected in patients without cortical lesions (the without group). Patients in the frontal group (with frontal lobe lesions) had measures of retronasal olfactory function that lay between the other two groups. A relationship between degree of cortical damage and OB volume was also observed. OB volumes were smallest in the fronto-temporal group, largest in patients without cortical damage, and medium sized in the frontal group.
When analyzing post-URTI (N = 22) and post-trauma (N = 9) patients, Mueller et al. [23] observed significant correlations between OB volumes and the TDI score expressing overall olfactory function. In addition, olfactory bulb volume was found to correlate significantly with each component of the sense of smell namely odor thresholds, odor discrimination, and odor identification. When controlling for the influence of age, partial correlations were still significant.
On the other hand, when analyzing post-URTI patients, Rombaux et al. [24] observed that OB volume correlated with identification, and not with threshold or discrimination. However, in a longitudinal study of patients with post-URTI and post-trauma olfactory loss, Haehner et al. [25] observed that in initially hyposmic patients, changes in OB volume correlated with changes in odor threshold.
Rombaux et al. [26], when evaluating patients with post-URTI and post-trauma olfactory loss, observed a correlation between baseline TDI score (overall olfactory function) and initial OB volume, as well as correlation between baseline retronasal odor identification and initial OB volume. Initial OB volume proved to be a useful prognostic tool, as larger initial OB volumes related to higher olfactory improvement. Changes in olfactory function were observed in all subtests (odor threshold, odor discrimination, and odor identification) as well as in retronasal odor identification.
Goektas et al. [27] studied 24 patients with post-URTI (N = 1), post-trauma (N = 5) and idiopathic (N = 9) olfactory loss. A significant correlation was found between electrophysiological measures of olfactory function (amplitudes of olfactory event-related potentials) and OB volume; but no correlation was identified for psychophysical olfactory evaluation (TDI score) and OB volume.
In patients with chronic rhinosinusitis, an increase in OB volume was observed after treatment, which correlated significantly with an increase in odor threshold [15].
In several studies, when comparing patients with and without parosmia, OB volume was smaller in patients with parosmia, without differing olfactory function [22–24].
Olfactory loss is also a common symptom of many neurological and psychiatric diseases. Various neurodegenerative diseases are believed to have olfactory dysfunction as an early symptom [28]. The affected areas and mechanisms differ from one to the other and, in some cases, are not clear.
In Parkinson’s disease (PD), in a recent study by Brodoehl et al. [29], a significant difference was observed in OB volume between PD patients and healthy controls. Left OB was significantly reduced in PD patients. They also demonstrated a significant correlation between olfactory function (composite TDI score) and OB volume in PD patients. Similar results were observed in a recent study by Chen et al. [30] who found significantly smaller OB volume in PD patients compared to controls. The grey matter of olfactory associated brain areas was also significantly reduced in PD patients. Olfactory function was not assessed. This is contrary to the results by Mueller et al. [17, 25] who reported no differences between the OB volumes of PD patients and controls. In this study, neither left-sided, nor right-sided, nor ‘‘best’’ OB volumes correlated significantly with overall olfactory function.
In Alzheimers disease, however, Thomann et al. [31, 32] observed reduced OB volume in patients compared to controls, and reduced OB volume in mild cognitive impairment compared with controls. Unfortunately olfactory function was not assessed.
When studying patients with Schizophrenia, Turetsky et al. [33] observed a 23 % reduction in OB volume in patients compared to healthy controls. In the control group, there was a strong association between OB volume and threshold; such association was not seen in the patient group. OB volume was unrelated to olfactory identification.
In a study comparing Schizophrenia patients, healthy first-degree family members and healthy controls, Turetsky et al. [34] observed reduced OB volume in patients and first-degree relatives. Olfactory threshold decreased only in patients. Olfactory identification did not decrease in patients and first-degree relatives. No correlation was observed between OB volume and olfactory function.
In a study on patients with temporal lobe epilepsy [16] patients were found to have reduced OB volume and reduced odor identification and odor threshold, compared to controls. OB volume correlated with odor identification, not with odor threshold.
Patients with idiopathic normal pressure hydrocephalous have lower olfactory function compared to healthy controls (p < 0.04). They also exhibited smaller OB volume (p < 0.02) [35].
When evaluating patients with acute major depression, a significant correlation was seen between the left OB and left threshold. Correlation between right OB volume and right threshold was not significant [36].
When evaluating patients treated for depression, comparing patients with a history of childhood maltreatment with patients without history of childhood maltreatment, Croy et al. [37] found significantly reduced odor thresholds and odor identification. OB volume was also significantly reduced in patients with history of childhood maltreatment. A trend was found for the correlation between the olfactory threshold and the left OB volume, but not for the right or the best OB volume. There was no significant correlation between the OB volume and olfactory discrimination or identification.
Smokers were seen to have olfactory function similar to non-smokers, but OB volume was significantly smaller in smokers [38]. Smoking could affect neurogenesis that occurs in the OB, this way reducing OB volume before affecting olfactory function.
Discussion
The OB is the first relay station in the olfactory pathway and is a highly plastic structure. Changes in OB volume occur in healthy subjects during their lifetime, with an increase during childhood and adolescence and a decrease towards 7 and 8th decade of life. Fluctuations in OB volume are related to changes in olfactory function.
OB volume is influenced by information from ORN (bottom-up effect) and by CNS structures (top-down effect). Direct damage to the OB can also affect its volume and function, for example in trauma, infections, and neurodegenerative diseases. Furthermore, factors such as stress and toxins are reflected in a reduced olfactory bulb volume, as was seen in acute major depression [36] and smokers [38]. The effect seems to be more pronounced if stress occurs in early childhood [38].
In the present review, we observed a very clear and consistent correlation between olfactory function and OB volume. A study comparing smokers to non-smokers was one notable exception [36], probably due to OB volume changes in smokers preceding changes in olfactory function.
We were not able to find a clear relationship between a specific smell component and OB volume, even when analyzing pathologic conditions separately. In some cases, changes were observed for different subtests, but these changes did not correlate with OB volume [38] or had only a borderline correlation [20, 33, 34, 38]. In other cases, we found contradictory data, for example in post-viral olfactory loss, Rombaux et al. [24] observed that change in OB volume correlated with a change in orthonasal odor identification while Haehner et al. [25] observed that OB volume change correlated with odor threshold. Other authors found that OB volume changes correlated with all the components of the sense of smell [23, 26]. In addition, in post-trauma olfactory loss, correlations between OB volume and specific components of the sense of smell were not clear.
These inconsistent results may be due to the type of olfactory test used, sample size, and age distribution which varied between these investigations. It may also be due to different MRI acquisition techniques used in different studies that might have contributed to inconsistencies of results. Further, several factors in olfactory processing may contribute to the difficulties in finding correlations with the different components of smell: (1) the OB is influenced by information from ORN (bottom-up effect), information from CNS (top-down effect) and by direct “affection” and (2) most pathologic conditions affect more than one area of the olfactory pathway; (3) small sample sizes of hyposmic subjects were used.
In conclusion, we believe that it is necessary to do further studies with larger numbers of subjects to answer the currently investigated question. Multicenter studies would be useful to reach meaningful numbers of participants.
References
Brämerson A, Johansson L, Ek L, Nordin S, Bende M (2004) Prevalence of olfactory dysfunction: the Skovde population-based study. Laryngoscope 114:733–737
Landis BN, Konnerth CG, Hummel T (2004) A study on the frequency of olfactory dysfunction. Laryngoscope 114:1764–1769
Soler GM, Nunez M (2012) The sense of smell in Buenos Aires population: a statistical study. Revista FASO N° 3
Temmel A, Quint C, Schikinger-Fisher B, Klimek L, Stoller E, Hummer T (2002) Characteristics of olfactory disorders in relation to major causes of olfactory loss. Arch Otolaryngol Head Neck Surg 128:635–641
Damm M, Temmel A, Welge-Lüssen A, Eckel HE, Kreft MP, Klussmann JP, Gudziol H, Hüttenbrink KB, Hummel T (2004) Epidemiologie und therapie von riechstörungen in Deutschland, Österreich und der schweiz. HNO 52:112–120
Buschhüter D, Smitka M, Puschmann S, Gerber JC, Witt M, Abolmaali ND, Hummel T (2008) Correlation between OB volume and olfactory function. Neuroimage 42:498–502
Hummel T, Smitka M, Puschmann S, Gerber JC, Schaal B, Buschhüter D (2011) Correlation between olfactory bulb volume and olfactory function in children and adolescents. Exp Brain Res 214:285–291. doi:10.1007/s00221-011-2832-7
Rombaux PH, Duprez T, Hummel T (2009) Olfactory bulb volume in clinical assessment of olfactory function. Rhinology 47:3–9
Hummel T, Sekinger B, Wolf SR, Pauli E, Kobal G (1997) Sniffin’ sticks’: olfactory performance assessed by the combined testing of odor identification, odor discrimination and olfactory threshold. Chem Senses 22:39–52
Cain W, Gent JF, Goodspeed RB, Leonard G (1988) Evaluation of olfactory dysfunction in the connecticut chemosensory clinical research center. Laryngoscope 98:83–88
Cain W, Rabin M (1989) Comparability of two tests of olfactory functioning. Chem Senses 14:479–485
Doty RL, Shaman P, Kimmelman CP, Dann MS (1984) University of Pennsylvania smell identification test: a rapid quantitative olfactory function test for the clinic. Laryngoscope 94:176–178
Hedner M, Larsson M, Arnold N, Zucco GM, Hummel T (2010) Cognitive factors in odor detection, odor discrimination, and odor identification tasks. J Clin Exp Neuropsychol 32:1062–1067
Lotsch J, Reichmann H, Hummel T (2008) Different odor tests contribute differently to the evaluation of olfactory loss. Chem 33:17–21
Gudziol V, Buschhüter D, Abolmaali N, Gerber J, Rombaux P, Hummel T (2009) Increasing olfactory bulb volume due to treatment of chronic rhinosinusitis—a longitudinal study. Brain 132:3096–3101
Hummel T, Henkel S, Negoias S, Galvan JR, Bogdanov V, Hopp P, Hallmeyer-Elgner S, Gerber J, Reuner U, Haehner A (2013) OB volume in temporal lobe epilepsy. J Neurol 260:1004–1008
Mueller A, Abolmaali ND, Hakimi AR, Gloeckler T, Herting B, Reichmann H, Hummel T (2005) Olfactory bulb volumes in patients with idiopathic Parkinson’s disease a pilot study. J Neural Transm 112:1363–1370
Malnic B, Hirono J, Takaaki S, Buck LB (1999) Combinatorial receptor codes for odors. Cell 96:713–723
Yousem DM, Gekle RJ, Bilker WB, Doty RL (1998) Olfactory bulb and tract and temporal lobe volume. Normative data across decades. Ann NY Acad Sci 855:546–555
Yousem DM, Gekle RJ, Bilker WB, McKeown DA, Doty RL (1996) Posttraumatic olfactory dysfunction: MR and clinical evaluation. Am J Neuroradiol 117:1171–1179
Yousem DM, Gekle RJ, Bilker WB, Kroger H, Doty RL (1999) Posttraumatic smell loss: relationship of psychophysical tests and volumes of the olfactory bulbs and tracts and the temporal lobes. Acad Radiol 6:264–272
Rombaux PH, Mouraux A, Bertrand B, Nicolas G, Duprez T, Hummel T (2006) Retronasal and orthonasal olfactory function in relation to olfactory bulb volume in patients with posttraumatic loss of smell. Laryngoscope 116:901–905
Mueller A, Rodewald A, Reden J, Gerber J, von Kummer R, Hummel T (2005) Reduced olfactory bulb volume in post-traumatic and post-infectious olfactory dysfunction. Chem Senses 16:475–478
Rombaux PH, Mouraux A, Bertrand B, Nicolas G, Duprez T, Hummel T (2006) Olfactory function and olfactory bulb volume in patients with postinfectious olfactory loss. Laryngoscope 116:436–439
Haehner A, Rodewald A, Gerber JC, Hummel T (2008) Correlation of olfactory function with changes in volume of the human olfactory bulb. Arch Otolaryngol Head Neck Surg 134:621–624
Rombaux PH, Huart C, Deggouj N, Duprez T, Hummel T (2012) Prognostic value of olfactory bulb volume for recovery in postinfectious and posttraumatic olfactory loss. Otolaryngol Head Neck Surg 147:1136–1141
Goektas O, Fleiner F, Sedlmaier B, Bauknecht C (2009) Correlation of olfactory dysfunction of different etiologies in MRI and comparison with subjective and objective olfactometry. Eur J Radiol 71:469–473
Hawkes C (2003) Olfaction in neurodegenerative disorders. Mov Disord 18:364–372
Brodoehl S, Klingner C, Volk GF, Bitter T, Witte OW, Redecker C (2012) Decreased olfactory bulb volume in idiopathic Parkinson’s disease detected by 3.0-tesla magnetic resonance imaging. Mov Disord 27:1019–1025
Chen S, Tan H-Y, Wu Z-H, Sun C-P, He J-X, Li X-C, Shao M (2013) The imaging study of olfactory bulb volume and grey matter volume of olfactory related brain areas in patients with Parkinson’s disease and multiple system atrophy. Radiol. doi:10.1016/j.ejrad.2013.11.024
Thomann PA, Dos Santos V, Toro P, Schonknecht P, Essig M, Schroder J (2009) Reduced olfactory bulb and olfactory tract volume in early Alzheimer’s disease—A MRI study. Neurobiol Aging 30:838–841
Thomann PA, Dos Santos V, Seidl U, Toro P, Essig M, Schroder J (2009) MRI-derived atrophy of the olfactory bulb and tract in mild cognitive impairment and Alzheimer’s disease. J Alzheimers Dis 17:213–221
Turetsky BI, Moberg PJ, Yousem DM, Doty RL, Arnold SE, Gur RE (2000) Reduced olfactory bulb volume in patients with Schizophrenia. Am J Psychiatry 157:828–830
Turetsky BI, Moberg PJ, Arnold SE, Doty RL, Gur RE (2003) Low olfactory bulb volume in first-degree relatives of patients with Schizophrenia. Am J Psychiatry 160:703–708
Podlesek D, Leimert M, Schuster B, Gerber J, Schackert G, Kirsh M, Hummel T (2012) Olfactory bulb volume in patients with idiopathic normal pressure hydrocephalus. Neuroradiology 54:1229–1233
Negoias S, Croy I, Gerber J, Puschmann S, Petrowski K, Joraschky P, Hummel T (2010) Reduced olfactory bulb volume and olfactory sensitivity in patients with acute major depression. Neuroscience 169:415–421
Croy I, Negoias S, Symmank A, Schellong J, Joraschky P, Hummel T (2013) Reduced olfactory bulb volume in adults with history of childhood maltreatment. Chem Senses 38:679–684
Schriever VA, Reither N, Gerber J, Ianilli E, Hummel T (2013) Olfactory bulb volume in smokers. Exp Brain Research 225:153–157
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mazal, P.P., Haehner, A. & Hummel, T. Relation of the volume of the olfactory bulb to psychophysical measures of olfactory function. Eur Arch Otorhinolaryngol 273, 1–7 (2016). https://doi.org/10.1007/s00405-014-3325-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-014-3325-7