Abstract
Introduction
Robotic systems have been introduced to improve the precision of total knee arthroplasty. However, different robotic systems are available, each with unique features used to plan and execute the surgery. As such, due to this diversity, the clinical evaluation of each robotic platform should be separated.
Methods
An extensive literature search of PubMed, Medline, Embase and Web of Science was conducted with subsequent meta-analysis. Randomised controlled trials, comparative studies, and cohort studies were included regarding robot-assisted total knee arthroplasty. Evaluated outcomes included clinical results, surgical precision, ligament balance, surgical time, learning curve, complications and revision rates. These were split up based on the robot-specific brand: ROBODOC (T-SOLUTION ONE), OMNIBOT, MAKO, NAVIO (CORI) and ROSA.
Results
With a follow-up of more than 10 years, no improved clinical outcomes have been noted with the ROBODOC system compared to the conventional technique. If available, other platforms only present short-term clinical outcomes. Radiological outcomes are published for most robotic setups, demonstrating improved surgical precision compared to the conventional technique. Gap balance assessment is performed differently between all systems, leading to heterogeneous outcomes regarding its relationship on clinical outcomes. There is a similar learning curve based on operative time for all robotic platforms. In most studies, robot assistance requires longer operative time compared to the conventional technique. Complications and revision rates are published for ROBODOC and MAKO, without clear differences to conventional total knee arthroplasty.
Conclusion
The main finding of this systematic review is that the current evidence regarding each robotic system is diverse in quantity and quality. Each system has its own specificities and must be assessed for its own value. Regarding scientific literature, the generic term of robotic should be banned from the general conclusion.
Level of evidence
Systematic review level IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The field of total knee arthroplasty (TKA) has been continuously evolving throughout the last decades. While the main idea of resurfacing has remained, multiple technical concepts and innovations have been the target of change [2, 12, 35, 47]. For instance, surgical navigation and patient-specific instruments were introduced to improve surgical precision compared to conventional instruments. However, due to lack of long-term clinical benefit, neither surgical navigation nor patient-specific instruments are systematically used today [2]. Recently, robots have been added to the surgeons’ arsenal to improve surgical precision even further. They provide the surgeon a real-time evaluation of the knee joint, while (semi-) actively aiding to perform the required bony cuts during TKA [51, 56, 61]. Although the first robot-assisted (RA) TKA has been performed in 1988 using the ACROBOT system, the current robotic platforms are not identical to what they were during initial development [17]. The introduction of the currently available robotic systems has led to an increase in RATKA. However, similarly to surgical navigation and patient-specific instruments, the question remains whether robotics will be used systematically in all cases in the long run. Of note is the increasing attention to data collection, which could be a thriving factor for using robotics, at least for scientific purposes [16]. The large amount of data collected during surgical workflow allows precise correlation with clinical outcomes.
In the last couple of years, major orthopaedic firms have jumped on the bandwagon and released their own version of a robotic platform to aid the orthopaedic surgeon during total knee surgery [3, 19, 30, 64, 66]. However, each system has a unique set of design characteristics, which cannot be overlooked. First, the reference frame and working volume are either based on an image-less or image-based philosophy. Next, all systems have a different type of motor control to restrict the surgeon in performing bony resections. Third, ligament tension assessment could be performed manually, sensor assisted or standardised during full range of motion. Finally, most robotic systems are dedicated to brand-specific implants, partially limiting the opportunity to compare between the different available robotic platforms.
As a result, the clinical evidence regarding RATKA cannot be grouped indiscriminately. Therefore, these systems should be assessed separately by peer review. This systematic review serves the goal of evaluating present literature for each individual robotic system currently available, related to patient-reported outcome measures, surgical precision, ligament balance, learning curve, complications and revision rates.
Materials and methods
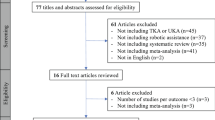
In December 2021, a search was performed in the electronical databases PubMed, Medline, Embase and Web of Science without date restriction. The reviewing process was completed independently by two authors (H.V. and C.B.). In case of disagreement, a third reviewer (S.L.) intervened to achieve consensus. The search strategy consisted the following terms: total knee replacement, total knee arthroplasty, robotics, robotic surgical procedure and robot-assisted. The reviewing process started with removal of all duplicates, after which all articles were evaluated for eligibility by title and abstract. Full-text articles were obtained for review to allow further assessment of inclusion and exclusion criteria. The reference lists of all relevant articles were reviewed to identify additional studies. This work was performed according to the PRISMA guidelines [29].
The inclusion criteria were defined as all English language studies evaluating clinical outcomes (patient-reported outcome measures and functional outcomes), surgical precision, gap balancing, learning curve, surgical time, complications and revision rates after RATKA. Randomised controlled trials, cohort studies and case–control studies were incorporated into the review process. The exclusion criteria were editorials, systematic reviews or meta-analyses, case reports, conference abstracts and the unavailability of full texts.
For both RATKA and conventional TKA, surgical precision was assessed as the difference between the intended implant position and the final position of the implant. The following variables were assessed regarding surgical precision: hip–knee–ankle axis (HKA), coronal femoral implant position, coronal tibial implant position, sagittal femoral implant position and sagittal tibial implant position. The methodology (radiography, computed tomography, intraoperative navigation) used to evaluate implant position was noted.
Data was collected using a predefined datasheet to behold the following study outcomes: clinical outcomes (patient-reported outcome measures and functional outcomes), surgical precision, learning curve, surgical time, complications and revision rates. The evidence was split up based on the robot used in the study: ROBODOC (T-SOLUTION ONE), OMNIBOT, MAKO, NAVIO (CORI) and ROSA (Table 1).
Quality assessment
The quality of the included studies and their relative risk of bias were evaluated with the ROBINS-I tool (Risk Of Bias In Non-Randomised Studies of Interventions) [58] (Table 2). The invested bias domains include bias due to confounding, selection of participants, classification of interventions, deviations from intended interventions, missing data, measurement of outcomes and selection of reported result. These domains were categorised based on the risk on bias being “low”, “moderate”, “serious” and “critical”. The worst judgement bias assigned within any one domain gives the judgement score of the complete study. All studies were screened for research funding or any conflict of interest to the orthopaedic company distributing the robotic system.
A meta-analysis was conducted using Review Manager 5.4 (Cochrane Collaboration, Oxford, UK) based on all studies comparing RATKA with conventional TKA. Heterogeneity among the studies was assessed using the χ2 test and I2. A fixed effect model was applied when I2 < 50%, and a random effects model when I2 > 50%. A p value < 0.05 was considered statistically significant.
Results
The PRISMA flow diagram can be seen in Fig. 1. After removal of duplicates, a total of 960 relevant references were found, and after screening, 92 full-text articles were assessed for eligibility. Further exclusion of 46 references and the addition of 2 articles by relevant references resulted in a total of 48 full-length articles [1, 3,4,5,6,7,8,9, 11, 13, 15, 18,19,20, 22, 24,25,26,27, 31,32,33, 36,37,38,39,40,41,42,43,44, 48, 49, 51, 52, 54,55,56, 58,59,60,61,62,63,64,65,66,67]. According to the ROBINS-I tool, 3, 41 and 4 studies were presented with low, moderate and serious risk of bias, respectively. In Appendix 1, an overview is given of all evidence for each system. In Appendix 2–6, each separate outcome is presented in detail.
ROBODOC/TSolution One
The ROBODOC system is the only system with long-term clinical follow-up. However, there was no short- or long-term (> 10 years) evidence illustrating better outcomes after total knee arthroplasty with ROBODOC compared to the conventional procedure. Of note, these studies were performed based on a principle of mechanical alignment. With respect to the radiological outcomes, there was no to some minor, although significant, improvement of surgical precision to achieve coronal and sagittal component alignment and hip–knee–ankle axis in case a robotic system was used [8, 18, 26, 33, 44, 55, 56, 67]. Based on the conducted meta-analysis, surgical precision was higher for ROBODOC compared to the conventional technique regarding HKA and tibial coronal and sagittal alignment (p = 0.02, 0.04 and 0.003 respectively, Fig. 2). Several studies have reported a lower proportion of outliers (> 3° coronal or sagittal malalignment compared to neutral mechanical alignment) in RATKA compared to the conventional procedure, but it was not correlated to improved clinical outcomes [8, 26, 33, 55, 56, 67]. Concerning gap balancing, there was one randomised controlled trial by Song and colleagues demonstrating a lower extent of gap imbalance (defined as a difference of > 2 mm between the extension and flexion gap) in case of RATKA compared to the conventional technique [56]. In this study, gap balance was obtained with a commercially available tensioner [56].
The forest plots of the meta-analysis performed regarding the studies comparing conventional with robot-assisted total knee arthroplasty with the ROBODOC system. A Surgical time. B Precision of hip–knee–ankle axis. C Precision of coronal femoral component position. D Precision of coronal tibial component position. E Precision of sagittal femoral component position. F Precision of sagittal tibial component position
According to Mahure et al. there was a learning curve of 10–12 cases based on the exact operative times [37]. The transition of a learning phase to proficiency phase could be seen after 12–19 cases, based on a CUSUM (cumulative summation) analysis. There was no impact of the learning curve on patient outcomes and operative complications. Overall surgical time, from incision to skin closure, was on average 23 min longer with ROBODOC compared to conventional TKA (p = 0.02; Fig. 2, Appendix 6). There was no difference in complications, long-term revision rates or long-term implant survival compared to the conventional technique. In total, 17% (2/12) of the included studies on the ROBODOC system demonstrated industry funding with a potential conflict of interest.
OMNIBOT
One study by Blum et al. compared the Knee Osteoarthritis Outcome Scores (KOOS) of a prospective RATKA cohort with the KOOS of the FORCE-TJR cohort, which is an accessible database of conventional total knee arthroplasty outcomes. No significant differences were seen between the two cohorts [5]. Based on the automated gap evaluation with the BalanceBot, a target for gap balance was defined as a difference of 1.5 mm between either extension/flexion or medial/lateral gap. In a prospective trial by Keggi and colleagues, comparing the OMNIBOT with and without predictive plan by the BalanceBot, the utilisation of predictive balancing led to a significant increase of 37% (88 vs 51%) in the amount of knees classified as balanced. All balanced knees demonstrated improved KOOS for subscore Pain at 3 months postoperatively, subscore Symptoms at all postoperative time points, subscore Activities of Daily Life at 6 months, and subscore Quality of Life at 3 months and 6 months compared to unbalanced knees (p < 0.05; without reaching the minimal clinical important difference) [24]. As such, specific targets for ligament balance with the BalanceBot have been published by Wakelin et al. which could improve PROMs: an equally balanced or tighter medial compartment in extension, medial laxity ± 1 mm compared to the final insert thickness in midflexion, and a medio-lateral imbalance of less than 1.5 mm in flexion [66]. One study was able to demonstrate minor significant superiority of the OMNIBOT system regarding surgical precision to achieve coronal tibial component position compared to patient-specific instruments, with an average difference of 0.5° between both (p = 0.02) [42]. There is no published data on the learning curve, surgical time and complication or revision rates. A conflict of interest or industry funding was found in 57% (4/7) of the included studies on the OMNIBOT system.
MAKO
The MAKO robot system was the most intensively researched out of all robotic systems for total knee surgery. There were some studies advocating improved clinical outcomes up to 1 year postoperatively compared to the conventional technique [22, 39,40,41, 52]. However, long-term clinical outcomes are still lacking. The surgical precision achieved with the system was higher compared to the conventional technique [19, 61], more specifically for HKA and tibial coronal alignment (p < 0.001 and p = 0.008 respectively, Fig. 3). Nevertheless, there was no demonstrated correlation between the accuracy of the bone resections and the improvement of clinical outcomes with this robotic system. There were two studies advocating improved ligament balance with sensor technology combined with the MAKO platform [7, 28]. To reach the transition from the learning phase to the proficiency phase, 7–43 cases should be completed [19, 54, 65]. Component alignment and gap balance were not influenced by a surgeon’s learning curve. Overall surgical time, from incision to skin closure, was not significantly different between RATKA and the conventional technique (p = 0.95, Fig. 3). After completing the learning curve setup time of the robot took 9.2 ± 1.5 min in the study by Kayani et al. [19]. In the included studies, there was no evidence for a difference in complications between robot-assisted and conventional TKA [22, 38, 41, 43, 52]. There was no long-term data available on revision rates. In half of the included studies (10/20) on the MAKO platform, there was a potential conflict of interest.
The Forest plots of the meta-analysis performed regarding the studies comparing conventional with robot-assisted total knee arthroplasty with the MAKO system. A Surgical time. B Precision of the hip–knee–ankle axis. C Precision of the coronal femoral component position. D Precision of the coronal tibial component position. E Precision of the sagittal femoral component position. F Precision of the sagittal tibial component position
NAVIO/CORI
Despite the promising results concerning the implant positioning and limb alignment, with superior precision to achieve the intended HKA (p < 0.001, Fig. 4), there was only one study, by Held et al., evaluating clinical outcomes without clear improvements when comparing conventional to RATKA [15]. According to Bell et al. and Savov et al. the learning curve encompasses the completion of 7–11 cases [3, 48]. Joint balance, when assessed with sensor technology, was improved with the application of the robotic system compared to the conventional technique [15]. Several studies have assessed surgical time, possibly demonstrating an increase in surgical time with the NAVIO robot compared to conventional TKA. There was no data available on the complications and revision rates. There was a potential conflict of interest or industry funding in 57% (4/7) of the included studies on the NAVIO/CORI system.
The forest plots of the meta-analysis performed regarding the studies comparing conventional with robot-assisted total knee arthroplasty with the NAVIO/CORI system. A Precision of the hip–knee–ankle axis. B Precision of the coronal femoral component position. C Precision of the coronal tibial component position
ROSA
There was no data available on clinical outcomes or possible complications. Compared to the intraoperative plan, the system obtained high surgical precision [64]. The learning curve regarding operative time would be completed after 6–11 performed cases with the system [64]. The operative time of the robotic procedure required on average 18 additional minutes compared to the conventional TKA [64]. There was a potential conflict of interest or research funding for the one study on the ROSA system included in this review.
Discussion
The primary aim of this systematic review was to give an overview of the capabilities of each robotic system for total knee arthroplasty and to identify gaps in currently available scientific literature. The main finding of this systematic review is the current evidence regarding each robotic system being diverse in quantity and quality, and consequently the generic term of robotic should be banned from general conclusion. For most systems, although not all, surgical precision was seen to be superior with robot assistance compared to conventional TKA. Long-term clinical benefit of any robot-assisted procedure is yet to be determined. However, some short-term clinical benefit has been reported compared to conventional TKA. When using a robot for TKA, surgical time is increased for most systems, albeit there is potential to reach identical surgical times of conventional TKA. There was no difference in the amount of complications between RATKA and conventional TKA. The most profound benefit of these robotic systems is the superior surgical precision compared to the conventional technique (Appendix 3) [6, 8, 11, 13, 18, 19, 26, 27, 31, 33, 36, 42, 44, 48, 50, 51, 55, 56, 59,60,61,62, 64, 67]. Most evidence is found in lower outlier rates, although fewer studies identifying direct superiority of implant positioning in the RATKA are available. For ROSA and VELYS, clinical studies identifying its validated surgical precision are still yet to be published. Interestingly, Kayani and colleagues identified better soft tissue protection while maintaining high precision during surgery, which might stress an additional benefit of stereotactic boundary control with the robot-assisted systems [20].
The literature on clinical outcomes with currently available robotic systems is not available for the ROSA and VELYS robotic systems and still limited for the other platforms. Up to date, there are no clear long-term clinical improvements after total knee surgery when comparing any robotic system to its conventional counterpart (Appendix 2). Unfortunately, patient-reported outcomes and functional outcomes were deemed to heterogeneously due to different time intervals per individual robot to perform a meaningful meta-analysis. There are some studies advocating early improved patient outcomes, although this trend did not continue after 6 months to 1 year postoperatively [15, 22, 32, 39,40,41, 52]. Of note, especially for ROBODOC, is that the clinical studies were mainly based on a principle of mechanical alignment. The superior precision of the robotic systems opens doors for more individualised alignment techniques, theoretically avoiding major limitations of surgical error (e.g., early failure with aseptic loosening or implant migration) with the conventional technique [12, 34, 46]. However, these individualised alignment strategies are in need of further refinement and proven clinical benefit before becoming the golden standard [47].
Besides good surgical precision, an additional added value of multiple robotic systems is the capability of assessing ligament tension. Currently, there are three options of assessing ligament tension. First, the laxity assessment with the robotic assisted system could be performed manually. The surgeon exerts a significant varus and valgus force on the knee, with or without tensioner. This assessment is dependent on the strength and evaluation of the surgeon, on the depth of anaesthesia, and the BMI or the physical stature of the patient. The ligament balancing is thus not entirely objective and dependent upon the surgeon’s experience of with the system. Second, with the MAKO platform, sensor-guided technology can objectify soft tissue balance with a wireless and disposable articular loading quantification device, which is inserted in the tibial component tray during the surgery, after the tibial and femoral cuts are completed [14]. Third, standardised distraction of the joint is possible with the BalanceBot, due to the option to apply variable or fixed, but known, forces during full range of motion [24, 66]. The BalanceBot requires a tibial first technique to insert the device, which limits the influence of tibial osteophytes on ligament balance. Studies on both the sensor and the standardised distraction device have shown promising results with superior clinical outcomes when specific balance targets are met [14, 15, 24, 28, 66]. However, due to heterogeneous assessment, comparing these systems is not possible. In the end, long-term randomised controlled studies are still necessary to confirm these findings.
The learning curve of most systems seems to be similar between all available robotic systems, except for the OMNIBOT and VELYS systems, which have not been assessed yet (Appendix 4) [3, 19, 37, 48, 54, 64, 65]. However, Keggi and Plaskos have published the learning curve of the OMNIBOT system in a conference abstract, which resulted in a learning curve of seven cases based on surgical time [23] At first sight though, there was a wider variation of the amount of cases necessary to complete the learning curve with the MAKO robot (7–43 cases) compared to other systems (6–12), possibly due to the fact that more studies have been published on the MAKO robot, possibly with the learning curve of a more diverse audience. The initial studies on a surgical system might involve surgeons involved in the robot design. As such, these might be biased towards faster learning curves. According to this systematic review, there was no clear difference in the learning curve between image-based and imageless devices, based on operative time and implant positioning. After completion of the learning curve, some studies have advocated the possibility to achieve time identical surgical times with RATKA compared to the conventional technique [54, 65]. These studies were performed by mostly high-volume and experienced joint replacement surgeons, which makes it difficult to apply to a low-volume or less experienced surgeon.
Literature on surgical complications is available for ROBODOC and MAKO. These studies on the ROBODOC and MAKO could not present any difference in complications between the conventional technique and RATKA (Appendix 5) [8, 33, 56, 67]. However, surgeons should remain cautious when using tracker pins, since periprosthetic fractures through tracking pin sites could occur in up to 5% of cases, as has been reported by Smith et al. [53]. Long-term revision rates are only available for ROBODOC system, which could not demonstrate any superiority of RATKA. However, these studies have been performed with a principle of mechanical alignment. Revision rates for the other systems are still to be published, as the time of commercial release lies within the past couple of years.
Surgical time is important as well in the consideration of robot-assisted versus conventional TKA. Although not present for the MAKO system in our meta-analysis, in almost all individual studies included in this review, the total knee arthroplasty required more time to complete when performed with robot-assistance (Appendix 6). Any increase of operative time and additional personnel in the operating room should be approached with caution, as it could potentially increase infection rates [57]. However, more than operative time, which is from skin incision to skin closure, should be considered. As an example, the time needed for set-up of the robotic systems has an influence on the capability to use operating time efficiently as well. Kayani et al. have found an average set-up time of 9.2 min was necessary for the MAKO platform [19]. While it is a large system yet easily moved, the set-up time necessary for other systems is still unknown.
In the included studies, a conflict of interest or research funding by the orthopaedic company was present in (more than) half of all cases, except for the ROBODOC system (17% of all studies). The reader of future studies on RATKA should be aware conflicts of interest are not scarce in this topic.
The available robotic systems, besides the VELYS system, all have demonstrated their technical capabilities in some degree. However, cost-effectiveness is a factor which cannot be ignored when assessing the introduction of robotic systems in current daily practice. As such, up to now, there is only limited evidence on the cost-effectiveness of the MAKO platform. According to Cool et al. and Pierce et al. RATKA was associated with lower health-related costs compared to the conventional technique due to fewer readmissions and economically beneficial discharge destinations [10, 45]. However, these studies did not take into account confounding variables which might be present based on the patient’s deliberate choice for robot-assisted surgery.
The limitations of this review relate to the level of available evidence and the inherent lack of homogenous high quality data, incomplete reporting of surgical experience. There is a paucity of trials and level 1 data regarding all systems available for RATKA. However, promising studies are underway [21]. As well, as only English language manuscripts were included together with the requirement of full text access, some relevant studies could have been excluded. Next, in the assessment of all included studies, the fact that these were performed by experienced surgeons working in high-volume arthroplasty centres should be highlighted, potentially introducing bias. It is unlikely that the conclusions of these studies can be extrapolated to less experienced and lower volume surgeons.
Conclusion
The current systematic review demonstrates there are certainly gaps in the current literature on robot-assisted total knee surgery. The available robotic platforms have high surgical precision and are associated with similar learning curves, without evidence of clear improved patient outcomes for most of them. However, as high patient satisfaction and patient function with a durable prosthesis remain the ultimate goal, the implementation of these precise systems and gap balancing opportunities could potentially unlock the door to improved patient outcomes. To provide solid scientific evidence of such improvement, the main recommendation is that each system must be assessed for its own value and the generic term of robotic should be banned from general conclusion.
References
Bardou-Jacquet J, Murgier J, Laudet F, Fabre T (2021) Combining load sensor and robotic technologies for ligament balance in total knee arthroplasty. Orthop Traumatol Surg Res 108:102889
Batailler C, Swan J, Sappey Marinier E, Servien E, Lustig S (2020) New technologies in knee arthroplasty: current concepts. J Clin Med 10:47
Bell C, Grau L, Orozco F, Ponzio D, Post Z, Czymek M, Ong A (2021) The successful implementation of the navio robotic technology required 29 cases. J Robot Surg 16:495–499
Bhimani SJ, Bhimani R, Smith A, Eccles C, Smith L, Malkani A (2020) Robotic-assisted total knee arthroplasty demonstrates decreased postoperative pain and opioid usage compared to conventional total knee arthroplasty. Bone Jt Open 1:8–12
Blum CL, Lepkowsky E, Hussein A, Wakelin EA, Plaskos C, Koenig JA (2021) Patient expectations and satisfaction in robotic-assisted total knee arthroplasty: a prospective two-year outcome study. Arch Orthop Trauma Surg 141:2155–2164
Bollars P, Boeckxstaens A, Mievis J, Kalaai S, Schotanus MGM, Janssen D (2020) Preliminary experience with an image-free handheld robot for total knee arthroplasty: 77 cases compared with a matched control group. Eur J Orthop Surg Traumatol 30:723–729
Chang JS, Kayani B, Wallace C, Haddad FS (2021) Functional alignment achieves soft-tissue balance in total knee arthroplasty as measured with quantitative sensor-guided technology. Bone Joint J 103-B:507–514
Cho K-J, Seon J-K, Jang W-Y, Park C-G, Song E-K (2019) Robotic versus conventional primary total knee arthroplasty: clinical and radiological long-term results with a minimum follow-up of ten years. Int Orthop 43:1345–1354
Clark TC, Schmidt FH (2013) Robot-assisted navigation versus computer-assisted navigation in primary total knee arthroplasty: efficiency and accuracy. ISRN Orthop 2013:794827
Cool CL, Jacofsky DJ, Seeger KA, Sodhi N, Mont MA (2019) A 90-day episode-of-care cost analysis of robotic-arm assisted total knee arthroplasty. J Comp Eff Res 8:327–336
Deckey DG, Rosenow CS, Verhey JT, Brinkman JC, Mayfield CK, Clarke HD, Bingham JS (2021) Robotic-assisted total knee arthroplasty improves accuracy and precision compared to conventional techniques. Bone Joint J 103-B:74–80
Fang DM, Ritter MA, Davis KE (2009) Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty 24:39–43
Figueroa F, Wakelin E, Twiggs J, Fritsch B (2019) Comparison between navigated reported position and postoperative computed tomography to evaluate accuracy in a robotic navigation system in total knee arthroplasty. Knee 26:869–875
Gordon AC, Conditt MA, Verstraete MA (2021) Achieving a balanced knee in robotic TKA. Sensors (Basel) 21:535
Held MB, Grosso MJ, Gazgalis A, Sarpong NO, Boddapati V, Neuwirth A, Geller JA (2021) Improved compartment balancing using a robot-assisted total knee arthroplasty. Arthroplast Today 7:130–134
Helm JM, Swiergosz AM, Haeberle HS, Karnuta JM, Schaffer JL, Krebs VE, Spitzer AI, Ramkumar PN (2020) Machine learning and artificial intelligence: definitions, applications, and future directions. Curr Rev Musculoskelet Med 13:69–76
Jakopec M, Harris SJ, Rodriguez y Baena F, Gomes P, Cobb J, Davies BL (2001) The first clinical application of a “hands-on” robotic knee surgery system. Comput Aided Surg 6:329–339
Jeon S-W, Kim K-I, Song SJ (2019) Robot-assisted total knee arthroplasty does not improve long-term clinical and radiologic outcomes. J Arthroplasty 34:1656–1661
Kayani B, Konan S, Huq SS, Tahmassebi J, Haddad FS (2019) Robotic-arm assisted total knee arthroplasty has a learning curve of seven cases for integration into the surgical workflow but no learning curve effect for accuracy of implant positioning. Knee Surg Sports Traumatol Arthrosc 27:1132–1141
Kayani B, Konan S, Pietrzak JRT, Haddad FS (2018) Iatrogenic bone and soft tissue trauma in robotic-arm assisted total knee arthroplasty compared with conventional jig-based total knee arthroplasty: a prospective cohort study and validation of a new classification system. J Arthroplasty 33:2496–2501
Kayani B, Konan S, Tahmassebi J, Oussedik S, Moriarty PD, Haddad FS (2020) A prospective double-blinded randomised control trial comparing robotic arm-assisted functionally aligned total knee arthroplasty versus robotic arm-assisted mechanically aligned total knee arthroplasty. Trials 21:194
Kayani B, Konan S, Tahmassebi J, Pietrzak JRT, Haddad FS (2018) Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty: a prospective cohort study. Bone Joint J 100-B:930–937
Keggi J, Plaskos C (2017) Learning curve and early patient satisfaction of robotic-assisted total knee arthroplasty. Br Editor Soc Bone Jt Surg 99:59
Keggi JM, Wakelin EA, Koenig JA, Lawrence JM, Randall AL, Ponder CE, DeClaire JH, Shalhoub S, Lyman S, Plaskos C (2021) Impact of intra-operative predictive ligament balance on post-operative balance and patient outcome in TKA: a prospective multicenter study. Arch Orthop Trauma Surg 141:2165–2174
Khlopas A, Sodhi N, Hozack WJ, Chen AF, Mahoney OM, Kinsey T, Orozco F, Mont MA (2020) Patient-reported functional and satisfaction outcomes after robotic-arm-assisted total knee arthroplasty: early results of a prospective multicenter investigation. J Knee Surg 33:685–690
Kim Y-H, Yoon S-H, Park J-W (2020) Does robotic-assisted TKA result in better outcome scores or long-term survivorship than conventional TKA? A randomized, controlled trial. Clin Orthop Relat Res 478:266–275
Laddha M, Gaurav S (2021) Assessment of limb alignment and component placement after all burr robotic-assisted TKA. Indian J Orthop 55:69–75
Lee G-C, Wakelin E, Randall A, Plaskos C (2021) Can a robot help a surgeon to predict a good total knee arthroplasty? Bone Joint J 103-B:67–73
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
Liow MHL, Chin PL, Pang HN, Tay DK-J, Yeo S-J (2017) THINK surgical TSolution-One® (Robodoc) total knee arthroplasty. Sicot-J 3:63
Liow MHL, Chin PL, Tay KJD, Chia SL, Lo NN, Yeo SJ (2014) Early experiences with robot-assisted total knee arthroplasty using the DigiMatch™ ROBODOC surgical system. Singapore Med J 55:529–534
Liow MHL, Goh GS-H, Wong MK, Chin PL, Tay DK-J, Yeo S-J (2017) Robotic-assisted total knee arthroplasty may lead to improvement in quality-of-life measures: a 2-year follow-up of a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc 25:2942–2951
Liow MHL, Xia Z, Wong MK, Tay KJ, Yeo SJ, Chin PL (2014) Robot-assisted total knee arthroplasty accurately restores the joint line and mechanical axis: a prospective randomised study. J Arthroplasty 29:2373–2377
Liu H-X, Shang P, Ying X-Z, Zhang Y (2016) Shorter survival rate in varus-aligned knees after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24:2663–2671
Lustig S, Sappey-Marinier E, Fary C, Servien E, Parratte S, Batailler C (2021) Personalized alignment in total knee arthroplasty: current concepts. SICOT-J 7:19
Mahoney O, Kinsey T, Sodhi N, Mont MA, Chen AF, Orozco F, Hozack W (2022) Improved component placement accuracy with robotic-arm assisted total knee arthroplasty. J Knee Surg 35:337–344
Mahure SA, Teo GM, Kissin YD, Stulberg BN, Kreuzer S, Long WJ (2021) Learning curve for active robotic total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 30:2666–2676
Malkani AL, Roche MW, Kolisek FR, Gustke KA, Hozack WJ, Sodhi N, Acuña A, Vakharia R, Salem HS, Jaggard C, Smith L, Mont MA (2020) New technology for total knee arthroplasty provides excellent patient-reported outcomes: a minimum two-year analysis. Surg Technol Int 36:276–280
Marchand RC, Sodhi N, Anis HK, Ehiorobo J, Newman JM, Taylor K, Condrey C, Hepinstall MS, Mont MA (2019) One-year patient outcomes for robotic-arm-assisted versus manual total knee arthroplasty. J Knee Surg 32:1063–1068
Marchand RC, Sodhi N, Khlopas A, Sultan AA, Harwin SF, Malkani AL, Mont MA (2017) Patient satisfaction outcomes after robotic arm-assisted total knee arthroplasty: a short-term evaluation. J Knee Surg 30:849–853
Mitchell J, Wang J, Bukowski B, Greiner J, Wolford B, Oyer M, Illgen RL 2nd (2021) Relative clinical outcomes comparing manual and robotic-assisted total knee arthroplasty at minimum 1-year follow-up. HSS J 17:267–273
Nam D, Maher PA, Rebolledo BJ, Nawabi DH, McLawhorn AS, Pearle AD (2013) Patient specific cutting guides versus an imageless, computer-assisted surgery system in total knee arthroplasty. Knee 20:263–267
Naziri Q, Cusson BC, Chaudhri M, Shah NV, Sastry A (2019) Making the transition from traditional to robotic-arm assisted TKA: What to expect? A single-surgeon comparative-analysis of the first-40 consecutive cases. J Orthop 16:364–368
Park SE, Lee CT (2007) Comparison of robotic-assisted and conventional manual implantation of a primary total knee arthroplasty. J Arthroplasty 22:1054–1059
Pierce J, Needham K, Adams C, Coppolecchia A, Lavernia C (2020) Robotic arm-assisted knee surgery: an economic analysis. Am J Manag Care 26:e205–e210
Ritter MA, Davis KE, Meding JB, Pierson JL, Berend ME, Malinzak RA (2011) The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg Am 93:1588–1596
Sappey-Marinier E, Pauvert A, Batailler C, Swan J, Cheze L, Servien E, Lustig S (2020) Kinematic versus mechanical alignment for primary total knee arthroplasty with minimum 2 years follow-up: a systematic review. SICOT-J 6:18
Savov P, Tuecking L-R, Windhagen H, Ehmig J, Ettinger M (2021) Imageless robotic handpiece-assisted total knee arthroplasty: a learning curve analysis of surgical time and alignment accuracy. Arch Orthop Trauma Surg 141:2119–2128
Shaw JH, Lindsay-Rivera KG, Buckley PJ, Weir RM, Banka TR, Davis JJ (2021) Minimal clinically important difference in robotic-assisted total knee arthroplasty versus standard manual total knee arthroplasty. J Arthroplasty 36:S233–S241
Sires JD, Craik JD, Wilson CJ (2021) Accuracy of bone resection in MAKO total knee robotic-assisted surgery. J Knee Surg 34:745–748
Sires JD, Wilson CJ (2021) CT Validation of intraoperative implant position and knee alignment as determined by the MAKO total knee arthroplasty system. J Knee Surg 34:1133–1137
Smith AF, Eccles CJ, Bhimani SJ, Denehy KM, Bhimani RB, Smith LS, Malkani AL (2021) Improved patient satisfaction following robotic-assisted total knee arthroplasty. J Knee Surg 34:730–738
Smith TJ, Siddiqi A, Forte SA, Judice A, Sculco PK, Vigdorchik JM, Schwarzkopf R, Springer BD (2021) Periprosthetic fractures through tracking pin sites following computer navigated and robotic total and unicompartmental knee arthroplasty: a systematic review. JBJS Rev 9(e20):00091
Sodhi N, Khlopas A, Piuzzi NS, Sultan AA, Marchand RC, Malkani AL, Mont MA (2018) The learning curve associated with robotic total knee arthroplasty. J Knee Surg 31:17–21
Song E-K, Seon J-K, Park S-J, Bin JW, Park H-W, Lee GW (2011) Simultaneous bilateral total knee arthroplasty with robotic and conventional techniques: a prospective, randomized study. Knee Surgery, Sport Traumatol Arthrosc 19:1069–1076
Song EK, Seon JK, Yim JH, Netravali NA, Bargar WL (2013) Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA knee. Clin Orthop Relat Res 471:118–126
St Mart J-P, de Steiger RN, Cuthbert A, Donnelly W (2020) The three-year survivorship of robotically assisted versus non-robotically assisted unicompartmental knee arthroplasty. Bone Joint J 102-B:319–328
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan A-W, Churchill R, Deeks JJ, Hróbjartsson A, Kirkham J, Jüni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schünemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JP (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:i4919
Stulberg BN, Zadzilka JD (2021) Active robotic technologies for total knee arthroplasty. Arch Orthop Trauma Surg 141:2069–2075
Suero EM, Plaskos C, Dixon PL, Pearle AD (2012) Adjustable cutting blocks improve alignment and surgical time in computer-assisted total knee replacement. Knee Surg Sports Traumatol Arthrosc 20:1736–1741
Sultan AA, Samuel LT, Khlopas A, Sodhi N, Bhowmik-Stoker M, Chen A, Orozco F, Kolisek F, Mahoney O, Smith L, Malkani A, Molloy RM, Mont MA (2019) Robotic-arm assisted total knee arthroplasty more accurately restored the posterior condylar offset ratio and the insall-salvati index compared to the manual technique; a cohort-matched Study. Surg Technol Int 34:409–413
Vaidya N, Jaysingani TN, Panjwani T, Patil R, Deshpande A, Kesarkar A (2021) Assessment of accuracy of an imageless hand-held robotic-assisted system in component positioning in total knee replacement: a prospective study. J Robot Surg 16:361–367
Vaidya NV, Deshpande AN, Panjwani T, Patil R, Jaysingani T, Patil P (2022) Robotic-assisted TKA leads to a better prosthesis alignment and a better joint line restoration as compared to conventional TKA: a prospective randomized controlled trial. Knee Surg Sports Traumatol Arthrosc 30:621–626
Vanlommel L, Neven E, Anderson M, Bruckers L, Truijen J (2021) The initial learning curve for the ROSA® knee system can be achieved in 6–11 cases for operative time and has similar 90-day complication rates with improved implant alignment compared to manual instrumentation in total knee arthroplasty. J Exp Orthop 8:1–12
Vermue H, Luyckx T, Winnock de Grave P, Ryckaert A, Cools AS, Himpe N, Victor J (2022) Robot-assisted total knee arthroplasty is associated with a learning curve for surgical time but not for component alignment, limb alignment and gap balancing. Knee Surg Sports Traumatol Arthrosc 30(2):593–602. https://doi.org/10.1007/s00167-020-06341-6
Wakelin EA, Shalhoub S, Lawrence JM, Keggi JM, DeClaire JH, Randall AL, Ponder CE, Koenig JA, Lyman S, Plaskos C (2021) Improved total knee arthroplasty pain outcome when joint gap targets are achieved throughout flexion. Knee Surg Sports Traumatol Arthrosc 30:939–947
Yang HY, Seon JK, Shin YJ, Lim HA, Song EK (2017) Robotic total knee arthroplasty with a cruciate-retaining implant: a 10-year follow-up study. Clin Orthop Surg 9:169–176
Funding
Fonds Wetenschappelijk Onderzoek, 11F5919N, Hannes Vermue.
Author information
Authors and Affiliations
Contributions
Conceptualisation: PM, FH, SL, TL, and EKS Consensus Group. Methodology: HV, CB, PM, FH, SL, and TL. Data analysis: HV and CB. Writing—original draft preparation: HV and CB. Writing—review and editing: PM, FH, SL, and TL.
Corresponding author
Ethics declarations
Conflict of interest
One or more of the authors has declared the following potential conflict of interest or source of funding: HV was financially supported by doctoral grant 11F5919N from the Research Foundation Flanders. CB reports payment for lectures by Lepine, all outside the submitted work. PM has received consultancy fees from Zimmer-Biomet, all outside the submitted work. FH reports board membership of the Bone and Joint Journal, the Trustee British Orthopaedic Association and the Bosta Executive Committee; consultancy for Stryker; payment for lectures by AO recon, Bone and Joint Journal, Smith & Nephew and Stryker; royalties paid by Smith & Nephew, MatOrtho, Corin and Stryker, all outside the submitted work. TL reports consultancy for Corin, Lima and Stryker, as well as royalties paid by Corin, all outside the submitted work. SL reports board membership of the Journal of Bone & Joint Surgery, the SICOT Journal, the Journal of Experimental Orthopaedics, board membership of the EKS and ISAKOS; royalties paid by Stryker and Smith & Nephew; consultancy for Amplitude, Groupe Lepine and Heraeus, all outside the submitted work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vermue, H., Batailler, C., Monk, P. et al. The evolution of robotic systems for total knee arthroplasty, each system must be assessed for its own value: a systematic review of clinical evidence and meta-analysis. Arch Orthop Trauma Surg 143, 3369–3381 (2023). https://doi.org/10.1007/s00402-022-04632-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04632-w