Abstract
Purpose
The application of robotics in the operating theatre for total knee arthroplasty (TKA) remains controversial. As with all new technology, the introduction of new systems is associated with a learning curve and potentially associated with extra complications. Therefore, the aim of this study is to identify and predict the learning curve of robot-assisted (RA) TKA.
Methods
A RA TKA system (MAKO) was introduced in April 2018 in our service. A retrospective analysis was performed of all patients receiving a TKA with this system by six surgeons. Operative times, implant and limb alignment, intraoperative joint balance and robot-related complications were evaluated. Cumulative summation (CUSUM) analyses were used to assess learning curves for operative time, implant alignment and joint balance in RA TKA. Linear regression was performed to predict the learning curve of each surgeon.
Results
RA TKA was associated with a learning curve of 11–43 cases for operative time (p < 0.001). This learning curve was significantly affected by the surgical profile (high vs. medium vs. low volume). A complete normalisation of operative times was seen in four out of five surgeons. The precision of implant positioning and gap balancing showed no learning curve. An average deviation of 0.2° (SD 1.4), 0.7° (SD 1.1), 1.2 (SD 2.1), 0.2° (SD 2.9) and 0.3 (SD 2.4) for the mLDFA, MPTA, HKA, PDFA and PPTA from the preoperative plan was observed. Limb alignment showed a mean deviation of 1.2° (SD 2.1) towards valgus postoperatively compared to the intraoperative plan. One tibial stress fracture was seen as a complication due to suboptimal positioning of the registration pins.
Conclusion
RA TKA is associated with a learning curve for surgical time, which might be longer than reported in current literature and dependent on the profile of the surgeon. There is no learning curve for component alignment, limb alignment and gap balancing.
Level of evidence
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Early failure following total knee arthroplasty (TKA) is often related to surgical errors [8]. Avoiding these errors by improving precision in component positioning and soft-tissue balance could improve functional results. Evolution in surgical technology has led to the development of surgical robots to execute the surgery with high accuracy and aid in soft tissue balance.
The use of new technologies follows a learning curve, both in relation to the obtained position of the implant and the time needed to perform the operation.
The error of surgical positioning could be twofold. First, there is the failure to define the desired position in relation to the patient’s anatomy, which is planning error. Second, there is the failure to perform the procedure reliably with a resulting deviation to the desired position, which is the precision error.
Both traditional surgery and robotic surgery can fail on these two points. With Computed Tomography (CT) based robotic surgery, the CT scan can deliver additional information to improve the planning of the procedure. The elimination of surgical errors in fixing cutting blocks and executing motorized bone cuts could improve on the precision part of the procedure.
For robot-assisted (RA) TKA surgery, a learning curve can be seen when evaluating the operative times of consecutive cases [7, 12, 17]. However, prior studies on the learning curve of robot-assisted TKA have only included a maximum of two surgeons [7, 11, 12, 17]. The hypothesis of this research project states that a surgeon’s learning curve of RA TKA is more variable and longer than expected in the current literature.
Therefore, the aim of this study was to determine the learning curve for surgeons utilizing a haptic surgical robot for TKA at three different levels: (1) surgical time, (2) precision of limb alignment and (3) precision of component position. Second, complications related to the use of the robotic system were registered.
Material and methods
The authors obtained approval by the institutional ethical committee for this study (B117201940872). The MAKO robotic platform (Stryker, Michigan, USA) was introduced in our department in April 2018. All patients who underwent TKA between April 2018 and September 2019 due to end-stage primary osteoarthritis of the knee joint were retrospectively reviewed and included in this study. Exclusion criteria were: conversion from unicompartmental knee arthroplasty to total knee arthroplasty, infection, neurological dysfunction limiting knee mobility, posttraumatic osteoarthritis with severe knee deformity and lack of radiographs in the patient file. All patients eligible to the in- and exclusion criteria received RA TKA.
Patients who underwent conventional TKA surgery by the same group of surgeons in the second half of 2017, prior to the introduction of the surgical robot, were included as a control group. Identical inclusion and exclusion criteria were used. All surgeons contributed > 25 cases to the control group. Low, medium and high volume surgeons were seen as surgeons performing < 50, 50–100 and > 100 TKA cases/year respectively [9, 20].
Surgery
The surgeries were performed by six fellowship-trained surgeons (Table 1). A subvastus approach was used in all cases. The Triathlon (Stryker, Michigan, USA) cruciate retaining (CR) or posterior stabilized (PS) implant was utilized.
Femoral pins (4 mm diameter) were positioned in the wound underneath the vastus medialis. Tibial pins (3.2 mm diameter) were positioned 10 cm below the surgical incision through two step incisions.
All surgeons completed 4 h of theoretical training and 2 h of cadaveric training on robot-assisted total knee arthroplasty with MAKO technology. Annual TKA case volume was estimated based on the conventional TKA cases performed in the second half of 2017.
Outcome measures
Retrospective review of the office notes, hospital records, radiographs and intra-operative data was independently performed by the principal author (HV). Radiographs were additionally assessed by two other independent reviewers (ASC, NH).
Operative time
In this study, the operative time was defined as the time between initial skin incision to final wound closure. The operative time was extracted from the electronical patient file, which is filled in during the surgery.
Intraoperative plan
The intraoperative plan on implant positioning was evaluated, taking into account possible intraoperative alterations. As such, femoral and tibial implant positioning and the planned hip-knee-ankle axis of the involved leg was obtained. Joint balance was evaluated with final medial and lateral gaps between femur and tibia in extension and flexion, similar to the studies of Gu et al. and Song et al. [4, 18, 19]. Imbalance was defined as a mismatch of more than 2 mm in either the medial, lateral, extension or flexion compartment. Tensioning of the gaps was performed manually with spoons or with a lamina spreader until equal tension of the collateral ligaments was achieved, guided by the experience of the surgeon.
Radiological
Patients’ pre- and postoperative full leg radiograph and sagittal knee radiograph were reviewed according to Paley et al. and Ewald by three independent examiners [2, 13]. An EOS system (EOS imaging, Paris, France) was utilised to obtain full leg standing radiographs. Full leg radiographs used for coronal limb alignment and coronal implant alignment. The hip-knee-ankle (HKA) axis was defined as the angle between the mechanical axis of the femur and the mechanical axis of the tibia. Femoral coronal alignment was measured with the mechanical lateral distal femoral angle (mLDFA), which is the angle between the mechanical axis of the femur and the line connecting the most distal points on the medial and lateral femoral condyle. Tibial coronal alignment was defined as the medial proximal tibial angle (MPTA), which is the angle between the mechanical axis of the tibia and the line connecting the medial to the lateral base of the tibial plateau. True lateral knee radiographs were used for evaluation of sagittal alignment with the posterior distal femoral angle (PDFA) and posterior proximal tibial angle (PPTA). The precision of component positioning was defined as the deviation of the postoperative component position on the radiographs versus the intraoperative navigation data. Postoperative coronal alignment data were only assessed in case a full leg radiograph was available.
The cohort was split based on the preoperative HKA: valgus knees (HKA > 3° valgus), neutral knees (3° valgus ≤ HKA ≤ 3° varus) and varus knees (HKA > 3° varus). The change of HKA and coronal implant alignment was evaluated as well, based on the differentiation between valgus, neutral and varus knees.
Complications
All patient files were reviewed for robot-related complications, such as fractures of the femur or tibia due to pin placement or wound infection at the pin tracts.
Statistical analysis
Sample size calculation was based on the operative times, which is the primary outcome of this study. To detect a minimal clinical difference of 5 min (SD 10 min) with a power of 0.80 and alpha set at 0.05 at least 60 patients are required in each arm [7, 15].
Categorical data analysis is performed with Chi-Square test. Homogeneity of variances was evaluated with Levene’s Test. Normal distribution of continuous variables was tested with the Shapiro Wilk test and visually verified with boxplots. Parametric data were analysed using independent t test in case of unpaired variables and one-way ANOVA in case of multiple variables. Univariate linear regression was performed with the operative time as an dependent variable and the consecutive case number of each surgeon as independent variable. Statistical significance was set at 0.05. The learning curve of the time used for robot-assisted TKA was assessed with cumulative summation analysis (CUSUM), similar to Kayani et al. [7]. A cumulative sum is a running total of the sum of the deviations of all individual sample results from a prespecified target. An inflexion point in the visualised trend is defined as the transition from a learning phase to a proficiency phase. The target used for the operative time used for robot-assisted TKA was the mean average of operative time for every surgeon individually. Similarly, the difference between postoperative coronal and sagittal alignment of femoral and tibial component compared to the intraoperative plan were evaluated with CUSUM analysis. MATLAB 2016a (MathWorks, Massachusetts, USA) was used to perform the statistical analysis.
Results
A total of 386 patients were included in the present study. Six patients were excluded according to the exclusion criteria. Three patients lacked radiographs in the electronical patient file. Two patients suffered from post-traumatic osteoarthritis with severe knee deformity. One patient was excluded due to a prior history of septic arthritis of the knee joint. The RATKA group did not show statistically significant differences in age, BMI, gender and HKA compared to the control group (see Table 2).
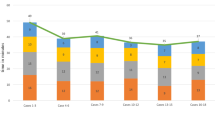
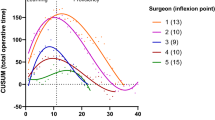
Operative times based on surgical volume
In the robot-assisted TKA cases, CUSUM analysis showed a clear inflexion point for high-volume surgeons (Surgeon 3, 5 and 6) after 11, 43 and 22 cases respectively (Fig. 1). Analysis of the learning phase (prior to the inflexion point) compared to the proficiency phase (after the inflexion point) showed longer operative times during the learning phase (p < 0.001 for Surgeon 3, 5 and 6) without differences in baseline characteristics of the involved patients.
Similarly, the operative times of the first 10 robot-assisted cases were significantly longer than operative times prior to the introduction of the robotic system. As Surgeon 2 did not reach 10 cases in the study time interval, the analysis was performed on the cases of the remaining surgeons. The last 10 robot-assisted cases of all but one surgeon (Surgeon 3) did not differ significantly from the conventional TKA control group (p > 0.05; Table 3; Fig. 2). The mean change of OR times of the first 10 robot-assisted cases versus the last 10 robot-assisted TKA cases was 31.6 min (SD 22.1; Fig. 3). The percentual difference (relative to the control group) was a 34.1% (SD 20.8) decrease of OR time.
Linear regression analysis showed a correlation between the amount of robot-assisted TKA cases performed and the skin-to-skin time for the high-volume surgeon (Fig. 4). The mean decrease for every case in the linear regression parameter for these three surgeons is 0.4 min (SD 0.3) per case.
Intraoperative balancing
With CUSUM analysis, no learning curve could be described regarding the achievement of balanced medial, lateral, extension and flexion compartments of the knee joint. A balance mismatch was prevalent in 3.5, 3.5, 1.5 and 1.5% of all robot-assisted TKA cases for the medial, lateral, extension and flexion compartments respectively. The difference between all compartments was not significant (p > 0.05).
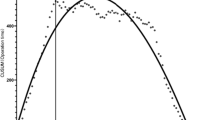
Component alignment
All radiographic measurements were reproducible, with intra- and interrater correlation coefficients of > 0.7 for HKA, mLDFA, MPTA and PPTA; > 0.5 for PDFA. CUSUM analysis did not result in a clear inflexion point regarding the deviation between postoperative alignment and the intraoperative plan.
Postoperative full leg radiographs were available in 108 out of 386 patients. Postoperative analysis of the femoral and tibial component alignment versus the intraoperative navigation data showed a mean precision of 0.2 (SD 1.4), 0.7 (SD 1.1), 0.2 (SD 2.9) and 0.3 (SD 2.4) degrees for the mLDFA, MPTA, PDFA and PPTA respectively. On average, the postoperative HKA was aligned in 1.2° (SD 2.1) more valgus as measured on full leg standing radiographs compared to the intraoperative navigation data. Overall distribution of postoperative HKA, MPTA and mLFDA showed outliers were still present in the robot-assisted TKA cohort (Fig. 5).
No significant differences in the precision of postoperative alignment were observed in the different alignment groups (valgus vs neutral vs varus) (Table 4).
In valgus knees, the correction of the coronal alignment was seen on the distal femur (3.2° SD 2.3). In varus knees, this correction was found on the proximal tibia (2.9° SD 2.9) (Table 5).
Complications
One complication related to the tibial pin placement was observed. The patient presented with persistent pain on the anterior side of the shin. Further investigations resulted in the diagnosis of a diaphyseal tibial stress fracture caused by the registration pin insertion (Fig. 6). This healed uneventfully after 8 weeks.
Discussion
The most important finding of this study was that a learning curve for an operative time was present after the introduction of robot-assisted total knee arthroplasty but not for the precision of limb alignment or component positioning. The clinical significance of a learning curve lies in the ability to identify the learning curve of an individual surgeon, prior to starting with RA TKA in his/her practice.
It is possible that the learning curve of robot-assisted total knee arthroplasty is longer than defined in the current literature [7, 11, 12, 17, 21]. CUSUM analysis in this study visualised inflexion points based on operative time after 11, 22 and 43 cases for three surgeons. The included surgeons in this study had a longer learning curve than defined by Kayani et al. who saw an inflexion point at seven cases based on operative time [7]. No other studies evaluated the learning curve after robot-assisted total knee arthroplasty with CUSUM analysis. The longer learning curve in this study might be associated with the real-life setting in which this study was performed due to its retrospective nature. It was not possible to have an identical surgical team for all RA TKA cases of an individual surgeon, leading to a slower increase in experience of a surgical nurse.
However, the overall operative times between all surgeons in both the control group and the RA-TKA group did show significant differences, as can be seen in Fig. 4. Surgeon 5 and 6, two high volume surgeons, were both 5 years into practice, which might be the reason why they have longer OR times compared to Surgeon 1, a medium volume surgeon with longer clinical experience. Surgeon 3 has the lengthiest career combined with performing > 100 TKA cases annually, resulting in the lowest OR times.
In this study, an overall normalisation of operative times was seen in the robot-assisted total arthroplasty group compared to conventional total knee arthroplasty group for 4 out of 5 surgeons. However, this implies that one surgeon did not reach the normalisation of operative times, which has not yet been reported in the current literature. There are possible factors associated with the lack of operative time normalisation. First, for this surgeon the mean operative time prior to the introduction of the robot assistance is lower compared to the other surgeons. Second, the involved surgeon is a high volume TKA surgeon (> 100 cases/year). The combination of efficient operative times and high volume per year might be evidence of an already efficient workflow with conventional total knee arthroplasty, which could not be matched in overall operative time for robot-assisted total knee arthroplasty.
One of the main benefits of robotic technology for total knee arthroplasty is positioning the prosthesis accurately compared to the preoperative plan [5, 19]. In this study, it is confirmed that performing consecutive robot-assisted cases did not impact the accuracy of postoperative alignment compared to the intraoperative plan. Mean precision below one degree for postoperative coronal implant position could therefore be achieved from the initial cases. By being able to visualize the intraoperative variables quantified on the robot hardware the surgeon is capable to strive for the ideal positioning and balancing. As such, the surgeon might be able to achieve learning curve being non-existent for component alignment and ligament balance of the knee joint [7]. Although the mean precision of coronal and sagittal implant position was low, caution is necessary due to the wider distribution of the analysed alignment variables. The broad distribution of HKA angle, MPTA and mLDFA in Fig. 6 shows there is still some variation possible when performing robot-assisted TKA. Additionally, it shows there robot-assisted TKA might not be able to avoid all outliers in coronal alignment. In current literature, RA TKA has been proven to provide a reduction in the amount of outliers from neutral coronal alignment (≤ 3° varus or valgus) compared to conventional TKA [1, 6, 10, 16, 19, 23]. However, the clear superiority of RA TKA achieving higher accuracy in coronal or sagittal alignment compared to conventional TKA remains up for debate [1, 14, 23].
Important to note is the systematic valgus deviation (1.2°) on postoperative full leg radiographs compared to the planned limb alignment. This deviation is not associated to the preoperative lower limb alignment although the magnitude of error on the tibial component seems to be slightly larger in varus and neutral knees. This systematic deviation to valgus lower limb alignment could be related to a methodical error in the intraoperative planning phase, in which the coordinate for the tibial knee center is defined more laterally or the ankle center is defined more medially. Similarly, for the femoral coordinates, the femoral knee center could be defined more laterally, whereas the hip center might be defined more medially. As these coordinates are used to construct a reference frame for the lower limb, their identification is crucial [3]. Victor et al. have found a maximal inter-observer error of 3.3 mm for the identification of the tibial knee center between three orthopaedic surgeons [22]. This variation could only account for an angular error of 0.34° for the mechanical axis of the tibia in the coronal plane. The intra- and interobserver error of the other coordinates used for the definition of the knee coordinate system was less than 1 mm. Furthermore, it is not known how a surgeons’ experience in knee surgery affects the positioning of these coordinates. Initial surgical plans are often determined by company employees, prior to evaluation of the surgeon. When not carefully evaluated and adapted by the surgeon, coordinate positioning errors might be possible in the surgical plan. Additionally, the EOS system requires the patients to stand still with one foot (non-operative leg) in front of the other (operative leg) when seen from the side. As the operative leg is positioned in a neutral position for the patient and the other foot is set relative to this position, it might lead to a systematic valgus deviation during radiographic measurements.
Another benefit of RA TKA is the possibility to achieve improved ligament balancing. Flexion- and extension gap balancing has been shown to be superior in RA TKA with ROBODOC compared to the conventional technique in studies by Song et al. [18, 19].
In this study, we observed one (stress) fracture, which is one of the typical complications after robot-assisted total knee arthroplasty. Care should be taken to position the tibial registration pins centric in the tibia anteroposterior. Additionally, as both pins of 4 and 3.2 mm are available, the smaller pins of 3.2 mm might lead to less complications.
This study does have some limitations. Most important is the retrospective nature of this study, which could imply confounding factors in patient characteristics due to the lack of randomisation. However, no difference in patient characteristics was seen between the RATKA and conventional TKA group.
To predict the learning curve of an individual surgeon after the introduction of robotic assistance in total knee procedures, the learning curve of a broader population of surgeons should be examined, including individual surgeon characteristics. Additionally, more research is needed to evaluate the effect of experience in knee surgery on the reliability to identify anatomical landmarks around the knee joint.
Conclusion
The introduction of a robot for assistance during total knee arthroplasty is associated with a longer learning curve than currently reported in the literature. Surgeons starting with robotics for TKA surgery should foresee enough time to cope with this learning curve during the first 11–43 cases.
References
Cho KJ, Seon JK, Jang WY, Park CG, Song EK (2019) Robotic versus conventional primary total knee arthroplasty: clinical and radiological long-term results with a minimum follow-up of ten years. Int Orthop 43:1345–1354
Ewald FC (1989) The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 248:9–12
Grood ES, Suntay WJ (1983) A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech 105:136–144
Gu Y, Howell SM, Hull ML (2017) Simulation of total knee arthroplasty in 5° or 7° valgus: a study of gap imbalances and changes in limb and knee alignments from native. J Orthop Res 35:2031–2039
Hampp EL, Chughtai M, Scholl LY, Sodhi N, Bhowmik-Stoker M, Jacofsky DJ, Mont MA, Hampp EL, Chughtai M, Scholl LY, Sodhi N, Bhowmik-Stoker M, Jacofsky DJ, Mont MA (2019) Robotic-arm assisted total knee arthroplasty demonstrated greater accuracy and precision to plan compared with manual techniques. J Knee Surg 32:239–250
Jeon S-W, Kim K-I, Song SJ (2019) Robot-assisted total knee arthroplasty does not improve long-term clinical and radiologic outcomes. J Arthroplasty 34:1656–1661
Kayani B, Konan S, Huq SS, Tahmassebi J, Haddad FS (2019) Robotic-arm assisted total knee arthroplasty has a learning curve of seven cases for integration into the surgical workflow but no learning curve effect for accuracy of implant positioning. Knee Surg Sports Traumatol Arthrosc 27:1132–1141
Khan M, Osman K, Green G, Haddad FS (2016) The epidemiology of failure in total knee arthroplasty: avoiding your next revision. Bone Joint J 98-B:105–112
Lau RL, Perruccio AV, Gandhi R, Mahomed NN (2012) The role of surgeon volume on patient outcome in total knee arthroplasty: a systematic review of the literature. BMC Musculoskelet Disord 13:250
Liow MHL, Xia Z, Wong MK, Tay KJ, Yeo SJ, Chin PL (2014) Robot-assisted total knee arthroplasty accurately restores the joint line and mechanical axis A prospective randomised study. J Arthroplast 29:2373–2377
Marchand RC, Sodhi N, Khlopas A, Sultan AA, Harwin SF, Malkani AL, Mont MA (2017) Patient satisfaction outcomes after robotic arm-assisted total knee arthroplasty: a short-term evaluation. J Knee Surg 30:849–853
Naziri Q, Cusson BC, Chaudhri M, Shah NV, Sastry A (2019) Making the transition from traditional to robotic-arm assisted TKA: what to expect? A single-surgeon comparative-analysis of the first-40 consecutive cases. J Orthop 16:364–368
Paley D, Pfeil J (2000) Principles of deformity correction around the knee. Orthopade 29:18–38
Park SE, Lee CT (2007) Comparison of robotic-assisted and conventional manual implantation of a primary total knee arthroplasty. J Arthroplasty 22:1054–1059
Seon JK, Song EK (2006) Navigation-assisted less invasive total knee arthroplasty compared with conventional total knee arthroplasty: a randomized prospective trial. J Arthroplasty 21:777–782
Siebert W, Mai S, Kober R, Heeckt PF (2002) Technique and first clinical results of robot-assisted total knee replacement. Knee 9:173–180
Sodhi N, Khlopas A, Piuzzi NS, Sultan AA, Marchand RC, Malkani AL, Mont MA (2018) The learning curve associated with robotic total knee arthroplasty. J Knee Surg 31:17–21
Song E-K, Seon J-K, Park S-J, Bin JW, Park H-W, Lee GW (2011) Simultaneous bilateral total knee arthroplasty with robotic and conventional techniques: a prospective, randomized study. Knee Surgery, Sport Traumatol Arthrosc 19:1069–1076
Song EK, Seon JK, Yim JH, Netravali NA, Bargar WL (2013) Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA knee. Clin Orthop Relat Res 471:118–126
Tan S-C, Chan Y-H, Chong H-C, Chin P-L, Yew A, Chia S-L, Tay D, Lo N-N, Yeo S-J (2014) Association of surgeon factors with outcome scores after total knee arthroplasty. J Orthop Surg 22:378–382
Vermue H, Lambrechts J, Tampere T, Arnout N, Auvinet E, Victor J (2020) How should we evaluate robotics in the operating theatre? Bone Joint J 102-B:407–413
Victor J, Van Doninck D, Labey L, Innocenti B, Parizel PM, Bellemans J (2009) How precise can bony landmarks be determined on a CT scan of the knee? Knee 16:358–365
Yang HY, Seon JK, Shin YJ, Lim HA, Song EK (2017) Robotic total knee arthroplasty with a cruciate-retaining implant: a 10-year follow-up study. Clin Orthop Surg 9:169–176
Funding
The authors declare no acceptance of external funding.
Author information
Authors and Affiliations
Contributions
HV: data collection and presentation, manuscript preparation. TL: data collection and interpretation, manuscript preparation. PWG: data interpretation. AR: data collection. A-SC: data collection. NH: data collection. JV: data interpretation, manuscript preparation.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest or acceptance of external funding.
Ethical approval
The authors obtained approval by the institutional ethical committee for this study (B117201940872).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vermue, H., Luyckx, T., Winnock de Grave, P. et al. Robot-assisted total knee arthroplasty is associated with a learning curve for surgical time but not for component alignment, limb alignment and gap balancing. Knee Surg Sports Traumatol Arthrosc 30, 593–602 (2022). https://doi.org/10.1007/s00167-020-06341-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06341-6