Abstract
Purpose
The most criticism of antegrade humeral nailing is the potentially deleterious effect on the shoulder function, which is caused by the trauma to the M. supraspinatus (SSP) at the nail insertion site. We describe a new technique of all-arthroscopical intramedullary nailing, which preserves the rotator cuff, and compare it with the conventional open procedure.
Methods
From 11/2009 to 12/2010 82 patients with unstable, displaced proximal humeral fractures were treated surgically. Twenty-one of these patients received an intramedullary nailing. Sixteen of 21 met the inclusion criteria. Based on the surgeon’s arthroscopic experience, patients were assigned to the arthroscopic (group I, n = 8) or open group (group II, n = 8). Both groups were compared due to the replacement results, complications, time of surgery and fluoroscopy. Concomitant intraarticular pathologies were assessed (group I). First clinical results after a median follow-up of 13 months (group I) and 14 months (group II) were reported.
Results
Between group I and II, no significant differences were seen in patients age [77 years (range 45–90 years) vs. 76 years (range 65–92 years)], gender (6 female/2 male vs. 5 female/3 male) and fracture pattern (six 2-/two 3-part fractures vs. five 2-/three 3-part fractures). The reduction was evaluated by the caput-diaphysis-angle, which was median 137° (range 120–147°) in group I and 132° (range 120–158°) in group II (p = 0.959). Postoperatively, group I showed one varus-, group II two varus- and valgus deformities. Median time of surgery was 75 min (range 45–182 min) versus 70 min (range 40–146 min) (p = 0.442), fluoroscopy time 1.5 min (range, 0.6–3.7 min) versus 1.2 min (range 0.3–2.2 min) in group I and II (p = 0.336). Concomitant pathologies like one traumatic bicipital tendon-lesion and three partial lesions of the SSP were observed and treated in group I. Constant Scores and Visual Analogue Scale did not differ significantly between both groups at the time of follow-up.
Conclusions
All-arthroscopical humeral nailing is possible, preserves the rotator cuff and provides equal replacement and functional results like the open technique. An arthroscopically visualized optimal nail insertion point provides less frequent head deformities.
Level of evidence Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Proximal humeral fractures are still a challenge in the elderly patient with osteoporotic bone structure [1, 8, 9, 11, 12, 15]. Optimal operative strategy regarding complex fracture patterns is still a discussed controversy. The intramedullary nailing has established as one of the standard treatments especially for unstable, displaced 2- and 3-part fractures (Codman-classification [2]) with predominantly satisfying to good results [1, 8, 9]. However, the most frequent criticism of antegrade humeral nailing (and nail removal) is the potentially deleterious effect on the shoulder function, which is caused by the trauma to the M. supraspinatus (SSP) at the nail insertion point [6]. So, the intramedullary nailing was recommended predominantly for elderly patients [8].
We present a new technique of arthroscopic intramedullary nailing of proximal humeral fractures with the advantages of the minimally invasive surgery, with the effort to decrease the SSP-trauma and to suture the SSP-insertion point arthroscopically, and with the possibility to treat concomitant intraarticular pathologies. The first intra- and early postoperative results of arthroscopic and open nailing are described. We hypothesized that arthroscopical intramedullary nailing of proximal humeral fractures is possible, preserves the rotator cuff and provides equal replacement results like the conventional open technique.
Methods
Surgical indications
Surgical indications for (arthroscopic) nailing are displaced, unstable 2- and 3-part fractures of the proximal humerus, proximal spiral fractures, subcapital fractures with a wide comminute zone and nonunions.
Contraindications are complex intraarticular fractures, head-split fractures, fractures in younger patients.
Surgical technique
The arthroscopic procedure is performed under general anesthesia. The patient is placed in beach chair position. The injured arm is hanging free, so that a spontaneous ad axis-replacement of the main fracture fragments (head and shaft fragment) can be occured. The image intensifier is pre-positioned and integrated in the operative set up.
The anatomic landmarks for shoulder arthroscopy are marked. The standard posterior portal is the scope-portal during the whole operation (Fig. 1). Under direct vision the anteroinferior standard portal is placed superior to the subscapularis tendon for instrumental passage. A standard diagnostic arthroscopy was performed to evaluate the glenohumeral joint and to treat potential intraarticular, concomitant injuries of the proximal humeral fracture, like lesion/displacement of the long biceps tendon, rotator cuff tears and/or chondral lesions. If necessary, a biceps tenodesis, chondroplasty or rotator cuff debridement/repair could be performed.
In case of a varus malposition of the humeral head fragment, it could be necessary to reduce and retain the humeral head with an elevatorium, which was percutaneously inserted from lateral in the subcapital fracture area under fluoroscopic control (Fig. 2). An anteroacromial portal was applied after needling directly in front of the anterior acromion margin and about 1 cm medial of the lateral acromial edge, transtendinous and posterior of the long bicipital tendon (Figs. 2, 3). If there was a prominent anterior acromion edge, an arthroscopic acromioplasty (3–4 mm) was necessary in two cases before finding the ideal insertion point of the nail. We use a straight nail model (Targon PH®, Aesculap, Tuttlingen, Germany) with a central nail insertion site. This offers more reliable anchorage in the humeral head than an angulated nail with a more lateral insertion point [7].
A guide pin is inserted through the anteroacromial portal and a small SSP-incision (1 cm, lengthwise with the fibers) to the ideal nail insertion site at the apex (highest point) of the humeral head. The apex of the humeral head was identified via arthroscopy in the anterior–posterior direction and via arthroscopy and fluoroscopy in the medial–lateral direction. Subsequently, the guide pin was drilled in the apex of the humeral head (Fig. 4). A probe in the anteroinferior portal could be used to lift the rotator cuff, and to control the drill-procedure. If the insertion point is correct, a hollow reamer overdrills the guide pin (Fig. 4). Under arthroscopic control, the nail was inserted until the superior nail edge was closely subchondral (Fig. 5).
Arthroscopy was interrupted, and four head screws as well as two shaft screws were inserted via a targeting device using small skin incisions. Fluoroscopy in tow planes (true ap and axillary view) controlled and documented the correct fragment replacement, implantat position and screw lengths.
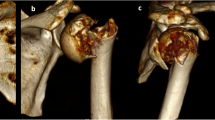
Re-arthroscopy was performed. The localized small rotator cuff lesion in the area of nail insertion is closed under arthroscopic view with a side-to-side suture. Finally, the small skin incisions were sutured and sterile bandage was applied. Two days after surgery a X-ray (true ap and Y-view) were performed to control the correct fracture reduction and implant position (Fig. 6).
Postoperative management
For the first 3 days, the arm was immobilized in a sling. After that, an early functional physiotherapy started with an unlimited range of motion, and without any loading for 6 weeks postoperatively.
Study design: case series
Between November 2009 and December 2010, 82 displaced proximal humeral fractures were surgically treated at the author’s institution: 43 with locking plates, 21 with intramedullary nailing and 18 with hemiarthoplasty. The ideal indication for intramedullary nailing was seen in displaced, unstable subcapital 2- and 3-part fractures with non/slightly (<5 mm) displaced greater tuberosity as well as in proximal shaft spiral fractures. The inclusion criteria of this study were: (1) displaced subcapital 2- or 3-part fractures with non/slightly (<5 mm) displaced greater tuberosity within 7 days after trauma, (2) no previous fractures or surgical procedures of the affected shoulder, (3) no deforming musculoskeletal or neurological disorders of the shoulder girdle, (4) a patient’s age over 18 years.
Sixteen of 21 sequential patients treated with intramedullary nailing met the inclusion criteria. Based on the primary surgeon’s preference and arthroscopic experience, patients were assigned to the arthroscopic (group I) or the conventional open group (group II). Eight of the 16 included patients were treated in the described new arthroscopic technique (group I) by the first author, the other eight patients were treated in the conventional open anterior delta-split nailing technique [7]. Patients data, fracture types, intraoperative parameters and the postoperative clinical and radiological results were evaluated and compared between the open and the new arthroscopic technique. First clinical results were evaluated in the form of the Constant Score and the Visual Analogue Scale (VAS).
Statistics
All data were reported as median (minimum–maximum), and analyzed by means of descriptive statistics with use of SPSS (Version 14.0, Chicago, USA). Comparison between the two groups was performed with the use of the Mann-Whitney U test. The level of significance was set at p = 0.05.
Results
Patients data, baseline demographics and fracture types are were shown in Table 1.
There were no statistically significant differences between the two groups regarding age, gender and number of fracture fragments. All proximal humeral fractures except one in group II (patient No. 14: additive pertrochanteric fracture) were isolated injuries.
Intraoperative parameters
The median duration of surgery was 75 min (range 45–182 min) in group I, and 70 min (range 40–146 min) in group II without statistical difference (p = 0.442). The image intensifier time was median 1.5 min (range 0.6–3.7 min) in group I and 1.2 min (range 0.3–2.2 min) in group II (p = 0.336). During arthroscopic evaluation of the glenohumeral joint in group I one lesion of the long bicipital tendon and three partial lesions of the SSP were diagnosed and treated by a bicipital tenodesis and debridement of the SSP.
Postoperative parameters
The aim of each fracture replacement was an anatomic caput-diaphysis (CD)-angle which ranges from 130° to 140° [5]. All patients got postoperative X-rays (ap and Y-view of the injured shoulder) 2 days after surgery. The CD-angle was assessed. In group I, a median CD-angle of 137° (range 120–147°) and of 132.5° (range 120–158°) in group II was measured (p = 0.959). In group I one varus deformity with a CD-angle of 120° was observed (patient No. 5), in group II two varus deformities (CD = 120°, patient No. 10 and CD = 121°, patient No. 11), and two valgus deformities (CD = 155°, patient No. 13 and 158°, patient No. 14) were detected.
The duration of hospitalisation was median 5 days (range 4–13 days) in group I, and 6 days (range 5–18 days) in group II without any statistical significance (p = 0.130). In the time of hospitalisation one early postoperative complication occurred in the form of a N. radialis irritation in patient No. 13. (2-part + shaft spiral). No revision surgery was required.
Table 2 shows the pain score (VAS) and the first clinical results median 13 months (range, 10–18 months) postoperatively in group I, and 14 months (range, 9–21 months) postoperatively in group II. No significant differences were found in the VAS and in the, to the unaffected contralateral side, adjusted Constant Score at the time of follow-up in both groups (Table 2). One patient of each group (patients No. 8 and No. 11) showed a avascular head necrosis (partial necrosis) and secondary screw perforations with a “poor” or “satisfactory” Constant Score result.
Discussion
A general trend of minimally invasive surgical techniques in fracture treatment can be observed because of advanced arthroscopic techniques, instruments and operative skills of the surgeons. So, arthroscopic treatment of tuberosity fractures [14, 16] or implant removal [6, 17] was described.
Arthroscopic techniques in the treatment of fractures offer a lot of advantages especially for the mainly affected elderly and premorbid patient compared to the open surgery like a:
-
less peri- and postoperative morbidity,
-
minimal soft tissue trauma,
-
minimal blood loss,
-
reduced risk of postoperative infections and adhesions,
-
complete joint inspection and treatment of concomitant intraarticular injuries [17].
In the present study 4/8 (50%) of the patients in the arthroscopic group (group I) showed therapy-relevant intraarticular injuries. In a previous study, we analyzed acute proximal humeral fractures in the MRI and observed rotator cuff tears (with indication to treat) in seven of 30 patients (23%) [18]. Gallo et al. [4] described in 12 of 30 patients (40%) complete rotator cuff tears or avulsions in the context of acute proximal humeral fractures as well. This confirms the relevance of a correct diagnosis and the treatment of concomitant injuries in patients with proximal humeral fractures for a better functional outcome.
Furthermore, arthroscopic techniques take into consideration the biological aspects of the fractures, and the protection of the blood supply of the humeral head. So, a reduced number of postoperative avascular humeral head necroses, which are still a main complication of proximal humeral fractures, could be expected [12, 15, 19].
The described surgical technique allows the intramedullary nailing completely arthroscopically. The study hypothesis that the arthroscopical intramedullary nailing of proximal humeral fractures is possible, preserves the rotator cuff and provides equal replacement results like the conventional open technique was confirmed.
A sufficient and stable osteosynthesis of proximal humeral fractures with an early functional postoperative management includes all advantages of a minimally invasive procedure. The main problem of conventional antegrade humeral nailing was the impairment of the shoulder function due to the trauma of the rotator cuff at the nail insertion point [1, 8, 9, 13]. This could be decreased due to (1) an approach through the rotator interval, like described by Park et al. [13], but not suited for all implant types, or (2) due to an arthroscopic controlled mini-split in the anterior SSP for nail insertion and a subsequent side-to-side closure. The advantages of an arthroscopic rotator cuff repair over the mini-open repairs were also described previously [6, 10, 20]. Subacromial gliding layers are preserved maximally, and a pronounced subacromial scarring, which was observed after open techniques [3, 16], could be minimized by the arthroscopic surgery, as well as the trauma to the deltoid in an extended open approach. Thereby, a less postoperative patient discomfort, an early recovery of the shoulder function and good postoperative range of motion are expected. So, the intramedullary nailing as an arthroscopic procedure with a very small rotator cuff incision (1 vs. 2–3 cm in the open technique) and closure could also recommended in younger patients.
The new arthroscopic technique assures a better visual localisation of the correct nail insertion point, which is reflected in a decreased number of postoperative humeral head deformities. The preliminary data of the present study shows, no disadvantages related to the time of operation or fluoroscopy. Patients after arthroscopic nailing feel earlier comfortable in the treated shoulder in the first day after operation. This could not be reflected by a shorter time of hospitalisation, because of difficulties in the postoperative social care in case of predominantly solitarily old patients.
The short-term functional results of the arthroscopic technique were not superior to those after the conventional, open procedure.
The limits of this technique are seen in patients with adipositas per magna when the targeting device does not fit around the upper arm under arthroscopic flushing. Further, the described surgical technique is mainly suitable for surgeons who are familiar with shoulder arthroscopy.
Conclusions
All-arthroscopical humeral nailing is possible, preserves the rotator cuff and provides equal replacement and functional results like the open technique. An arthroscopically visualized optimal nail insertion point provides less frequent head deformities.
References
Blum J, Hansen M, Rommens PM (2009) Angle stable intramedullary nailing of proximal humeral fractures with the PHN (proximal humeral nail). Oper Orthop Traumatol 21(3):296–311
Codman EA (1934) Rupture of the Supraspinatus tendon and other lesions in or about the subacromial Bursa. In: Codman EA (ed) The shoulder. Thomas Todd, Boston, pp 262–293
Flinkkila T, Hyvonen P, Siira P, Hamalainen M (2004) Recovery of shoulder joint function after humeral shaft fracture: a comparative study between antegrade intramedullary nailing and plate fixation. Arch Orthop Trauma Surg 124(8):537–541
Gallo RA, Sciulli R, Daffner RH, Altman DT, Altman GT (2007) Defining the relationship between rotator cuff injury and proximal humerus fractures. Clin Orthop Rel Res 458:70–77
Ianotti J, Gabriel JP, Schneck SL, Evans BG, Misra S (1992) The normal glenohumeral relationship. J Bone Joint Surg 74-A:491–500
Kim KC, Rhee KJ, Shin HD, Kim YM (2007) Arthroscopic removal of an intramedullary nail in the humerus. Knee Surg Sports Traumatol Arthosc 15:922–926
Mathews J, Lobenhoffer P (2007) The Targon® PH Nail as an internal fixator for unstable fractures of the proximal humerus. Oper Orthop Traumatol 19:255–275
Mathews J, Lobenhoffer P (2004) Results of the provision of unstable proximal humeral fractures in geriatric patients with a new angle stabilizing antegrade nail system. Unfallchirurg 107(5):372–380 (German)
Mittlmeier TW, Stedtfeld HW, Ewert A, Beck M, Frosch B, Gradl G (2003) Stabilization of proximal humeral fractures with an angular and sliding stable antegrade locking nail (Targon PH). J Bone Joint Surg Am 85(Suppl 4):136–146
Musil D, Sadovský P (2007) Massive tears of the rotator cuff–comparison of mini-open and arthroscopic techniques. Part 2. Arthroscopic repair. Acta Chir Orthop Traumatol Cech 74(5):318–325
Nho SJ, Brophy RH, Barker JU, Cornell CN, MacGillivray JD (2007) Management of proximal humeral fractures based on current literature. J Bone Joint Surg Am 89(Suppl 3):44–58
Owsley KC, Gorczyca JT (2008) Fracture displacement and screw cutout after open reduction and locked plate fixation of proximal humeral fractures. J Bone Joint Surg Am 90(2):233–240
Park JY, Pandher DS, Chun JY, Md ST (2008) Antegrade humeral nailing through the rotator cuff interval: a new entry portal. J Orthop Trauma 22(6):419–425
Scheibel M, Martinek V, Imhoff AB (2005) Arthroscopic reconstruction of an isolated avulsion fracture. Arthroscopy 21(4):487–494
Südkamp N, Bayer J, Hepp P, Voigt C, Oestern H, Kaab M, Luo C, Plecko M, Wendt K, Kostler W, Konrad G (2009) Open reduction and internal fixation of proximal humeral fractures using the locking proximal humerus plate: results of a prospective multicenter observational study. J Bone Joint Surg Am 91(6):1320–1328
Taverna E, Sansone V, Battistella F (2004) Arthroscopic treatment for greater tuberosity fractures: rationale and surgical technique. Arthroscopy 20(6):e53–e57
Voigt C, Geisler A, Lill H (2010) Arthroscopic locking plate removal after proximal humeral fractures. Arch Orthop Trauma Surg 130(3):391–395
Voigt C, Ewig M, Vosshenrich R, Lill H (2010) Die diagnostische Wertigkeit des MRT bei proximalen Humerusfrakturen im Vergleich zur Computertomographie und konventionellem Röntgen. Unfallchirurg 113(5):378–385
Voigt C, Woltmann A, Lill H (2007) Management of complications after angulary stable locking proximal humerus plate fixation. Chirurg 78:40–46
Yamaguchi K, Levine WN, Marra G et al (2003) Transitioning to arthroscopic rotator cuff repair: the pros and cons. Instr Course Lect 52:81–92
Conflict of interest
There is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lill, H., Katthagen, C., Hertel, A. et al. All-arthroscopic intramedullary nailing of 2- and 3-part proximal humeral fractures: a new arthroscopic technique and preliminary results. Arch Orthop Trauma Surg 132, 641–647 (2012). https://doi.org/10.1007/s00402-011-1430-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-011-1430-2