Abstract
The incidence of proximal humeral fractures increases. The locking plate osteosynthesis is a standard procedure to treat displaced proximal humeral fractures. In the mostly affected elderly patients with an osteoporotic bone structure, complication rate is still high. An implant removal is commonly required. But also younger patients often request for hardware removal. The open implant removal with a subacromial and subdeltoideal arthrolysis is an extensive secondary surgery for the patients. We present a new technique to remove a locking plate from the proximal humerus arthroscopically with all advantages of the minimally invasive surgery, and the possibility to treat concomitant intraarticular pathologies parallelly.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The proximal humeral fracture is a typical fracture of the elderly patient. The demographic trend will cause a threefold incidence in 2030 [4]. Because of the osteoporotic bone structure, the treatment of displaced proximal humeral fractures is a challenge [7]. Open reduction and internal fixation is usually recommended in displaced proximal humeral fractures [1, 5, 7, 10, 12]. A lot of fixation techniques are described [7]. Locking plate fixation is a well-established surgical option with predominantly good results [5, 12]. Nevertheless, complication rates are still high (up to 76%) [1, 2, 5, 8, 10, 12]. Primary (up to 8%) or secondary screw perforations (up to 8%) (Fig. 1a, b), secondary displacement and sintering of the osteoporotic bone (up to 25%), implant impingement in case of malpositioning (up to 6%), or a restricted range of motion are the main complication-types which indicates a screw, or implant removal [1, 5, 8, 10, 12]. Furthermore, plate extraction can be performed at the request of patients without any complications. The previously used open implant removal with a subacromial and subdeltoideal arthrolysis is an extensive secondary surgery for the affected patient. We present here a novel technique to remove a locking plate from the proximal humerus arthroscopically.
Surgical technique
The arthroscopic procedure is performed under general anesthesia with the patient in beach chair position. Initially, range of motion of the affected glenohumeral joint is checked.
The portals used are the posterior, the anteroinferior and the anterolateral standard portals, as well as three portals at the lateral proximal humerus directly in the lane of the plate (Fig. 2). The surface landmark for the posterior portal is the posterior “soft spot”. Arthroscope is maintained in the posterior portal during the whole operation. Under direct vision anteroinferior standard portal is placed superior to the subscapularis tendon for instrumental passage. A standard diagnostic arthroscopy was performed to detect and treat intraarticular, concomitant pathologies of the primary proximal humeral fracture like partial lesions of the rotator cuff or long biceps tendon, and chondral lesions. If necessary, displaced tuberosity fragments can be abraded (Fig. 3), and an arthrolysis adjusted to the limits of motion can be performed subacromial and periglenoidal.
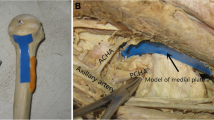
Then, arthroscope is changed in the subacromial space, and an anterolateral portal is created directly inferior to the lateral margin of the acromion 1 cm posterior of the anterior acromial edge. Subacromial bursectomy is performed until superior margin of the plate can be defined. The plate is debrided with a shaver, electrodissection or a small rasparatorium (Figs. 4, 5) close to the plate. It is essential to remove soft tissue from screw-head-cones with a small hook to provide a good grip of the screwdriver. Then, under abduction and rotation of the arm by an assistant, the proximal head screws, except the calcar screws, have to be positioned directly below the anterolateral portal, so that they can take out with a small-fragment-screwdriver through this portal (Fig. 6). It is very important to pay attention to the correct screw direction to avoid losing of the screws in the soft tissue. If the locking screws are fused in the plate, a left-hand-thread with a long hand-holder must be used.
For calcar- and shaft-screw-removal, three extra small skin incisions are performed on the lateral proximal humerus after localizing the optimal height by a needle: one incision for the calcar screws and two incisions exactly between two adjacent shaft-screws. Subcutaneous tissue is spread with a clamp, and shaft-screws are removed. Subsequently, scar tissue and adhesions are divided around the plate with a shaver, electrodissection or rasparatorium carefully. If necessary, ossifications around the margin of the plate can be eliminated by a small chisel over the anterolateral portal. In the same fashion, the plate can be underrided and lifted (Fig. 7). Then, the anterolateral portal has to be enlarged to 2 cm, and the plate is extracted through this portal with a hook (Fig. 8). Finally, the six small skin incisions are closed and sterile bandage applied. A postsurgery radiograph is made to document the complete implant removal. Posttreatment is early functional without limitations.
Discussion
A general trend of minimally invasive surgical techniques in fracture treatment can be observed because of advanced arthroscopic techniques, instruments and operative skills of the surgeon. So minimally invasive applications of a plate to the proximal humerus [9], or arthroscopic treatment of greater tuberosity-fractures [11] were described.
The arthroscopic locking plate removal is a successful innovation in the treatment of proximal humeral fractures and their concomitant complications. Because of the well-known problems with osteoporotic fractures and locking plates, the rate of implant removal constitutes 6–9% [1, 5, 8, 12]. The main causes were mentioned above.
Recently, the functional short-term outcome following removal of locking plate fixation of the proximal humerus was evaluated [6]. Patients with hardware related subacromial impingement, persisting rotation deficit, and with request for hardware removal showed a significant increase of the Constant Score 6 months after open plate removal from 66.2 ± 25.2% preoperatively to 84.3 ± 20.6% postoperatively [6].
Compared to the open surgery, the described arthroscopic technique offers a lot of advantages particularly for the mainly affected elderly and premorbid patient:
-
less peri- and postoperative morbidity,
-
minimal soft tissue trauma,
-
minimal blood loss,
-
reduced risk of postoperative infections or adhesions,
-
complete glenohumeral inspection and treatment of concomitant intraarticular injuries.
In terms of relevant concomitant intraarticular pathologies of proximal humeral fractures, we observed rotator cuff tears with therapy relevance in magnetic resonance imaging in 7 of 30 patients (23%). Gallo et al. [3] even described in 12 of 30 patients (40%) complete rotator cuff tears or avulsions in this context. Furthermore, approximately 15% of our patients with proximal humeral fractures stabilized with a locking plate showed a restricted range of motion and needed an operative arthrolysis. In up to 9% relevant tuberosity malpositions are described [5, 10, 12] with an indication for tuberculoplasty. The arthroscopy is the optimal procedure to address those concomitant injuries and to perform an intraarticular and subacromial arthrolysis before plate removal by using the same portals.
The limits of this technique are seen in patients with adipositas per magna, locking plates, which are implanted several years ago and covered from massive ossifications, or some fused locking screws, which cannot be grasped by a left-hand thread.
We conclude that arthroscopic plate removal after proximal humeral fractures is a useful innovation, which offers all advantages of a minimally invasive surgical procedure to the patient. The described technique is recommended for all surgeons familiar with arthroscopic surgery.
References
Agudelo J, Schürmann M, Stahel P, Helwig P, Morgan SJ, Zechel W et al (2007) Analysis of efficacy and failure in proximal humerus fractures treated with locking plates. J Orthop Trauma 21(10):676–681. doi:10.1097/BOT.0b013e31815bb09d
Fankhauser F, Boldin C, Schippinger G, Haunschmid C, Szyszkowitz R (2005) A locking plate for unstable fractures of the proximal humerus. Clin Orthop Relat Res 430:176–181. doi:10.1097/01.blo.0000137554.91189.a9
Gallo RA, Sciulli R, Daffner RH, Altman DT, Altman GT (2007) Defining the relationship between rotator cuff injury and proximal humerus fractures. Clin Orthop Relat Res 458:70–77
Kannus P, Palvanen M, Niemi S, Parkkari J, Järvinen M, Vuori I (2000) Osteoporotic fractures of the proximal humerus in elderly Finnish persons: sharp increase in 1970–1998 and alarming projections for the new millennium. Acta Orthop Scand 71(5):465–470. doi:10.1080/000164700317381144
Kettler M, Biberthaler P, Braunstein V, Zeiler C, Kroetz M, Mutschler W (2006) Treatment of proximal humeral fractures with the PHILOS angular stable plate. Presentation of 225 cases of dislocated fractures. Unfallchirurg 109(12):1032–1040. doi:10.1007/s00113-006-1165-7
Kirchhoff C, Braunstein V, Kirchhoff S, Sprecher CM, Ockert B, Fischer F et al (2008) Outcome analysis following removal of locking plate fixation of the proximal humerus. BMC Musculoskelet Disord 9:138. doi:10.1186/1471-2474-9-138
Nho SJ, Brophy RH, Barker JU, Cornell CN, MacGillivray JD (2007) Management of proximal humeral fractures based on current literature. J Bone Joint Surg Am 89(Suppl 3):44–58. doi:10.2106/JBJS.G.00648
Owsley KC, Gorczyca JT (2008) Fracture displacement and screw cutout after open reduction and locked plate fixation of proximal humeral fractures. J Bone Joint Surg Am 90(2):233–240. doi:10.2106/JBJS.F.01351
Röderer G, Abouelsoud M, Gebhard F, Böckers TM, Kinzl L (2007) Minimally invasive application of the non-contact-bridging (NCB) plate to the proximal humerus: an anatomical study. J Orthop Trauma 21(9):621–627. doi:10.1097/BOT.0b013e318157f0cd
Südkamp N, Bayer J, Hepp P, Voigt C, Oestern H, Kaab M, Luo C, Plecko M, Wendt K, Kostler W, Konrad G (2009) Open reduction and internal fixation of proximal humeral fractures using the locking proximal humerus plate—results of a prospective multicenter observational study. J Bone Joint Surg Am (accepted)
Taverna E, Sansone V, Battistella F (2004) Arthroscopic treatment for greater tuberosity fractures: rationale and surgical technique. Arthroscopy 20(6):e53–e57. doi:10.1016/j.arthro.2004.04.072
Voigt C, Woltmann A, Partenheimer A, Lill H (2007). Management of complications after angularly stable locking proximal humerus plate fixation. Chirurg 78(1):40–46. doi:10.1007/s00104-006-1241-0
Conflict of interest statement
There is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Voigt, C., Geisler, A. & Lill, H. Arthroscopic locking plate removal after proximal humeral fractures. Arch Orthop Trauma Surg 130, 391–395 (2010). https://doi.org/10.1007/s00402-009-0882-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-009-0882-0