Abstract
Purpose
To report our experience with antegrade short locked intramedullary nail for treatment of proximal humeral fractures and to review the current literature.
Materials and methods
From January 2012 to July 2013, 41 patients affected by two and three-part proximal humeral fractures were treated with surgical internal fixation with short locked intramedullary nails. Outcome analysis included standard clinical follow-up, Constant shoulder score and plain radiographs. The mean follow-up was 30 months (range 24–42). Moreover, a review of the literature was carried out.
Results
The mean Constant shoulder score was 81.5, excellent functional outcomes in 24/38 patients. All the fractures healed in an average time of 3.7 months. Five patients underwent additional operations, complications included hardware penetration into the joint (n = 2), backed out screw (n = 1), shoulder impingement due to protrusion of the nail (n = 2) and superficial infection (n = 1). The literature review showed 530 patients affected by proximal humeral fracture and treated with intramedullary nail with mean age of 65 years, mean follow-up of 22.2 months and a Constant shoulder score of 72.9 points; the major complications reported were backing out of the screws, shoulder impingement and joint protrusion of the screws.
Conclusions
Antegrade short locked intramedullary nail allows stable fixation, minimal soft tissue dissection, early mobilization of the shoulder and good outcomes. It is an efficacious therapeutic solution for 2- and 3-part proximal humeral fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The majority of proximal humeral fractures are osteoporosis related, affect elderly women and are the result of low-energy falls [1,2,3].
Over the decades, there have been increasing number of osteoporotic fractures with the aging of the population and represent a considerable problem in health care due to severe consequences in terms of morbidity and mortality [4].
Proximal humeral fractures represent approximately 5% of all fractures and are the third most common fracture type in the elderly population; they are associated with increased mortality in men and risk of a subsequent hip fracture more than five times within one year [1, 5, 6].
Treatment of osteoporosis and prevention of falls in elderly population should decrease the frequency of these fractures [7].
A recent study carried out by Kathib et al. [8] showed that the incidence of proximal humeral fractures in patients aged 65 or older increased by 28% between 1990 and 2010; however, not all studies demonstrated the same rapid increase [9].
The management of patients changes according to age, case history, clinical evaluation, bone mineral quality, comorbidities such as obesity [10] and patient’s ability to participate in rehabilitation.
The hospitalization rate described ranges from 36.6 to 43% [3, 11]; furthermore, Zhang et al. described a hospital readmission of 14% after surgical treatment, 75% associated with medical diagnosis [12].
The treatment of these fractures remains still controversial, and consensus in the literature is poor [9]; indications depend on the personality of the fracture, patient’s factors and surgical factors [13].
Several classification methods have been developed in order to analyze the personality of the fractures [14,15,16,17,18].
Neer and AO classifications are the most commonly used despite neither of them showing a sufficient reproducibility [19].
Approximately, 80% of these fractures can be treated non-operatively with good outcomes [20], and on the other hand, adult or active elderly patients affected by displaced fractures may require surgical treatment [21, 22].
A fracture is considered displaced if the fragments are displaced more than 1 cm or there is an angulation of more than 45°. Conservative treatment of these fractures may result in malunion and stiffness of the shoulder [15].
The potential humeral head perfusion after an intracapsular fracture is an essential issue; the predictive factors of humeral head ischemia after intracapsular fracture, as described by Hertel et al. in 2004, are: length of the dorsomedial metaphyseal extension, integrity of the medial hinge, basic fracture type [17].
Nowadays, several meta-analyses emphasize the role of the conservative treatment in elderly patients even in displaced fractures, thanks to the results being as good as the ones of the surgical treatment with the advantage of the absence of postoperative complications [23, 24].
Nevertheless, in the last decade the rate of surgical treatment increased significantly [8, 9].
Different procedures have been developed: minimally invasive techniques, open reduction and plate fixation, intramedullary nailing and arthroplasty.
The aim of this retrospective study and literature review is to investigate the functional outcome, union and complication rates in patients with 2- and 3-part proximal humeral fractures treated using antegrade short locked intramedullary nail.
Materials and methods
From January 2012 to July 2013, 63 patients with proximal humeral fractures were treated with intramedullary nail at the Department of Orthopaedics, University of Cagliari; we included in this study 41 of 63 patients.
Inclusion criteria were 2- and 3-part proximal humeral fractures according to Neer classification [15].
We excluded 22 of 63 patients treated with intramedullary nail and affected by 4-part fractures, proximal fractures with shaft extension and open fractures.
In the 41 patients included in the study, the mean age was 70 years (range 60–88); the group was composed of 26 women and 15 men, and 17 of them had fractures on the dominant side.
In 36 cases, the injury was the result of an accidental fall from standing height.
A clinical assessment was performed in all patients, fractures were evaluated with X-ray trauma series of shoulder (antero-posterior, axillary and scapular Y view), and CT scans were performed in 32 cases in order to get more details regarding the characteristics of the displacement and fracture fragments.
Fractures were classified according to Neer classification, 2-part fractures (n = 26) and 3-part fractures (n = 15), and according to AO classification: 1.1-A2 (n = 12), 1.1-A3 (n = 14), 1.1-B1 (n = 11), 1.1-B2 (n = 4).
The mean time between admission and surgery was 3 days (range 1–7), and the average operating time was 60 min (range 40–95).
A total of 35 of 41 procedures were performed by three expert surgeons, and six procedures were performed by four other surgeons supervised.
All patients were positioned in a beach-chair position. We performed the trans-deltoid approach: The skin incision, from the border of the acromion, was parallel to the humeral axis. Paying particular attention to the axillary nerve, we split the deltoid muscle and then incised the supraspinatus tendon in line with its fibers.
In all cases, we used short humeral nail with proximal and distal locking screws: Citieffe Dinamic T (Citieffe, Bologna, Italy), Expert (Synthes, West Chester, PA, USA).
In 10/41 cases, we performed the proximal fixation using the spiral blade locked with an end cap.
During the postoperative 4 weeks, patients used a shoulder sling as comfortable; early elbow mobilization and pendulum exercises were allowed, and complete external rotation and abduction movements were avoided.
Clinic assessment and X-rays (anterior–posterior and lateral projections) were performed during follow-up at 1, 3, 6 and 12 months and every 6 months thereafter.
The Constant shoulder score were assessed at the final follow-up.
We considered Constant score excellent (100–81), good (80–61), sufficient (60–41) and insufficient (40–0).
The fracture was considered healed when there was cortical bridging of at least three out of four cortices in two X-rays projections.
Finally, we reviewed the current literature reporting the use of intramedullary nail in proximal humeral fractures; we analyzed number and mean age of patients, types of fractures according to Neer classification, functional outcomes with Constant shoulder score and complications.
Results
The mean follow-up period was 30 months (range 24–42 months).
One patient had died (cause unrelated to the surgery), and two patients were lost at the time of follow-up; therefore, our initial group lowered from 41 to 38 patients.
The mean time of fracture consolidation was 3, 7 months (range 2.5–4.3), and only one fracture consolidated after 4 months, while no cases presented nonunion of the humeral head.
The average score obtained according to the Constant shoulder score was 81.5 (range 27–100) (Table 1); twenty-four patients had an excellent result (100–81), ten had good result (80–61), two sufficient (60–41), two insufficient (40–0).
Six patients (6/38) (15.8%) showed complications, and five (5/38) (13.1%) underwent another operation.
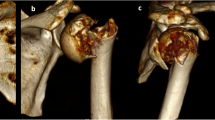
Spiral blades penetration into the articular surface of the humeral head was noticed in two patients, and two cases showed a subacromial impingement due to the nail protrusion (Fig. 1a, b: Subacromial impingement due to nail protrusion); one backed out screw and a superficial infection healed after antibiotics and wound debridement.
No cases presented avascular necrosis of the humeral head, malunion, deep infections, vascular or nervous injuries.
Our literature review revealed 15 studies (three prospective and 12 retrospective) with a total of 634 patients, where 530 of them available for the final follow-up [25,26,27,28,29,30,31,32,33,34,35,36,37,38,39] (Table 2).
Despite the variety of classification methods used in these studies, we considered only Neer classification of fracture, Constant score to assess clinical the outcomes, mean time of fracture healing, complications and reoperation rate.
The average number of patient participants in the studies selected was 35.3 (range 19–80), and the mean age was 65 years (range 48–78), the mean follow-up 22.2 months (range 10–42.8); according to Neer classification, 281 (51.1%) were 2-part fractures, 178 (32.5%) 3-part fractures, 58 (10.6%) 4-part fractures and 32 (5.8%) fractures with shaft extension.
We found an average Constant shoulder score of 72.9 (range 60.6–93.3) and a reoperation rate of 18.6% (range 0–33.3%).
Only six studies described a mean time of fractures union, and the average was 3.16 months (range 2.4–4.2).
Two studies showed significantly worst outcomes in elderly patients (> 60 years) [32, 33]; in five studies, worst outcomes were described in 4-part-type fractures [25, 28, 31, 36, 37].
The most reported complications are: backing out of the screws (n = 42), shoulder impingement (n = 31), screw protrusion into the shoulder joint (n = 21) and avascular necrosis (n = 20) (Table 3).
Discussion
Many authors obtained good results using the intramedullary nail, especially in 1.1-A2, 1.1-A3, 1.1-B1, 1.1-B2 fractures (AO classification), and 2- and 3-part fractures (Neer classification).
Our series considered the small number of patients, showed a better Constant shoulder score (81.5 vs 72.8) and less reoperation rate than our review (13.5% vs 18.6%), and this may be due to the absence of 4-part fractures and to the exclusion of proximal fractures with shaft extension [25,26,27,28,29,30,31,32,33,34,35,36,37,38,39].
The advantages of intramedullary nail reported were: stable fixation, less bleeding, less invasive surgery, close reduction in fracture, less vascular nerve injuries, shorter time of surgery and quick functional rehabilitation [25,26,27,28,29,30,31,32,33,34,35,36,37,38,39].
On the other hand, the disadvantages reported were: imperfect anatomical reduction, worst stability in fractures with more than two fragments, rotator cuff lesion, increased exposure to X-ray and subacromial impingement due to nail protrusion.
A systematic review performed by Wong et al. in 2015 [40] studied the outcome in 448 patients diagnosed with humeral head fracture treated with intramedullary nail. The mean age was 64.3 years, and the mean Constant score was 72.8 and was significantly higher in 2- and 3-part fractures. The reoperation rate for 2-, 3- and 4-part fractures was 13.6, 17.4 and 63.2%, respectively; therefore, the authors do not recommend the use of intramedullary nail in 4-part fractures.
The comparison between the intramedullary nailing and the ORIF with plate and screws in proximal humeral fractures still remains controversial.
Wang et al. [41] in 2015 carried out a meta-analysis using two randomized controlled trials, two prospective and four retrospective studies, showing that nailing and plating are both valuable options for 2-, 3- and 4-part fractures.
Zhu et al. [38] performed a prospective randomized study that compared locking intramedullary nails and locking plates in the treatment of 2-part fractures.
The locking nail group had a significantly lower complication rate compared to the locking plate group; and after three years, no significant difference was found between the locking nail and locking plate groups in terms of ASES score, Constant score and strength of the supraspinatus muscle.
Baltov et al. [42] and Owsley et al. [43] showed that both intramedullary nail and plate and screws fixation have high rate of complications.
Blum et al. [44] described, in a multicenter study, 48 complications in 113 patients treated by intramedullary nail; 63% of these complications were surgery related, and this study revealed that in the majority of cases a weak operative technique was responsible for treatment failure.
Two of the main problems reported after humeral intramedullary nailing are the poor range of movement due to rotator cuff lesions in entrance point of the nail and subacromial impingement caused by a nail not correctly inserted.
As aforementioned, there are no significant differences between plate and nail in proximal humeral fracture, whereas with humeral shaft fractures several studies carried out between 2006 and 2015 demonstrated the superiority of plate fixation on intramedullary nailing.
As Bhandari et al. [45] explained in 2006 with lack of cumulative evidence, Zhao et al. [46] demonstrated that plate is the gold standard in humeral shaft fractures. They did not find differences between nail and plate in terms of fracture union, radial nerve injury and infection, but intramedullary nail increased the risk of shoulder complications (shoulder impingement and restriction of movements) and reoperation.
In our experience, the difference between the results in proximal humerus fracture and humeral shaft is unclear. The presence of a cuff tear associated with a proximal humeral fracture occurred more frequently in complex fractures and in older patients, and it seems to decrease functional outcome and even improve skeletal deterioration [47, 48].
The debate concerning the lesion after the splitting of the supraspinatus muscle, used to introduce the intramedullary nail, remains open.
Gierer et al. [49] conducted a study on 15 patients affected by proximal humeral fractures; they used the orthogonal polarization spectral imaging technique to evaluate the vascular perfusion of the supraspinatus tendon and they found that, after the humeral nailing, the functional capillary density was reduced by about half; this effect seems to be transitional, but the authors recommended a careful tendon split.
Verdano et al. [50] demonstrated with ultrasonographic studies that anterolateral approach for humeral nailing did not cause significant alteration to the rotator cuff and did not affect long-term outcomes.
Gracitelli et al. [51] found, with ultrasound evaluation, 32% of partial and 13% of full thickness cuff tears in patients treated with antegrade nail for proximal humerus fractures; nevertheless, cuff tears detected did not affect clinical outcomes.
The strength of our study was to analyze our experience and the current literature; nevertheless, it has several limitations: The small sample size and the absence of a control group randomized did not allow a statistical analysis.
Conclusions
The results of this study suggest that antegrade short intramedullary nail is a valid treatment for patients affected by proximal humeral fractures 1-1-A2, 1-1-A3, 1-1-B1, 1-1-B2 according to AO classification, and 2- and 3-part according to Neer classification.
This device allows minimally invasive procedures, early shoulder mobilization and good outcome. Complications are frequent, but the majority of those are avoidable if a correct indication and a good surgical technique are used.
References
Court-Brown CM, Caesar B (2006) Epidemiology of adult fractures: a review. Injury 37(8):691–697
Court-Brown CM, Garg A, McQueen MM (2001) The epidemiology of proximal humeral fractures. Acta Orthop Scand 72(4):365–371
Roux A, Decroocq L, El Batti S, Bonnevialle N, Moineau G, Trojani C et al (2012) Epidemiology of proximal humerus fractures managed in a trauma center. OrthopTraumatolSurg Res 98(6):715–719
Holroyd C, Cooper C, Dennison E (2008) Epidemiology of osteoporosis. Best Pract Res Clin Endocrinol Metab 22(5):671–685
Piirtola M, Vahlberg T, Löppönen M, Räihä I, Isoaho R, Kivelä SL (2008) Fractures as predictors of excess mortality in the aged-a population-based study with a 12-year follow-up. Eur J Epidemiol 23(11):747–755
Clinton J, Franta A, Polissar NL, Neradilek B, Mounce D, Fink HA et al (2009) Proximal humeral fracture as a risk factor for subsequent hip fractures. J Bone Joint Surg Am 91(3):503–511
Chu SP, Kelsey JL, Keegan TH, Sternfeld B, Prill M, Quesenberry CP et al (2004) Risk factors for proximal humerus fracture. Am J Epidemiol 160(4):360–367
Khatib O, Onyekwelu I, Zuckerman JD (2014) The incidence of proximal humeral fractures in New York State from 1990 through 2010 with an emphasis on operative management in patients aged 65 years or older. J Shoulder Elbow Surg 23(9):1356–1362
Bell JE, Leung BC, Spratt KF, Koval KJ, Weinstein JD, Goodman DC et al (2011) Trends and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. J Bone Joint Surg Am 93(2):121–131
Werner BC, Griffin JW, Yang S, Brockmeier SF, Gwathmey FW (2015) Obesity is associated with increased postoperative complications after operative management of proximal humerus fractures. J Shoulder Elbow Surg 24:593–600
Tarantino U, Capone A, Planta M, D’Arienzo M, Letizia Mauro G, Impagliazzo A et al (2010) The incidence of hip, forearm, humeral, ankle, and vertebral fragility fractures in Italy: results from a 3-year multicenter study. Arthritis Res Ther 12(6):R226
Zhang AL, Schairer WW, Feeley BT (2014) Hospital readmissions after surgical treatment of proximal humerus fractures: is arthroplasty safer than open reduction internal fixation? Clin Orthop Relat Res 472:2317–2324
Murray IR, Amin AK, White TO, Robinson CM (2011) Proximal humeral fractures: current concepts in classification, treatment and outcomes. J Bone Joint Surg Br 93(1):1–11
Gumina S, Rita A, Arceri V, Postacchini F (2009) Fractures of the proximal humerus: incidence and classification. Lo Scalpello 23:2–7
Neer CS II (1970) Displaced proximal humeral fractures. Classification and evaluation. J Bone Joint Surg Am 52:1077–1089
Müller M (1988) Proximal humerus fracture: AO classification. Manual of internal fixation, pp 118–125
Hertel R, Hempfing A, Stiehler M, Leunig M (2004) Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elbow Surg 13:427–433
Edelson G, Kelly I, Vigder F, Reis ND (2004) A three-dimensional classification for fractures of the proximal humerus. J Bone Joint Surg Br 86(3):413–425
Siebenrock KA, Gerber C (1993) The reproducibility of classification of fractures of the proximal end of the humerus. J Bone Joint Surg Am 75(12):1751–1755
Gaebler C, McQueen MM, Court-Brown CM (2003) Minimally displaced proximal humeral fractures: epidemiology and outcome in 507 cases. Acta Orthop Scand 74(5):580–585
Gerber C, Werner CM, Vienne P (2004) Internal fixation of complex fractures of the proximal humerus. J Bone Joint Surg Br 86(6):848–855
Marongiu G, Mastio M, Capone A (2013) Current options to surgical treatment in osteoporotic fractures. Aging Clin Exp Res 25(Suppl 1):S15–S17. https://doi.org/10.1007/s40520-013-0081-2
Xie L, Ding F, Zhao Z, Chen Y, Xing D (2015) Operative versus non-operative treatment in complex proximal humeral fractures: a meta-analysis of randomized controlled trials. Springerplus 25(4):728
Rabi S, Evaniew N, Sprague SA, Bhandari M, Sloboge GP (2015) Operative vs non-operative management of displaced proximal humeral fractures in the elderly: a systematic review and meta-analysis of randomized controlled trials. World J Orthop 6(10):838–846
Sosef N, van Leerdam R, Ott P, Meylaerts S, Rhemrev S (2010) Minimal invasive fixation of proximal humeral fractures with an intramedullary nail: good results in elderly patients. Arch Orthop Trauma Surg 130(5):605–611
Rajasekhar C, Ray PS, Bhamra MS (2001) Fixation of proximal humeral fractures with the Polarus nail. J Shoulder Elbow Surg 10(1):7–10
Popescu D, Fernandez-Valencia JA, Rios M, Cuñé J, Domingo A, Prat S (2009) Internal fixation of proximal humerus fractures using the T2-proximal humeral nail. Arch Orthop Trauma Surg 129(9):1239–1244
Kumar V, Datir S, Venkateswaran B (2010) Intramedullary nailing for displaced proximal humeral fractures. J Orthop Surg (Hong Kong) 18(3):324–327
Iacobellis C, Serafini D, Aldegheri R (2009) PHN for treatment of proximal humerus fractures: evaluation of 80 cases. Chir Organi Mov 93(2):47–56
Hatzidakis AM, Shevlin MJ, Fenton DL et al (2011) Angular-stable locked intramedullary nailing of two-part surgical neck fractures of the proximal part of the humerus. A multicenter retrospective observational study. J Bone Joint Surg Am 93(23):2172–2179
Gradl G, Dietze A, Arndt D, Beck M, Gierer P, Börsch T, Mittlmeier T (2007) Angular and sliding stable antegrade nailing (Targon PH) for the treatment of proximal humeral fractures. Arch Orthop Trauma Surg 127(10):937–944
Giannoudis PV, Xypnitos FN, Dimitriou R, Manidakis N, Hackney R (2012) Internal fixation of proximal humeral fractures using the Polarus intramedullary nail: our institutional experience and review of the literature. J Orthop Surg Res 19(7):39
Fazal MA, Baloch I, Ashwood N (2014) Polarus nail fixation for proximal humeral fractures. J Orthop Surg (Hong Kong) 22(2):195–198
Konrad G, Audigé L, Lambert S, Hertel R, Südkamp NP (2012) Similar outcomes for nail versus plate fixation of three-part proximal humeral fractures. Clin Orthop Relat Res 470:602–609
Agel J, Jones CB, Sanzone AG, Camuso M, Henley MB (2004) Treatment of proximal humeral fractures with Polarus nail fixation. J Shoulder Elbow Surg 13(2):191–195
Adedapo AO, Ikpeme JO (2001) The results of internal fixation of three- and four-part proximal humeral fractures with the Polarus nail. Injury 32(2):115–121
Boudard G, Pomares G, Milin L, Lemonnier I (2014) Locking plate fixation versus antegrade nailing of 3- and 4-part proximal humerus fractures in patients without osteoporosis. Comparative retrospective study of 63 cases. Orthop Traumatol Surg Res 100(8):917–924
Zhu Y, Lu Y, Shen J, Zhang J, Jiang C (2011) Locking intramedullary nails and locking plates in the treatment of two-part proximal humeral surgical neck fractures: a prospective randomized trial with a minimum of three years of follow-up. J Bone Joint Surg Am 93(2):159–168
Nobile F, Carta S, Fortina M, Santoro P, Meccariello L, Ferrata P (2016) Displaced 3- and 4-part proximal humeral fractures: evaluation and management with an intramedullary nail within 48 h, in the emergency department. J Acute Dis 5(2):154–159
Wong J, Newman JM, Gruson KI (2015) Outcomes of intramedullary nailing for acute proximal humerus fractures: a systematic review. J Orthop Traumatol 17:113–122
Wang G, Mao Z, Zhang L, Zhang L, Zhao Y, Yin P et al (2015) Meta-analysis of locking plate versus intramedullary nail for treatment of proximal humeral fractures. J Orthop Surg Res 15(10):122
Baltov A, Mihail R, Dian E (2014) Complications after interlocking intramedullary nailing of humeral shaft fractures. Injury 45(Suppl 1):S9–S15
Owsley KC, Gorczyca JT (2008) Fracture displacement and screw cutout after open reduction and locked plate fixation of proximal humeral fractures. J Bone Joint Surg Am 90:233–240
Blum J, Hansen M, Muller M, Rommens PM et al (2009) Proximal humeral fractures and intramedullary nailing: experience with a new nail system. Eur J Trauma Emerg Surg 35(5):489–498
Bhandari M, Devereaux PJ, McKee MD, Schemitsch EH (2006) Compression plating versus intramedullary nailing of humeral shaft fractures—a meta-analysis. Acta Orthop 77(2):279–284
Zhao JG, Wang J, Wang C, Kan SL (2015) Intramedullary nail versus plate fixation for humeral shaft fractures: a systematic review of overlapping meta-analyses. Medicine 94:11
Bahrs C, Rolauffs B, Stuby F, Dietz K, Weise K, Helwig P (2010) Effect of proximal humeral fractures on the age-specific prevalence of rotator cuff tears. J Trauma 69(4):901–906
Fjalestad T, Hole MØ, Blücher J, Hovden IA, Stiris MG, Strømsøe K (2010) Rotator cuff tears in proximal humeral fractures: an MRI cohort study in 76 patients. Arch Orthop Trauma Surg 130(5):575–581
Gierer P, Scholz M, Beck M, Schaser KD, Vollmar B, Mittlmeier T et al (2010) Microcirculatory sequelae of the rotator cuff after antegrade nailing in proximal humerus fracture. Arch Orthop Trauma Surg 130(5):687–691
Verdano MA, Pellegrini A, Schiavi P, Somenzi L, Concari G, Ceccarelli F (2013) Humeral shaft fractures treated with antegrade intramedullary nailing: what are the consequences for the rotator cuff? Int Orthop 37(10):2001–2007
Gracitelli MEC, Malavolta EA, Assuncao JH, Matsumura BA, Kojima KE, Neto AAF (2017) Ultrasound evaluation of the rotator cuff after osteosynthesis of proximal humeral fractures with locking intramedullary nail. Rev Bras Orthop. 52(5):601–607
Acknowledgements
The authors are grateful to Dr. Marco Verona and Dr. Adriano Demurtas (Clinica Ortopedica, Università degli studi di Cagliari, Italy) for professional support (essential surgical and clinical activity).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the ethics committee of the Department of Surgical Science of the University of Cagliari.
Human and animal rights
The retrospective observational study included in this paper involved Human Participants.
Informed consent
Informed consent was obtained from all individual participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Congia, S., Palmas, A., Marongiu, G. et al. Is antegrade nailing a proper option in 2- and 3-part proximal humeral fractures?. Musculoskelet Surg 104, 179–185 (2020). https://doi.org/10.1007/s12306-019-00610-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-019-00610-5