Abstract
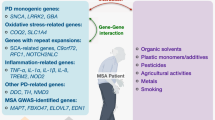
Recent advances in the molecular pathology and genetics of multiple system atrophy (MSA) indicate that the disease involves plural pathogenic mechanisms. The determination of the morphological spectrum of MSA using quantitative pathological analysis points to the need for further investigation to determine the population-bound phenotype distribution of MSA. These notions support the hypothesis that a spectrum of genetic susceptibility factors underlies MSA pathogenesis. A possibly effective strategy for determining this genetic susceptibility spectrum is to perform an association study of important genes for neurodegenerative diseases, which are prevalent in a population, using linkage disequilibrium mapping in MSA patients with well-characterized morphological phenotypes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple system atrophy (MSA) is an adult-onset neurodegenerative disease that clinically presents with various combinations of parkinsonism, cerebellar ataxia and autonomic failure [26, 70]. MSA is characterized pathologically by glial (oligodendroglial) cytoplasmic inclusions (GCIs) [52, 65], which are immunopositive for α-synuclein [45, 76, 90] and other minor proteins. Biochemical evidence suggests that oxidative and nitrative alterations of α-synuclein protein [2, 16, 24, 59, 60, 68] contribute to MSA pathogenesis. Epidemiologic evidence suggests that certain environmental toxins are associated with the increased risk of MSA [12, 29, 53, 87, 88]. Genetic background is also an important factor for MSA pathogenesis, because most neurodegenerative diseases have familial forms that have facilitated linkage studies leading to the discovery of pathogenic genes. However, family-based linkage studies of the genes responsible for MSA are impossible because this disease is usually sporadic and there are very few families reported to have MSA [75, 97]. Therefore, progress in the determination of genetic susceptibility factors is more likely to come from association studies of candidate genes in large MSA cohorts. These studies should be conducted taking into account the observation that there is a spectrum of pathological involvement of the striatonigral (SN) and olivopontocerebellar (OPC) regions in MSA [63]. In this review, we discuss recent advances in the molecular pathology and genetics of MSA, and propose a possibly effective strategy for determining the spectrum of genetic susceptibility factors to clarify MSA pathogenesis.
Molecular pathology of multiple system atrophy
The development of extensive GCIs in the central nervous system is a characteristic pathological feature of MSA (Fig. 1). GCIs contain a filamentous structure that can be recognized by an antibody against α-synuclein [45, 76, 90]. This discovery has lead to biochemical evidence showing that the major component of GCIs is abnormally misfolded, relatively insoluble α-synuclein [10, 46, 85], which is heavily coated with an amorphous material [21]. Oxidative and nitrative alterations play a major role in the modification of α-synuclein [2, 16, 24, 59, 60, 68], and this possibly causes the dysregulation of cellular processes. Moreover, α-synuclein interestingly has a synergistic action with τ-protein, which is another important molecule for neurodegerative diseases (reviewed in [22, 93]). However, α-synuclein is a neuronal protein that is transiently expressed only in developing but not mature oligodendrocytes [14, 71]. Moreover, there is no increase in the level of α-synuclein mRNA in MSA brains [62] or GCI-bearing oligodendrocytes [47]. Therefore, the origin of α-synuclein in GCIs and the mechanism by which GCIs are formed remain to be elucidated.
The brain specific protein tubulin polymerization promoting protein (TPPP/p25) is a strong marker of GCIs [41, 43]. The aggregation of α-synuclein is also associated with rab3, which is a member of the Ras super family of small GTP-binding proteins [15]. The protein 14-3-3 also accumulates in GCIs [25, 38, 40]. 14-3-3 is a chaperon protein that regulates various types of signal transduction pathway through a phosphorylation-dependent protein–protein interaction [18]. Interestingly, 14-3-3 and α-synuclein are also involved in the development of cytoplasmic inclusions, which are generated by the overexpression of trinucleotide CAG repeat stretches of the huntingtin gene [89]. Heat shock protein 90 has been reported to play a major role in the formation of α-synuclein aggregates in GCIs [86]. Of note, the Parkinson’s disease (PD)-associated protein DJ-1 is also involved in the formation of GCIs [54]. Finally, a variety of other molecules that abundantly exist in the central nervous system are involved in the formation of GCIs (reviewed in [94]).
MSA also induces the formation of inclusion bodies in the neurons of the inferior olivary nucleus, pontine nucleus, putamen and occasionally in the cerebral cortex [3, 5, 56, 63, 66, 100]; however, the role of these inclusion bodies in the induction of neuronal degeneration is not yet fully understood. Neuronal cytoplasmic inclusions (NCIs) in the pontine nucleus and putamen appear as round or ovoid homogenous or skeinlike structures, occupying a large area of the neuronal cytoplasm, whereas those in the inferior olivary nucleus are irregular in shape [4, 56, 72]. The major component of NCIs is also modified α-synuclein [55]; however, some NCIs are reported to have immunoreactivity for p25α, but none for α-synuclein [6]. Neuronal intranuclear inclusions (NNIs) are composed of densely packed, granulofilamentous structures [56]. The presence of both NCIs and NNIs in some neurons has occasionally been observed. A quantitative investigation of NCIs and NNIs in 14 MSA cases showed that NCI formation is accelerated by the progression of the disease process, and that NNI formation occurs earlier than NCI formation [56]. Further investigation is needed to elucidate whether NCI and NNI formations are the primary events that govern MSA pathogenesis.
Accumulating genetic evidence of multiple system atrophy
From the molecular pathology of GCI formation, the α-synuclein gene has become the most probable gene responsible for MSA pathogenesis. However, a genetic analysis of pathologically confirmed MSA cases failed to find any pathogenic mutations in the α-synuclein gene [50, 64]. Moreover, a case-control association study using a haplotype tagging approach showed that multiple regions in the α-synuclein gene are not associated with MSA pathogenesis [61], whereas they are associated with a sporadic cause of PD [51]. Likewise, other genes such as those of apolipoprotein E [9, 49, 50], τ [49, 50], dopamine β-hydroxylase [11, 31], ubiquitin C-terminal hydrolase-1 [32], fragile × mental retardation 1 [8, 23, 37, 98], and leucine-rich kinase 2 [33] showed no association with MSA pathogenesis. Several genes associated with the inflammatory process were studied with regard to MSA pathogenesis. Several studies indicate that polymorphisms of interleukin-1A [13], interleukin-1B [57], interleukin-8 [34], and intercellular adhesion molecule-1 genes [34] are associated with an increased risk of MSA. Another study demonstrated the association between a polymorphism of the α-1-antichymotrypsin gene and the risk of MSA [19]. Moreover, the promoter region polymorphism in the tumor necrosis factor gene has also been reported to be associated with the risk of MSA [58]. Further studies with much larger cohorts are needed to confirm these findings.
Several MSA patients have relatives with PD [95]. MSA and PD have similarities at the molecular level, i.e., the accumulation of α-synuclein protein aggregates, namely, GCIs in MSA [90] and Lewy bodies in PD [77], indicates that similar pathogenic mechanisms are involved in these two disorders. However, a case control study demonstrated that a family history of PD is not a risk factor for MSA [88]. Therefore, the association between MSA pathogenesis and the genetic susceptibility factors of PD remains to be elucidated. Interestingly, patients with sporadic PD are associated with certain haplotypes or genotypes of the τ gene [17, 30, 44, 67], which plays a crucial role in the pathogenesis of other neurodegenerative parkinsonian syndromes, such as progressive supranuclear palsy and corticobasal degeneration. Endeavors to find MSA patients who have relatives with PD or other neurodegenerative parkinsonian syndromes are needed to clarify the genetic background of MSA.
Plural pathogenic mechanisms of multiple system atrophy
Growing evidence suggests that oligodendrocytic synucleinopathy underlies MSA pathogenesis. Morphological analyses of pathologically confirmed MSA cases showed significant correlations between the frequency of GCIs and the severity of neuronal degeneration [35, 63]. An apoptotic cell death mechanism exists in oligodendrocytes but not in the neurons of MSA patients [69]. The mouse model of MSA showed that the overexpression of α-synuclein in oligodendrocytes results in neuronal degeneration in the central nervous system [73, 78, 99]. These findings indicate that the GCI formation contributes markedly to neuronal degeneration, and plays a central role in MSA pathogenesis. However, the question is whether GCIs always induce neuronal degeneration in every vulnerable region in patients with MSA. A recent neuropathological study using a novel pathological index called the ‘neuronal cell loss predominance score’ demonstrated that neuronal degeneration is always severe, whereas the appearance of GCIs is mild in the substantia nigra [63]. These findings indicate that neurodegeneration in the substantia nigra is not simply influenced by the accumulation of oligodendroglial α-synuclein aggregates. Furthermore, the study also demonstrated that the density of GCIs in the SN region is significantly lower than that in the OPC region [63]. From these observations, it is tempting to hypothesize that GCI formation is the cause of primary lesions in the OPC region, but not in the SN region, and also that factors other than GCIs contribute to the neurodegenerative process in the SN region.
The formation of NCIs is another cytopathological feature of MSA in which filamentous α-synuclein aggregates; however, the frequency of NCIs is not associated with a particular MSA morphological phenotype [63], and whether NCI formation primarily causes neuronal degeneration remains to be clarified. Moreover, the Purkinje cell layer in the cerebellum, which is severely affected in MSA, has no NCIs in its remaining Purkinje cells [48, 63]. The absence of NCIs suggests that the Purkinje cells are not involved in the pathogenic mechanism associated with α-synuclein aggregation, but they are highly vulnerable to oligodendroglial dysfunction owing to GCI formation. Neurons in the substantia nigra have incidental Lewy bodies [84], which appear in only 10% of MSA cases [63]; however, there are no MSA-specific NCIs in the remaining neurons in the substantia nigra. The absence of NCIs in the substantia nigra is presumably associated with rapid neuronal degeneration in this area [63]. This notion points to the need for further investigation to elucidate whether the neurons in the substantia nigra of MSA patients have an innate cell death mechanism.
Possibility of population-bound phenotype distribution
In a series of 100 MSA cases, 34% were striatonigral degeneration (SND)-predominant, 17% were olivopontocerebellar atrophy (OPCA)-predominant, and 49% had equivalent SND and OPCA pathologies [63]. This study also indicates that MSA with predominant parkinsonism (MSA-P) and MSA with predominant cerebellar ataxia (MSA-C) are clinical and pathological phenotypes that may represent different ends of a spectrum. Because selection bias is a crucial factor when the percentages of MSA-P and MSA-C cases are compared between populations, a future comparative morphological study using a similar approach for determining the percentages of MSA-P and MSA-C cases is needed. However, clinical evidence from retrospective case note reviews raises the possibility that MSA-P is relatively more frequent than MSA-C among Caucasians [92]. On the other hand, MSA-C may exist more frequently in the Japanese population [79, 91]. Likewise, it is suggested that in the Chinese population, MSA-C is relatively more frequent than MSA-P [36]. These findings support the hypothesis that there is a population-bound phenotype distribution of MSA (Fig. 2). It is reasonable to speculate that the subsets of biological factors, which are responsible for the vulnerability of neurons in the SN or OPC region, determine this difference in the emphasis of pathological phenotypes between populations. A combination of genetic factors is likely to underlie such vulnerability of neurons that differs between the SN and OPC regions in MSA.
Hypothesis on spectrum of genetic susceptibility factors in multiple system atrophy
A genetic approach should be carried out taking into account the notion that there is a spectrum of pathological involvement of the SN and OPC regions, and a possible population-bound phenotype distribution of MSA. Moderate genetic effects caused by a subset of certain genotypes, which are prevalent in a population, may influence the population-bound phenotype distribution of MSA. MSA is genetically distinct from inherited causes of spinocerebellar degeneration [7]. However, some cases of dominantly inherited spinocerebellar ataxia (SCA) have been reported to exhibit parkinsonism [20, 28, 74, 96], autonomic failure [81], and phenocopies of MSA [27, 39, 42]. For SCA cases, the relative prevalence of genotypes differs between Caucasians and Japanese; SCA1 and SCA2 are prevalent in Caucasians, whereas SCA3, SCA6, and dentatorubural pallidoluysian atrophy are prevalent in Japanese [80]. Interestingly, the frequency of normal alleles with a relatively large number of CAG repeats is also associated with the prevalence of these SCA genotypes [80]. For inherited causes of PD, genetic studies of different ethnicities show that mutations of the leucine-rich kinase 2 and DJ-1 are rare in the Asian population [82, 83]. These endeavors to determine the relative prevalence of genotypes that differs between populations may help elucidate the genetic susceptibility factors in MSA pathogenesis. Unlike effective strategies using Mendelian genetics, those for detecting moderate genetic effects in populations have been problematic, and a combination of techniques is recommended [1]. For MSA, it is likely that the linkage disequilibrium mapping of some important genes for neurodegenerative diseases, which are prevalent in a population, can be used for large MSA cohorts in which the morphological spectrum is well characterized [61]. This strategy is formulated on the basis of the hypothesis that there are different subsets of genetic susceptibility factors that are responsible for different ends of a spectrum such as MSA-P and MSA-C (Fig. 3). Hence, genetics based on pathology could be an effective approach to determining the spectrum of genetic susceptibility factors in MSA pathogenesis.
References
Abou-Sleiman PM, Healy DG, Wood NW (2004) Genetic approaches to solving common diseases. J Neurol 251:1169–1172
Andrekopoulos C, Zhang H, Joseph J, Kalivendi S, Kalyanaraman B (2004) Bicarbonate enhances alpha-synuclein oligomerization and nitration: intermediacy of carbonate radical anion and nitrogen dioxide radical. Biochem J 378:435–447
Arima K, Murayama S, Mukoyama M, Inose T (1992) Immunocytochemical and ultrastructural studies of neuronal and oligodendroglial cytoplasmic inclusions in multiple system atrophy. 1. Neuronal cytoplasmic inclusions. Acta Neuropathol (Berl) 83:453–460
Arima K, Ueda K, Sunohara N, Arakawa K, Hirai S, Nakamura M, Tonozuka-Uehara H, Kawai M (1998) NACP/alpha-synuclein immunoreactivity in fibrillary components of neuronal and oligodendroglial cytoplasmic inclusions in the pontine nuclei in multiple system atrophy. Acta Neuropathol (Berl) 96:439–444
Armstrong RA, Lantos PL, Cairns NJ (2005) Multiple system atrophy: laminar distribution of the pathological changes in frontal and temporal neocortex—a study in ten patients. Clin Neuropathol 24:230–235
Baker KG, Huang Y, McCann H, Gai WP, Jensen PH, Halliday GM (2006) P25alpha immunoreactive but alpha-synuclein immunonegative neuronal inclusions in multiple system atrophy. Acta Neuropathol (Berl) 111:193–195
Bandmann O, Sweeney MG, Daniel SE, Wenning GK, Quinn N, Marsden CD, Wood NW (1997) Multiple-system atrophy is genetically distinct from identified inherited causes of spinocerebellar degeneration. Neurology 49:1598–1604
Biancalana V, Toft M, Le Ber I, Tison F, Scherrer E, Thibodeau S, Mandel JL, Brice A, Farrer MJ, Durr A (2005) FMR1 premutations associated with fragile X-associated tremor/ataxia syndrome in multiple system atrophy. Arch Neurol 62:962–966
Cairns NJ, Atkinson PF, Kovacs T, Lees AJ, Daniel SE, Lantos PL (1997) Apolipoprotein E e4 allele frequency in patients with multiple system atrophy. Neurosci Lett 221:161–164
Campbell BC, McLean CA, Culvenor JG, Gai WP, Blumbergs PC, Jakala P, Beyreuther K, Masters CL, Li QX (2001) The solubility of alpha-synuclein in multiple system atrophy differs from that of dementia with Lewy bodies and Parkinson’s disease. J Neurochem 76:87–96
Cho S, Kim CH, Cubells JF, Zabetian CP, Hwang DY, Kim JW, Cohen BM, Biaggioni I, Robertson D, Kim KS (2003) Variations in the dopamine beta-hydroxylase gene are not associated with the autonomic disorders, pure autonomic failure, or multiple system atrophy. Am J Med Genet A 120:234–236
Chrysostome V, Tison F, Yekhlef F, Sourgen C, Baldi I, Dartigues JF (2004) Epidemiology of multiple system atrophy: a prevalence and pilot risk factor study in Aquitaine, France. Neuroepidemiology 23:201–208
Combarros O, Infante J, Llorca J, Berciano J (2003) Interleukin-1A (-889) genetic polymorphism increases the risk of multiple system atrophy. Mov Disord 18:1385–1386
Culvenor JG, Rietze RL, Bartlett PF, Masters CL, Li QX (2002) Oligodendrocytes from neural stem cells express alpha-synuclein: increased numbers from presenilin 1 deficient mice. Neuroreport 13:1305–1308
Dalfo E, Ferrer I (2005) Alpha-synuclein binding to rab3a in multiple system atrophy. Neurosci Lett 380:170–175
Duda JE, Giasson BI, Chen Q, Gur TL, Hurtig HI, Stern MB, Gollomp SM, Ischiropoulos H, Lee VM, Trojanowski JQ (2000) Widespread nitration of pathological inclusions in neurodegenerative synucleinopathies. Am J Pathol 157:1439–1445
Farrer M, Skipper L, Berg M, Bisceglio G, Hanson M, Hardy J, Adam A, Gwinn-Hardy K, Aasly J (2002) The tau H1 haplotype is associated with Parkinson’s disease in the Norwegian population. Neurosci Lett 322:83–86
Fu H, Subramanian RR, Masters SC (2000) 14-3-3 proteins: structure, function, and regulation. Annu Rev Pharmacol Toxicol 40:617–647
Furiya Y, Hirano M, Kurumatani N, Nakamuro T, Matsumura R, Futamura N, Ueno S (2005) Alpha-1-antichymotrypsin gene polymorphism and susceptibility to multiple system atrophy (MSA). Brain Res Mol Brain Res 138:178–181
Furtado S, Payami H, Lockhart PJ, Hanson M, Nutt JG, Singleton AA, Singleton A, Bower J, Utti RJ, Bird TD, de la Fuente-Fernandez R, Tsuboi Y, Klimek ML, Suchowersky O, Hardy J, Calne DB, Wszolek ZK, Farrer M, Gwinn-Hardy K, Stoessl AJ (2004) Profile of families with parkinsonism-predominant spinocerebellar ataxia type 2 (SCA2). Mov Disord 19:622–629
Gai WP, Pountney DL, Power JH, Li QX, Culvenor JG, McLean CA, Jensen PH, Blumbergs PC (2003) Alpha-synuclein fibrils constitute the central core of oligodendroglial inclusion filaments in multiple system atrophy. Exp Neurol 181:68–78
Galpern WR, Lang AE (2006) Interface between tauopathies and synucleinopathies: a tale of two proteins. Ann Neurol 59:449–458
Garland EM, Vnencak-Jones CL, Biaggioni I, Davis TL, Montine TJ, Robertson D (2004) Fragile X gene premutation in multiple system atrophy. J Neurol Sci 227:115–118
Giasson BI, Duda JE, Murray IV, Chen Q, Souza JM, Hurtig HI, Ischiropoulos H, Trojanowski JQ, Lee VM (2000) Oxidative damage linked to neurodegeneration by selective alpha-synuclein nitration in synucleinopathy lesions. Science 290:985–989
Giasson BI, Mabon ME, Duda JE, Montine TJ, Robertson D, Hurtig HI, Lee VM, Trojanowski JQ (2003) Tau and 14-3-3 in glial cytoplasmic inclusions of multiple system atrophy. Acta Neuropathol (Berl) 106:243–250
Gilman S, Low PA, Quinn N, Albanese A, Ben-Shlomo Y, Fowler CJ, Kaufmann H, Klockgether T, Lang AE, Lantos PL, Litvan I, Mathias CJ, Oliver E, Robertson D, Schatz I, Wenning GK (1999) Consensus statement on the diagnosis of multiple system atrophy. J Neurol Sci 163:94–98
Gilman S, Sima AA, Junck L, Kluin KJ, Koeppe RA, Lohman ME, Little R (1996) Spinocerebellar ataxia type 1 with multiple system degeneration and glial cytoplasmic inclusions. Ann Neurol 39:241–255
Gwinn-Hardy K, Chen JY, Liu HC, Liu TY, Boss M, Seltzer W, Adam A, Singleton A, Koroshetz W, Waters C, Hardy J, Farrer M (2000) Spinocerebellar ataxia type 2 with parkinsonism in ethnic Chinese. Neurology 55:800–805
Hanna PA, Jankovic J, Kirkpatrick JB (1999) Multiple system atrophy: the putative causative role of environmental toxins. Arch Neurol 56:90–94
Healy DG, Abou-Sleiman PM, Lees AJ, Casas JP, Quinn N, Bhatia K, Hingorani AD, Wood NW (2004) Tau gene and Parkinson’s disease: a case-control study and meta-analysis. J Neurol Neurosurg Psychiatry 75:962–965
Healy DG, Abou-Sleiman PM, Ozawa T, Lees AJ, Bhatia K, Ahmadi KR, Wullner U, Berciano J, Moller JC, Kamm C, Burk K, Barone P, Tolosa E, Quinn N, Goldstein DB, Wood NW (2004) A functional polymorphism regulating dopamine beta-hydroxylase influences against Parkinson’s disease. Ann Neurol 55:443–446
Healy DG, Abou-Sleiman PM, Quinn N, Ahmadi KR, Ozawa T, Kamm C, Wullner U, Oertel WH, Burk K, Dupont E, Pellecchia MT, Tolosa E, Gasser T, Holton JL, Revesz T, Goldstein DB, Lees AJ, Wood NW (2005) UCHL-1 gene in multiple system atrophy: a haplotype tagging approach. Mov Disord 20:1338–1343
Hernandez D, Paisan Ruiz C, Crawley A, Malkani R, Werner J, Gwinn-Hardy K, Dickson D, Wavrant Devrieze F, Hardy J, Singleton A (2005) The dardarin G 2019 S mutation is a common cause of Parkinson’s disease but not other neurodegenerative diseases. Neurosci Lett 389:137–139
Infante J, Llorca J, Berciano J, Combarros O (2005) Interleukin-8, intercellular adhesion molecule-1 and tumour necrosis factor-alpha gene polymorphisms and the risk for multiple system atrophy. J Neurol Sci 228:11–13
Inoue M, Yagishita S, Ryo M, Hasegawa K, Amano N, Matsushita M (1997) The distribution and dynamic density of oligodendroglial cytoplasmic inclusions (GCIs) in multiple system atrophy: a correlation between the density of GCIs and the degree of involvement of striatonigral and olivopontocerebellar systems. Acta Neuropathol (Berl) 93:585–591
Jamora RD, Gupta A, Tan AK, Tan LC (2005) Clinical characteristics of patients with multiple system atrophy in Singapore. Ann Acad Med Singapore 34:553–557
Kamm C, Healy DG, Quinn NP, Wullner U, Moller JC, Schols L, Geser F, Burk K, Borglum AD, Pellecchia MT, Tolosa E, del Sorbo F, Nilsson C, Bandmann O, Sharma M, Mayer P, Gasteiger M, Haworth A, Ozawa T, Lees AJ, Short J, Giunti P, Holinski-Feder E, Illig T, Wichmann HE, Wenning GK, Wood NW, Gasser T (2005) The fragile X tremor ataxia syndrome in the differential diagnosis of multiple system atrophy: data from the EMSA study group. Brain 128:1855–1860
Kawamoto Y, Akiguchi I, Nakamura S, Budka H (2002) Accumulation of 14-3-3 proteins in glial cytoplasmic inclusions in multiple system atrophy. Ann Neurol 52:722–731
Khan NL, Giunti P, Sweeney MG, Scherfler C, Brien MO, Piccini P, Wood NW, Lees AJ (2005) Parkinsonism and nigrostriatal dysfunction are associated with spinocerebellar ataxia type 6 (SCA6). Mov Disord 20:1115–1119
Komori T, Ishizawa K, Arai N, Hirose T, Mizutani T, Oda M (2003) Immunoexpression of 14-3-3 proteins in glial cytoplasmic inclusions of multiple system atrophy. Acta Neuropathol (Berl) 106:66–70
Kovacs GG, Laszlo L, Kovacs J, Jensen PH, Lindersson E, Botond G, Molnar T, Perczel A, Hudecz F, Mezo G, Erdei A, Tirian L, Lehotzky A, Gelpi E, Budka H, Ovadi J (2004) Natively unfolded tubulin polymerization promoting protein TPPP/p25 is a common marker of alpha-synucleinopathies. Neurobiol Dis 17:155–162
Lee WY, Jin DK, Oh MR, Lee JE, Song SM, Lee EA, Kim GM, Chung JS, Lee KH (2003) Frequency analysis and clinical characterization of spinocerebellar ataxia types 1, 2, 3, 6, and 7 in Korean patients. Arch Neurol 60:858–863
Lindersson E, Lundvig D, Petersen C, Madsen P, Nyengaard JR, Hojrup P, Moos T, Otzen D, Gai WP, Blumbergs PC, Jensen PH (2005) p25alpha Stimulates alpha-synuclein aggregation and is co-localized with aggregated alpha-synuclein in alpha-synucleinopathies. J Biol Chem 280:5703–5715
Martin ER, Scott WK, Nance MA, Watts RL, Hubble JP, Koller WC, Lyons K, Pahwa R, Stern MB, Colcher A, Hiner BC, Jankovic J, Ondo WG, Allen FH Jr, Goetz CG, Small GW, Masterman D, Mastaglia F, Laing NG, Stajich JM, Ribble RC, Booze MW, Rogala A, Hauser MA, Zhang F, Gibson RA, Middleton LT, Roses AD, Haines JL, Scott BL, Pericak-Vance MA, Vance JM (2001) Association of single-nucleotide polymorphisms of the tau gene with late-onset Parkinson disease. JAMA 286:2245–2250
Mezey E, Dehejia A, Harta G, Papp MI, Polymeropoulos MH, Brownstein MJ (1998) Alpha synuclein in neurodegenerative disorders: murderer or accomplice? Nat Med 4:755–757
Miake H, Mizusawa H, Iwatsubo T, Hasegawa M (2002) Biochemical characterization of the core structure of alpha-synuclein filaments. J Biol Chem 277:19213–19219
Miller DW, Johnson JM, Solano SM, Hollingsworth ZR, Standaert DG, Young AB (2005) Absence of alpha-synuclein mRNA expression in normal and multiple system atrophy oligodendroglia. J Neural Transm 112:1613–1624
Mori F, Piao YS, Hayashi S, Fujiwara H, Hasegawa M, Yoshimoto M, Iwatsubo T, Takahashi H, Wakabayashi K (2003) Alpha-synuclein accumulates in Purkinje cells in Lewy body disease but not in multiple system atrophy. J Neuropathol Exp Neurol 62:812–819
Morris HR, Schrag A, Nath U, Burn D, Quinn NP, Daniel S, Wood NW, Lees AJ (2001) Effect of ApoE and tau on age of onset of progressive supranuclear palsy and multiple system atrophy. Neurosci Lett 312:118–120
Morris HR, Vaughan JR, Datta SR, Bandopadhyay R, Rohan De Silva HA, Schrag A, Cairns NJ, Burn D, Nath U, Lantos PL, Daniel S, Lees AJ, Quinn NP, Wood NW (2000) Multiple system atrophy/progressive supranuclear palsy: alpha-Synuclein, synphilin, tau, and APOE. Neurology 55:1918–1920
Mueller JC, Fuchs J, Hofer A, Zimprich A, Lichtner P, Illig T, Berg D, Wullner U, Meitinger T, Gasser T (2005) Multiple regions of alpha-synuclein are associated with Parkinson’s disease. Ann Neurol 57:535–541
Nakazato Y, Yamazaki H, Hirato J, Ishida Y, Yamaguchi H (1990) Oligodendroglial microtubular tangles in olivopontocerebellar atrophy. J Neuropathol Exp Neurol 49:521–530
Nee LE, Gomez MR, Dambrosia J, Bale S, Eldridge R, Polinsky RJ (1991) Environmental-occupational risk factors and familial associations in multiple system atrophy: a preliminary investigation. Clin Auton Res 1:9–13
Neumann M, Muller V, Gorner K, Kretzschmar HA, Haass C, Kahle PJ (2004) Pathological properties of the Parkinson’s disease-associated protein DJ-1 in alpha-synucleinopathies and tauopathies: relevance for multiple system atrophy and Pick’s disease. Acta Neuropathol (Berl) 107:489–496
Nishie M, Mori F, Fujiwara H, Hasegawa M, Yoshimoto M, Iwatsubo T, Takahashi H, Wakabayashi K (2004) Accumulation of phosphorylated alpha-synuclein in the brain and peripheral ganglia of patients with multiple system atrophy. Acta Neuropathol (Berl) 107:292–298
Nishie M, Mori F, Yoshimoto M, Takahashi H, Wakabayashi K (2004) A quantitative investigation of neuronal cytoplasmic and intranuclear inclusions in the pontine and inferior olivary nuclei in multiple system atrophy. Neuropathol Appl Neurobiol 30:546–554
Nishimura M, Kawakami H, Komure O, Maruyama H, Morino H, Izumi Y, Nakamura S, Kaji R, Kuno S (2002) Contribution of the interleukin-1beta gene polymorphism in multiple system atrophy. Mov Disord 17:808–811
Nishimura M, Kuno S, Kaji R, Kawakami H (2005) Influence of a tumor necrosis factor gene polymorphism in Japanese patients with multiple system atrophy. Neurosci Lett 374:218–221
Norris EH, Giasson BI (2005) Role of oxidative damage in protein aggregation associated with Parkinson’s disease and related disorders. Antioxid Redox Signal 7:672–684
Norris EH, Giasson BI, Ischiropoulos H, Lee VM (2003) Effects of oxidative and nitrative challenges on alpha-synuclein fibrillogenesis involve distinct mechanisms of protein modifications. J Biol Chem 278:27230–27240
Ozawa T, Healy DG, Abou-Sleiman PM, Ahmadi KR, Quinn N, Lees AJ, Shaw K, Wullner U, Berciano J, Moller JC, Kamm C, Burk K, Josephs KA, Barone P, Tolosa E, Goldstein DB, Wenning G, Geser F, Holton JL, Gasser T, Revesz T, Wood NW (2006) The {alpha}-synuclein gene in multiple system atrophy. J Neurol Neurosurg Psychiatry 77:464–467
Ozawa T, Okuizumi K, Ikeuchi T, Wakabayashi K, Takahashi H, Tsuji S (2001) Analysis of the expression level of alpha-synuclein mRNA using postmortem brain samples from pathologically confirmed cases of multiple system atrophy. Acta Neuropathol (Berl) 102:188–190
Ozawa T, Paviour D, Quinn NP, Josephs KA, Sangha H, Kilford L, Healy DG, Wood NW, Lees AJ, Holton JL, Revesz T (2004) The spectrum of pathological involvement of the striatonigral and olivopontocerebellar systems in multiple system atrophy: clinicopathological correlations. Brain 127:2657–2671
Ozawa T, Takano H, Onodera O, Kobayashi H, Ikeuchi T, Koide R, Okuizumi K, Shimohata T, Wakabayashi K, Takahashi H, Tsuji S (1999) No mutation in the entire coding region of the alpha-synuclein gene in pathologically confirmed cases of multiple system atrophy. Neurosci Lett 270:110–112
Papp MI, Kahn JE, Lantos PL (1989) Glial cytoplasmic inclusions in the CNS of patients with multiple system atrophy (striatonigral degeneration, olivopontocerebellar atrophy and Shy-Drager syndrome). J Neurol Sci 94:79–100
Papp MI, Lantos PL (1992) Accumulation of tubular structures in oligodendroglial and neuronal cells as the basic alteration in multiple system atrophy. J Neurol Sci 107:172–182
Pastor P, Ezquerra M, Munoz E, Marti MJ, Blesa R, Tolosa E, Oliva R (2000) Significant association between the tau gene A0/A0 genotype and Parkinson’s disease. Ann Neurol 47:242–245
Paxinou E, Chen Q, Weisse M, Giasson BI, Norris EH, Rueter SM, Trojanowski JQ, Lee VM, Ischiropoulos H (2001) Induction of alpha-synuclein aggregation by intracellular nitrative insult. J Neurosci 21:8053–8061
Probst-Cousin S, Rickert CH, Schmid KW, Gullotta F (1998) Cell death mechanisms in multiple system atrophy. J Neuropathol Exp Neurol 57:814–821
Quinn N (1989) Multiple system atrophy–the nature of the beast. J Neurol Neurosurg Psychiatry (Suppl):78–89
Richter-Landsberg C, Gorath M, Trojanowski JQ, Lee VM (2000) Alpha-synuclein is developmentally expressed in cultured rat brain oligodendrocytes. J Neurosci Res 62:9–14
Sakurai A, Okamoto K, Yaguchi M, Fujita Y, Mizuno Y, Nakazato Y, Gonatas NK (2002) Pathology of the inferior olivary nucleus in patients with multiple system atrophy. Acta Neuropathol (Berl) 103:550–554
Shults CW, Rockenstein E, Crews L, Adame A, Mante M, Larrea G, Hashimoto M, Song D, Iwatsubo T, Tsuboi K, Masliah E (2005) Neurological and neurodegenerative alterations in a transgenic mouse model expressing human alpha-synuclein under oligodendrocyte promoter: implications for multiple system atrophy. J Neurosci 25:10689–10699
Simon-Sanchez J, Hanson M, Singleton A, Hernandez D, McInerney A, Nussbaum R, Werner J, Gallardo M, Weiser R, Gwinn-Hardy K, Singleton AB, Clarimon J (2005) Analysis of SCA-2 and SCA-3 repeats in Parkinsonism: evidence of SCA-2 expansion in a family with autosomal dominant Parkinson’s disease. Neurosci Lett 382:191–194
Soma H, Yabe I, Takei A, Fujiki N, Yanagihara T, Sasaki H (2006) Heredity in multiple system atrophy. J Neurol Sci 240:107–110
Spillantini MG, Crowther RA, Jakes R, Cairns NJ, Lantos PL, Goedert M (1998) Filamentous alpha-synuclein inclusions link multiple system atrophy with Parkinson’s disease and dementia with Lewy bodies. Neurosci Lett 251:205–208
Spillantini MG, Schmidt ML, Lee VM, Trojanowski JQ, Jakes R, Goedert M (1997) Alpha-synuclein in Lewy bodies. Nature 388:839–840
Stefanova N, Reindl M, Neumann M, Haass C, Poewe W, Kahle PJ, Wenning GK (2005) Oxidative stress in transgenic mice with oligodendroglial alpha-synuclein overexpression replicates the characteristic neuropathology of multiple system atrophy. Am J Pathol 166:869–876
Tada M, Ozawa T, Onodera O, Tada M, Piao YS, Takahashi H, Nishizawa M (2004) Clinical features of 49 pathologically proven patients with multiple system atrophy in the Japanese population (abstract). In: 8th International congress of Parkinson’s disease and movement disorders, Rome, Italy
Takano H, Cancel G, Ikeuchi T, Lorenzetti D, Mawad R, Stevanin G, Didierjean O, Durr A, Oyake M, Shimohata T, Sasaki R, Koide R, Igarashi S, Hayashi S, Takiyama Y, Nishizawa M, Tanaka H, Zoghbi H, Brice A, Tsuji S (1998) Close associations between prevalences of dominantly inherited spinocerebellar ataxias with CAG-repeat expansions and frequencies of large normal CAG alleles in Japanese and Caucasian populations. Am J Hum Genet 63:1060–1066
Takiyama Y, Sakoe K, Nakano I, Nishizawa M (1997) Machado-Joseph disease: cerebellar ataxia and autonomic dysfunction in a patient with the shortest known expanded allele (56 CAG repeat units) of the MJD1 gene. Neurology 49:604–606
Tan EK, Shen H, Tan LC, Farrer M, Yew K, Chua E, Jamora RD, Puvan K, Puong KY, Zhao Y, Pavanni R, Wong MC, Yih Y, Skipper L, Liu JJ (2005) The G2019S LRRK2 mutation is uncommon in an Asian cohort of Parkinson’s disease patients. Neurosci Lett 384:327–329
Tan EK, Tan C, Zhao Y, Yew K, Shen H, Chandran VR, Teoh ML, Yih Y, Pavanni R, Wong MC (2004) Genetic analysis of DJ-1 in a cohort Parkinson’s disease patients of different ethnicity. Neurosci Lett 367:109–112
Tison F, Wenning GK, Daniel SE, Quinn NP (1995) Multiple system atrophy with Lewy bodies. Rev Neurol (Paris) 151:398–403
Tu PH, Galvin JE, Baba M, Giasson B, Tomita T, Leight S, Nakajo S, Iwatsubo T, Trojanowski JQ, Lee VM (1998) Glial cytoplasmic inclusions in white matter oligodendrocytes of multiple system atrophy brains contain insoluble alpha-synuclein. Ann Neurol 44:415–422
Uryu K, Richter-Landsberg C, Welch W, Sun E, Goldbaum O, Norris EH, Pham CT, Yazawa I, Hilburger K, Micsenyi M, Giasson BI, Bonini NM, Lee VM, Trojanowski JQ (2006) Convergence of heat shock protein 90 with ubiquitin in filamentous {alpha}-synuclein inclusions of {alpha}-synucleinopathies. Am J Pathol 168:947–961
Vanacore N, Bonifati V, Fabbrini G, Colosimo C, De Michele G, Marconi R, Nicholl D, Locuratolo N, Talarico G, Romano S, Stocchi F, Bonuccelli U, De Mari M, Vieregge P, Meco G (2001) Epidemiology of multiple system atrophy. ESGAP Consortium. European study group on atypical parkinsonisms. Neurol Sci 22:97–99
Vanacore N, Bonifati V, Fabbrini G, Colosimo C, De Michele G, Marconi R, Stocchi F, Nicholl D, Bonuccelli U, De Mari M, Vieregge P, Meco G (2005) Case-control study of multiple system atrophy. Mov Disord 20:158–163
Waelter S, Boeddrich A, Lurz R, Scherzinger E, Lueder G, Lehrach H, Wanker EE (2001) Accumulation of mutant huntingtin fragments in aggresome-like inclusion bodies as a result of insufficient protein degradation. Mol Biol Cell 12:1393–1407
Wakabayashi K, Yoshimoto M, Tsuji S, Takahashi H (1998) Alpha-synuclein immunoreactivity in glial cytoplasmic inclusions in multiple system atrophy. Neurosci Lett 249:180–182
Watanabe H, Saito Y, Terao S, Ando T, Kachi T, Mukai E, Aiba I, Abe Y, Tamakoshi A, Doyu M, Hirayama M, Sobue G (2002) Progression and prognosis in multiple system atrophy: an analysis of 230 Japanese patients. Brain 125:1070–1083
Wenning GK, Ben Shlomo Y, Magalhaes M, Daniel SE, Quinn NP (1994) Clinical features and natural history of multiple system atrophy. An analysis of 100 cases Brain 117(Pt 4):835–845
Wenning GK, Jellinger KA (2005) The role of alpha-synuclein and tau in neurodegenerative movement disorders. Curr Opin Neurol 18:357–362
Wenning GK, Jellinger KA (2005) The role of alpha-synuclein in the pathogenesis of multiple system atrophy. Acta Neuropathol (Berl) 109:129–140
Wenning GK, Wagner S, Daniel S, Quinn NP (1993) Multiple system atrophy: sporadic or familial? Lancet 342:681
Wilkins A, Brown JM, Barker RA (2004) SCA2 presenting as levodopa-responsive parkinsonism in a young patient from the United Kingdom: a case report. Mov Disord 19:593–595
Wullner U, Abele M, Schmitz-Huebsch T, Wilhelm K, Benecke R, Deuschl G, Klockgether T (2004) Probable multiple system atrophy in a German family. J Neurol Neurosurg Psychiatry 75:924–925
Yabe I, Soma H, Takei A, Fujik N, Sasaki H (2004) No association between FMR1 premutations and multiple system atrophy. J Neurol 251:1411–1412
Yazawa I, Giasson BI, Sasaki R, Zhang B, Joyce S, Uryu K, Trojanowski JQ, Lee VM (2005) Mouse model of multiple system atrophy alpha-synuclein expression in oligodendrocytes causes glial and neuronal degeneration. Neuron 45:847–859
Yokoyama T, Kusunoki JI, Hasegawa K, Sakai H, Yagishita S (2001) Distribution and dynamic process of neuronal cytoplasmic inclusion (NCI) in MSA: correlation of the density of NCI and the degree of involvement of the pontine nuclei. Neuropathology 21:145–154
Acknowledgments
The author was a research fellow of the Department of Molecular Neuroscience, Institute of Neurology, Queen Square, and he was a specialist clinical fellow of the National Hospital for Neurology and Neurosurgery, Queen Square, London (2002–2003). Figure 1 shows a microscopy image taken from a brain material in the Queen Square Brain Bank, London.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ozawa, T. Pathology and genetics of multiple system atrophy: an approach to determining genetic susceptibility spectrum. Acta Neuropathol 112, 531–538 (2006). https://doi.org/10.1007/s00401-006-0109-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-006-0109-1