Abstract
Multiple system atrophy (MSA) is a neurodegenerative disease characterized by the presence of glial cytoplasmic inclusions (GCIs), which are comprised of fibrils of the protein α-synuclein (α-syn). Increasing evidence indicate that the formation of these lesions leads to cellular dysfunction and degeneration. The events that result in the formation of GCIs remain poorly understood. It is possible that changes in the cytoplasmic milieu, perhaps the aberrant expression of α-syn-interacting proteins, can promote the polymerization of α-syn. The presence of the microtubule-binding protein, tau, in GCIs has been reported in some studies, but these findings have not been consistent, and these studies were performed prior to the availability of the more sensitive methods of detecting GCIs using anti-α-syn antibodies. Recently, 14-3-3 proteins, putative α-syn-interacting partners, have been reported in Lewy bodies, which also are pathological inclusions comprised of α-syn. In this study the presence of tau and 14-3-3 proteins in GCIs of 21 patients with MSA was investigated. For the majority of cases, tau and 14-3-3 proteins were detected only in a subset of GCIs. In some cases none of the GCIs contained 14-3-3 or tau. When present in GCIs, tau was in a hypophosphorylated state as demonstrated with phosphorylation-specific antibodies. α-syn fibrillogenesis without 14-3-3 or tau appears to be sufficient for GCI formation, although it is possible that the accumulation of multi-functional proteins, like 14-3-3, in GCIs contribute to the disruption of cellular homeostasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple system atrophy (MSA) is an adult onset neurodegenerative disease characterized by varying degrees of parkinsonism features, cerebellar ataxia, corticospinal dysfunction and autonomic dysfunction [73, 74], but the defining feature of MSA is the presence of glial cytoplasmic inclusions (GCIs) [52]. MSA brains show varying extent of demyelination and atrophy, especially in the cerebellum, pons, and medulla, as well as the loss of pigmented cells in the substantia nigra pars compacta [73, 74]. Previously, patients with MSA were classified under three clinical categories: olivopontocerebellar atrophy, striatonigral degeneration and Shy-Drager syndrome [28]. However, it is now widely accepted that MSA is a single disease entity and this notion has led to the consensus recommendation that the classification of patients with MSA should be simplified to MSA-C (MSA with prominent cerebellar ataxia) or MSA-P (MSA with prominent parkinsonism) depending on the relative predominance of clinical and pathological abnormalities [26].
GCIs are found in oligodendrocytes and they can have a flame-, triangular-, or sickle-shaped appearance [52]. GCIs can be observed throughout the white matter, but they are more abundant in the basal ganglia, substantia nigra, pontine nucleus, medulla and cerebellum [2, 12, 39]. Ultrastructural analysis of GCIs demonstrated that they are composed of a meshwork of randomly arranged, loosely packed filaments with cross-sectional diameters of 15–30 nm [1, 34, 35, 44, 52]. Using immunological, ultrastructural and biochemical approaches, it has been demonstrated that these fibrils are predominantly comprised of polymerized α-synuclein (α-syn) [3, 11, 12, 68, 69, 70].
α-syn fibrils are also the major component of other types of pathological lesions, such as Lewy bodies (LBs) and Lewy neurites, which are defining features of Parkinson's disease (PD) and dementia with LBs (DLB) [62, 63]. Pathological inclusions comprised of α-syn are present in a spectrum of neurodegenerative disorders that are collectively referred to as α-synucleinopathies [14].
α-syn is predominantly expressed in central nervous system neurons, where it is localized mainly at presynaptic terminals [21, 31, 32, 75]. It is unclear if α-syn is normally expressed at low levels in oligodendrocytes in adult brain, but it can be detected in cultured rodent oligodendrocytes [57]. It is possible that an abnormal increase in expression of α-syn in these cells leads to the formation of GCIs, although α-syn mRNA does not seem to be increased in the white matter of MSA brains [49]. It is likely that other changes in the cytoplasmic milieu, perhaps the accumulation of α-syn-interacting proteins, must occur to promote the fibrillogenesis of α-syn. Some reports have demonstrated that the microtubule-binding protein tau, which interacts with α-syn in vitro [33], can be detected in GCIs. However, these findings are controversial since immunostaining analyses of GCIs with anti-tau antibodies have been reported to range from entirely negative [34, 44] to a substantial proportion of GCIs being labeled [1, 8, 38, 43, 51, 54, 56, 66].
Recently, it was reported that the 14-3-3 proteins are present in the majority of classical and cortical LBs in PD and DLB [36]. The 14-3-3 family of proteins is ubiquitously expressed in mammalian cells, but they are especially abundant in brain, where they account for ~1% of total soluble protein [7]. There are at least seven mammalian isoforms of 14-3-3 [7, 61], which exist as dimers, and they are thought to be adaptors that serve to modulate signal transduction pathways by preferentially binding to phosphorylated motifs [18, 61]. Notably, 14-3-3 proteins have been shown to bind to α-syn in living cells [47].
The presence of 14-3-3 and tau in GCIs was analyzed in 21 cases of MSA to determine if they were interacting proteins that might play a role in GCI formation. These proteins were found in a majority of GCIs in some brains. However, in most cases, only a minority or none of the GCIs were positive for 14-3-3 and tau, suggesting that their accumulation in GCIs is secondary to the fibrillogenesis of α-syn.
Materials and methods
Antibodies
Anti-14-3-3β (clone H-8) murine monoclonal antibody (mAb) was purchased from Santa Cruz Biotechnology (Santa Cruz, CA). Antibody 17026 is a rabbit antiserum raised against full-length recombinant tau and it detects all isoforms of tau [30]. PHF-1 [48] and PHF-6 [29] are phosphorylation-dependent mAbs that specifically react with tau phosphorylated at Ser-396/404 and Ser-231, respectively. Tau-1 is a dephosphorylation-specific mAb that recognizes an epitope within amino acid residues 189–209 in the longest isoform of tau [6, 65]. Murine anti-α-syn mAbs LB 509 and Syn 202 have been described previously [5, 23].
Cell culture
HEK293 cells were obtained from the American Type Culture Collection (Rockville, MD) and cultured in Dulbecco's modified medium-high glucose 4.5 g/l (DMEM) supplemented with 10% FBS, 100 U/ml penicillin, 100 U/ml streptomycin, and 2 mM l-glutamine. HEK 293 cells stably expressing human α-syn have been described previously [53].
Gel electrophoresis and Western blotting
Cells were harvested in phosphate-buffered saline (PBS; 137 mM NaCl, 2.7 mM KCl, 10 mM Na2HPO4, 1.8 mM KH2PO4), lysed in 2% SDS, 62.5 mM TRIS, pH 6.8, and protein concentrations were determined using the bicinchoninic acid (BCA) assay (Pierce, Rockford, IL). The cell extracts were diluted in SDS-sample buffer (10 mM TRIS, pH 6.8, 1 mM EDTA, 40 mM DTT, 1% SDS, 10% sucrose), and the proteins were resolved on slab gels by SDS-polyacrylamide gel electrophoresis. Proteins were electrophoretically transferred to nitrocellulose membranes (Schleicher and Schuell, Keene, NH) in buffer containing 48 mM TRIS, 39 mM glycine and 10% methanol. Membranes were blocked with 5% skimmed milk powder dissolved in TRIS-buffered saline-Tween (20 mM TRIS, pH 7.7, 137 mM NaCl and 0.1% Tween-20), incubated with primary antibodies followed by anti-mouse horseradish peroxidase (HRP)-conjugated antibodies and visualized by enhanced chemiluminescence as recommended by the manufacturer.
Tissue collection and processing
The harvesting, fixation and further processing of the tissue specimens studied here were conducted as previously described [12, 58]. Briefly, tissue blocks were removed at autopsy and fixed by immersion in 70% ethanol with 150 mM NaCl or 10% buffered formalin for 24–36 h. The samples were dehydrated through a series of graded ethanols to xylene at room temperature and infiltrated with paraffin at 60°C according to a previously described schedule [67]. The blocks were then cut into multiple, near serial 6-μm sections for immunohistochemical staining. The diagnostic assessment of all MSA cases was performed in accordance with published guidelines [20, 26, 42].
Immunohistochemistry
Immunohistochemistry was carried out using the avidin-biotin complex (ABC) detection system (Vector Laboratories, Burlingame, CA) and 3,3'-diaminobenzidine (DAB) as described [12]. Briefly, sections were deparaffinized and re-hydrated, endogenous peroxidases were quenched with 5% hydrogen peroxide in methanol for 30 min and sections were blocked in 0.1 M TRIS with 2% donor horse serum (TRIS/DHS) for 5 min. To try to improve antigen detection, some selected sections were pre-treated with 88% formic acid (FA) for 1 or 5 min or heated in a microwave oven for 5 min prior to treatment with hydrogen peroxide. All antibodies were diluted in TRIS/DHS. Primary antibodies were incubated overnight at 4°C. After washing, sections were sequentially incubated with species specific, biotinylated secondary antibodies for 1 h and ABC complex for 1 h. Bound antibody complexes were visualized by incubating sections in a solution containing 100 mM TRIS, pH 7.6, 0.1% Triton X-100, 1.4 mM diaminobenzidine (DAB), 10 mM imidazole and 8.8 mM hydrogen peroxide.
Evaluation of immunohistochemical data
The cerebellum and pons of MSA brains, which are rich in GCIs, were evaluated for the purpose of this study. The abundance of immunoreactive GCIs was assessed using a semi-quantitative assessment strategy, as described [12]. The regional density of immunoreactive inclusions was graded in each region as follows: 3, frequent; 2, moderate; 1, few; and 0, none. Sections were graded independently by two observers (B.I.G and M.E.M.).
Results
Specificity of 14-3-3β antibody
To study the presence of 14-3-3 proteins in GCIs, a pan-14-3-3 mAb (clone H-8) that recognizes a conserved epitope within the N terminus of 14-3-3 proteins was used. The specificity of this antibody was determined by Western blot analysis of HEK 293 cells extracts (Fig. 1). The anti-14-3-3 mAb specifically recognized a major immunoband of ~30 kDa and a less intense band with a slightly higher molecular mass, consistent with the predicted migration of 14-3-3 proteins on SDS-PAGE [18, 61]. Since 14-3-3 proteins have some sequence homology to α-syn [47], the possible cross-reactivity of this antibody with α-syn was assessed by Western blot analysis using extracts of HEK 293 cells stably overexpressing human α-syn, and this showed that α-syn was readily detected with the anti-α-syn mAb LB509, but there was no cross-reactivity of the anti-14-3-3 mAb with α-syn (Fig. 1).
Specificity of anti-14-3-3β antibody. Cell lysates (5 μg) from HEK 293 cells or HEK 293 cells stably expressing human α-syn (293/α-syn) were resolved on 13% SDS-polyacrylamide gels. Proteins were electrophoretically transferred onto nitrocellulose membranes that were probed with anti-14-3-3β mAb H-8 or anti-α-syn mAb LB509. The mobility of molecular mass markers is indicated on the left of each panel (α-syn α-synuclein, mAb monoclonal antibody)
Immunohistochemical detection of 14-3-3 and tau in GCIs
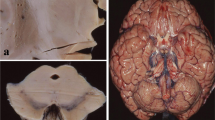
The abundance of GCIs was assessed in each MSA brain using the Syn 202 mAb (Fig. 2A), because it detected these lesions most robustly [12]. Tissue sections from the pons and cerebellum were used to determine the presence of tau and 14-3-3 in GCIs, since these regions are rich in these lesions (Table 1). In one case (case 1) there was a high proportion of GCIs that stained positive for 14-3-3 (Fig. 2B, Table 1), but in the majority of cases only a moderate or low number of GCIs were 14-3-3 positive (Table 1). There were also a few cases were no GCIs were detected with the anti-14-3-3 mAb.
Immunostaining of GCIs with antibodies to α-syn, 14-3-3 and tau. Immunolabeling of cerebellar sections of multiple system atrophy brains with antibodies Syn 202 (A), 14-3-3β (H-8) (B), 17026 (C), and Tau-1 (D). Higher magnifications of GCIs labeled with each antibody, respectively, are shown in the lower insets. Staining with PHF-6 is shown in the upper inset of D (GCI glial cytoplasmic inclusion). Bar A–D 160 μm; insets 80 μm
In a subset of MSA cases, some GCIs were immuno-detected with the anti-tau antibody 17026. This polyclonal antibody, raised against full-length recombinant human tau, was selected because it recognizes all the alternatively spliced isoforms of tau and it is phosphorylation independent [30]. There was no case where the density of tau-positive inclusions was very abundant (Table 1), although in some fields a significant number of GCIs were stained by 17026 (Fig. 2C), but in most cases infrequent or no GCIs were stained with 17026. Tau-positive inclusions were also strongly immunoreactive with the Tau-1 mAb specific for non-phosphorylated tau (Fig. 2D). Conversely, GCIs were unstained with the phosphorylation-specific antibody PHF-1 and only weakly reactive with the phosphorylation-specific antibody PHF-6 (Fig. 1D, upper inset). Antigen retrieval with FA treatment or heating in microwave oven did not enhance the staining with the anti-14-3-3 or anti-tau antibodies. In cases (e.g., case 1) where GCIs were frequently stained for 14-3-3 or tau, double-labeling analysis demonstrated that these proteins could accumulate together in GCIs. However, in most cases the major of GCIs were rarely double-labeled for 14-3-3 and tau (data not shown).
There was no direct association between the accumulation of tau in GCIs and the formation of tau inclusions in other region of the brain, such as the hippocampus. For example, cases with the most abundant tau-positive GCIs (cases 1, 3, 12 and 19) had little or sparse tau pathology in the entorhinal cortex (data not shown). Conversely, cases with abundant tau pathology in the entorhinal cortex (cases 5, 7, 17, and 20) (data not shown) had no or few tau-positive GCIs (see Table 1).
Discussion
Increasing evidence suggests that the polymerization of α-syn and the formation of pathological α-syn inclusions leads to the impairment of cellular functions and the degeneration of affected cells. For example, the pathological mutation A53T, which has been identified in at least 12 families [4, 41, 50, 55, 64], increases the propensity of α-syn to polymerize in vitro [10, 22, 45]. Although patients carrying the A53T mutation were initially diagnosed with familial PD, re-examination revealed that the distribution of α-syn pathology is significantly more widespread throughout the neuraxis than in classical idiopathic PD [13, 64]. Furthermore, the clinical presentation of affected individuals with the A53T mutation includes several features (e.g., dementia, prominent myoclonus and urinary incontinence) that are not characteristic of or common to classical idiopathic PD [27, 64]. Expression of human A53T α-syn in transgenic mice results in severe motor impairment that coincides with abundant α-syn pathological inclusions, but mice expressing equivalent levels of wild-type human α-syn do not display these impairments or pathological changes [24].
The events that result in the formation of pathological inclusions comprised of the wild-type α-syn protein remain enigmatic. It is possible that the interaction of α-syn with other proteins can induce the formation of inclusions. Here, the presence of two α-syn-interacting proteins, tau and 14-3-3, were investigated in the GCIs of 21 patients with MSA. Both proteins were detected in a subset of GCIs, but not in all the MSA cases. In some studies it has been reported that tau can be detected in at least a significant number of GCIs [1, 8, 38, 43, 51, 54, 56, 66], but in other studies the presence of tau in GCIs was not observed [34, 44]. In the cohort studied here, some GCIs in a subset of MSA cases were tau immunoreactive, but in some cases the α-syn-positive GCIs demonstrated a paucity of tau immunoreactivity (Table 1). Furthermore, the majority of these MSA cases showed no tau-positive GCIs in the cerebellum. These results indicate that the controversy of whether tau is present in GCIs can be explained, at least in part, by the specific subset of patients and the brain regions analyzed in prior independent studies, and this might reflect intrinsic pathological heterogeneity in MSA, not unlike the clinical variability in this disorder. Furthermore, previous analyses of GCIs with anti-phosphorylation specific antibodies suggested that tau was hypophosphorylated in these lesions [8]. Consistent with the results by Cairns et al. [8], GCIs containing tau demonstrated a paucity of staining with PHF-1, weak staining with PHF-6 (Fig. 2D, upper inset), and robust labeling with Tau-1 (Fig. 2D).
The accumulation of tau in pathological lesions in oligodendrocytes is also observed in other neurodegenerative disorders, such as coiled bodies in supranuclear palsy and corticobasal degeneration [9, 15]. Coiled bodies are typically morphologically distinct from GCIs. They commonly encircle the nucleus and extend into proximal cellular processes. These coiled bodies are comprised of bundles of tau filaments and they are not stained with antibodies to α-syn [69]. Alternatively spliced isoforms of tau containing the exon 10 insert (i.e., four microtubule binding repeats, 4R-tau) are the predominant components of coiled bodies [17, 60]. In one study, where the isoforms of tau in GCIs were analyzed biochemically, it was determined that 4R-tau isoforms were the major tau species in GCIs [54]. Unfortunately, frozen tissue from cases with sufficient tau-positive GCIs was not available to us to perform a similar biochemical analysis.
In some MSA cases, 14-3-3 proteins accumulated in a significant proportion of GCIs. However, in other cases, 14-3-3 could not be detected in any GCI. Recently, Kawamoto et al. [37] reported the presence of 14-3-3 proteins in GCIs; however, in their cohort of patients a high percentage of, but not all, GCIs were immunopositive for 14-3-3 proteins. These findings suggest that interaction between 14-3-3 and α-syn is not necessary for the formation of GCIs. Moreover, due to the temporal limitations of analyzing post-mortem specimens, it is difficult to ascertain at which stage of GCIs formation 14-3-3 proteins are incorporated. Once available, transgenic mouse models of MSA with an age-dependent accumulation of GCIs will be better suited to address this issue. 14-3-3 polypeptides are believed to act as adaptor proteins that bind to phosphorylated motifs [18, 61], and 14-3-3 has been shown to interact with α-syn in cells, while α-syn has also been shown to be a phosphoprotein [46] that is hyperphosphorylated in pathological lesions of PD, DLB and MSA [19]. It has been suggested that phosphorylation of α-syn may play a role in promoting fibril formation [19], but the mechanism to account for how this occurs remains to be elucidated. It is possible that 14-3-3 accumulates in GCIs by binding to phosphorylated α-syn. Similar to 14-3-3 and tau, synphilin, another α-syn-binding protein, also is found only in a subset of α-syn inclusions [71].
The proteins α-syn and tau share many similar properties. Both can adopt an unfolded confirmation in solutions [59, 72] and they can polymerize into fibrils leading to the formation of pathological lesions [14, 16]. They are also predominantly neuronal proteins, although they are likely expressed at low levels in oligodendrocytes [40, 57] and they can accumulate in these cells to form inclusions. The presence of tau in some GCIs is consistent with our resent findings that α-syn fibrils formation can be an initiator of tau fibrillogenesis [25]. The changes in cellular physiology that result in the formation of α-syn and tau inclusions are still unclear, but it is possible that the accumulation of interacting proteins in these inclusions may contribute to cell death by leading to the sequestration of key molecular mediators of homeostatic processes, thereby further impairing the regulation of normal cellular functions.
References
Abe H, Yagishita S, Amano N, Iwabuchi K, Hasegawa K, Kowa K (1992) Argyrophilic glial intracytoplasmic inclusions in multiple system atrophy: immunocytochemical and ultrastructural study. Acta Neuropathol 84:273–277
Arima K, Murayama S, Mukoyama M, Inose T (1992) Immunocytochemical and ultrastructural studies of neuronal and oligodendroglial cytoplasmic inclusions in multiple system atrophy. Acta Neuropathol 83:453–460
Arima K, Ueda K, Sunohara N, Arakawa K, Hirai S, Nakamura M, Tonozuka-Uehara H, Kawai M (1998) NACP/α-synuclein immunoreactivity in fibrillary components of neuronal and oligodendroglial cytoplasmic inclusions in the pontine nuclei in multiple system atrophy. Acta Neuropathol 96:439–444
Athanassiadou A, Voutsinas G, Psiouri L, Leroy E, Polymeropoulos MH, Ilias A, Maniatis GM, Papapetropoulos T (1999) Genetic analysis of families with Parkinson disease that carry the Ala53Thr mutation in the gene encoding α-synuclein. Am J Hum Genet 65:555–558
Baba M, Nakajo S, Tu PH, Tomita T, Nakaya K, Lee VM-Y, Trojanowski JQ, Iwatsubo T (1998) Aggregation of α-synuclein in Lewy bodies of sporadic Parkinson's disease and dementia with Lewy bodies. Am J Pathol 152:879–884
Binder LI, Frankfurter A, Rebhun LI (1985) The distribution of tau in the mammalian central nervous system. J Cell Biol 101:1371–1378
Boston PF, Jackson P, Thompson RJ (1982) Human 14-3-3 protein: radioimmunoassay, tissue distribution, and cerebrospinal fluid levels in patients with neurological disorders. J Neurochem 38:1475–1482
Cairns NJ, Atkinson PF, Hanger DP, Anderton BH, Daniel SE, Lantos PL (1997) Tau protein in the glial cytoplasmic inclusions of multiple system atrophy can be distinguished from abnormal tau in Alzheimer's disease. Neurosci Lett 230:49–52
Chin SS, Goldman JE (1996) Glial inclusions in CNS degenerative diseases. J Neuropathol Exp Neurol 55:499–508
Conway KA, Harper JD, Lansbury PT (1998) Accelerated in vitro fibril formation by a mutant α-synuclein linked to early-onset Parkinson disease. Nat Med 4:1318–1320
Dickson DW, Liu W, Hardy J, Farrer M, Mehta N, Uitti R, Mark M, Zimmerman T, Golbe L, Sage J, Sima A, D'Amato C, Albin R, Gilman S, Yen SH (1999) Widespread alterations of α-synuclein in multiple system atrophy. Am J Pathol 155:1241–1251
Duda JE, Giasson BI, Gur TL, Montine TJ, Robertson D, Biaggioni I, Hurtig HI, Stern MB, Gollomp SM, Grossman M, Lee VM-Y, Trojanowski JQ (2000) Immunohistochemical and biochemical studies demonstrate a distinct profile of α-synuclein permutations in multiple system atrophy. J Neuropathol Exp Neurol 59:830–841
Duda JE, Giasson BI, Mabon ME, Miller DC, Golbe LI, Lee VM-Y, Trojanowski JQ (2002) Concurrence of α-synuclein and tau brain pathology in the Contursi kindred. Acta Neuropathol 104:7-11
Duda JE, Lee VM-Y, Trojanowski JQ (2000) Neuropathology of synuclein aggregates. J Neurosci Res 61:121–127
Feany MB, Mattiace LA, Dickson DW (1996) Neuropathologic overlap of progressive supranuclear palsy, Pick's disease and corticobasal degeneration. J Neuropathol Exp Neurol 55:53–67
Forman MS, Lee VM-Y, Trojanowski JQ (2000) New insights into genetic and molecular mechanisms of brain degeneration in tauopathies. J Chem Neuroanat 20:225–244
Forman MS, Zhukareva V, Bergeron C, Chin SS, Grossman M, Clark C, Lee VM-Y, Trojanowski JQ (2002) Signature tau neuropathology in gray and white matter of corticobasal degeneration. Am J Pathol 160:2045–2053
Fu H, Subramanian RR, Masters SC (2000) 14-3-3 proteins: structure, function, and regulation. Annu Rev Pharmacol Toxicol 40:617–647
Fujiwara H, Hasegawa M, Dohmae N, Kawashima A, Masliah E, Goldberg MS, Shen J, Takio K, Iwatsubo T (2002) α-Synuclein is phosphorylated in synucleinopathy lesions. Nat Cell Biol 4:160–164
Gelb DJ, Oliver E, Gilman S (1999) Diagnostic criteria for Parkinson disease. Arch Neurol 56:33–39
George JM, Jin H, Woods WS, Clayton DF (1995) Characterization of a novel protein regulated during the critical period for song learning in the zebra finch. Neuron 15:361–372
Giasson BI, Uryu K, Trojanowski JQ, Lee VM-Y (1999) Mutant and wild type human α-synuclein assemble into elongated filaments with distinct morphologies in vitro. J Biol Chem 274:7619–7622
Giasson BI, Jakes R, Goedert M, Duda JE, Leight S, Trojanowski JQ, Lee VM-Y (2000) A panel of epitope-specific antibodies detects protein domains distributed throughout human alpha-synuclein in Lewy bodies of Parkinson's disease. J Neurosci Res 59:528–533
Giasson BI, Duda JE, Quinn SM, Zhang B, Trojanoswki JQ, Lee VM-Y (2002) Neuronal α-synucleinopathy with severe movement disorder in mice expressing A53T human α-synuclein. Neuron 34: 521–533
Giasson BI, Forman MS, Higuchi M, Golbe LI, Graves CL, Kotzbauer PT, Trojanowski JQ, Lee VM-Y (2003) Initiation and synergistic fibrillization of tau and alpha-synuclein. Science 300:636–640
Gilman S, Low PA, Quinn N, Albanese A, Ben Shlomo Y, Fowler CJ, Kaufmann H, Klockgether T, Lang AE, Lantos PL, Litvan I, Mathias CJ, Oliver E, Robertson D, Schatz I, Wenning GK (1999) Consensus statement on the diagnosis of multiple system atrophy. J Neurol Sci 163:94–98
Golbe LI, Di Iorio G, Sanges G, Lazzarini AM, La Sala S, Bonavita V, Duvoisin RC (1996) Clinical genetic analysis of Parkinson's disease in the Contursi kindred. Ann Neurol 40:767–775
Graham JG, Oppenheimer DR (1969) Orthostatic hypertension and nicotine insensitivity in a case of mutliple system atrophy. J Neurol Neurosurg Psychiatry 32:28–34
Hoffmann R, Lee VM-Y, Leight S, Varga I, Otvos L Jr (1997) Unique Alzheimer's disease paired helical filament specific epitopes involve double phosphorylation at specific sites. Biochemistry 36:8114–8124
Hong M, Zhukareva V, Vogelsberg-Ragaglia V, Wszolek Z, Reed L, Miller BI, Geschwind DH, Bird TD, McKeel D, Goate A, Morris JC, Wilhelmsen KC, Schellenberg GD, Trojanowski JQ, Lee VM-Y (1998) Mutation-specific functional impairments in distinct tau isoforms of hereditary FTDP-17. Science 282:1914–1917
Iwai A, Masliah E, Yoshimoto M, Ge N, Flanagan L, Silva HA de, Kittel A, Saitoh T (1995) The precursor protein of non-A beta component of Alzheimer's disease amyloid is a presynaptic protein of the central nervous system. Neuron 14:467–475
Jakes R, Spillantini MG, Goedert M (1994) Identification of two distinct synucleins from human brain. FEBS Lett 345:27–32
Jensen PH, Hager H, Nielsen MS, Hojrup P, Gliemann J, Jakes R (1999) α-synuclein binds to tau and stimulates the protein kinase A-catalyzed tau phosphorylation of serine residues 262 and 356. J Biol Chem 274:25481–25489
Kato S, Nakamura H (1990) Cytoplasmic argyrophilic inclusions in neurons of pontine nuclei in patients with olivopontocerebellar atrophy: immunohistochemical and ultrastructural studies. Acta Neuropathol 79:584–594
Kato S, Nakamura H, Hirano A, Ito H, Llena JF, Yen SH (1991) Argyrophilic ubiquitinated cytoplasmic inclusions of Leu-7-positive glial cells in olivopontocerebellar atrophy (multiple system atrophy). Acta Neuropathol 82:488–493
Kawamoto Y, Akiguchi I, Nakamura S, Honjyo Y, Shibasaki H, Budka H (2002) 14-3-3 proteins in Lewy bodies in Parkinson disease and diffuse Lewy body disease brains. J Neuropathol Exp Neurol 61:245–253
Kawamoto Y, Akiguchi I, Nakamura S, Budka H (2002) Accumulation of 14-3-3 proteins in glial cytoplasmic inclusions in multiple system atrophy. Ann Neurol 52:722–731
Kobayashi K, Miyazu K, Katsukawa K, Fukutani Y, Mukai M, Nakamura I, Yamaguchi N, Matsubara R, Isaki K (1992) Cytoskeletal protein abnormalities in patients with olivopontocerebellar atrophy—an immunocytochemical and Gallyas silver impregnation study. Neuropathol Appl Neurobiol 18:237–249
Lantos PL (1997) Mutliple system atrophy. Brain Pathol 7:1293–1297
LoPresti P, Szuchet S, Papasozomenos SC, Zinkowski RP, Binder LI (1995) Functional implications for the microtubule-associated protein tau: localization in oligodendrocytes. Proc Natl Acad Sci USA 92:10369–10373
Markopoulou K, Wszolek ZK, Pfeiffer RF, Chase BA (1999) Reduced expression of the G209A α-synuclein allele in familial Parkinsonism. Ann Neurol 46:374–381
McKeith IG, Galasko D, Kosaka K, Perry EK, Dickson DW, Hansen LA, Salmon DP, Lowe J, Mirra SS, Byrne EJ, Lennox G, Quinn NP, Edwardson JA, Ince PG, Bergeron C, Burns A, Miller BL, Lovestone S, Collerton D, Jansen EN, Ballard C, Vos RA de, Wilcock GK, Jellinger KA, Perry RH (1996) Consensus guidelines for the clinical and pathologic diagnosis of dementia with Lewy bodies (DLB): report of the consortium on DLB international workshop. Neurology 47:1113–1124
Murayama S, Arima K, Nakazato Y, Satoh J, Oda M, Inose T (1992) Immunocytochemical and ultrastructural studies of neuronal and oligodendroglial cytoplasmic inclusions in multiple system atrophy. Acta Neuropathol 84:32–38
Nakazato Y, Yamazaki H, Hirato J, Ishida Y, Yamaguchi H (1990) Oligodendroglial microtubular tangles in olivopontocerebellar atrophy. J Neuropathol Exp Neurol 49:521–530
Narhi L, Wood SJ, Steavenson S, Jiang Y, Wu GM, Anafi D, Kaufman SA, Martin F, Sitney K, Denis P, Louis JC, Wypych J, Biere AL, Citron M (1999) Both familial Parkinson's disease mutations accelerate α-synuclein aggregation. J Biol Chem 274:9843–9846
Okochi M, Walter J, Koyama A, Nakajo S, Baba M, Iwatsubo T, Meijer L, Kahle PJ, Haass C (2000) Constitutive phosphorylation of the Parkinson's disease associated alpha-synuclein. J Biol Chem 275:390–397
Ostrerova N, Petrucelli L, Farrer M, Mehta N, Choi P, Hardy J, Wolozin B (1999) α-Synuclein shares physical and functional homology with 14-3-3 proteins. J Neurosci 19:5782–5791
Otvos L Jr, Feiner L, Lang E, Szendrei GI, Goedert M, Lee VM-Y (1994) Monoclonal antibody PHF-1 recognizes tau protein phosphorylated at serine residues 396 and 404. J Neurosci Res 39:669–673
Ozawa T, Okuizumi K, Ikeuchi T, Wakabayashi K, Takahashi H, Tsuji S (2001) Analysis of the expression level of α-synuclein mRNA using postmortem brain samples from pathologically confirmed cases of multiple system atrophy. Acta Neuropathol 102:188–190
Papadimitriou A, Veletza V, Hadjigeorgiou GM, Patrikiou A, Hirano M, Anastasopoulos I (1999) Mutated α-synuclein gene in two Greek kindreds with familial PD: incomplete penetrance? Neurology 52:651–654
Papp MI, Lantos PL (1992) Accumulation of tubular structures in oligodendroglial and neuronal cells as the basic alteration in multiple system atrophy. J Neurol Sci 107:172–182
Papp MI, Kahn JE, Lantos PL (1989) Glial cytoplasmic inclusions in the CNS of patients with multiple system atrophy (striatonigral degeneration, olivopontocerebellar atrophy and Shy-Drager syndrome). J Neurol Sci 94:79–100
Paxinou E, Chen Q, Weisse M, Giasson BI, Norris EH, Rueter SM, Trojanowski JQ, Lee VM-Y, Ischiropoulos H (2001) Induction of α-synuclein aggregation by intracellular nitrative insult. J Neurosci 21:8053–8061
Piao YS, Hayashi S, Hasegawa M, Wakabayashi K, Yamada M, Yoshimoto M, Ishikawa A, Iwatsubo T, Takahashi H (2001) Co-localization of α-synuclein and phosphorylated tau in neuronal and glial cytoplasmic inclusions in a patient with multiple system atrophy of long duration. Acta Neuropathol 101:285–293
Polymeropoulos MH, Lavedan C, Leroy E, Ide SE, Dehejia A, Dutra A, Pike B, Root H, Rubenstein J, Boyer R, Stenroos ES, Chandrasekharappa S, Athanassiadou A, Papapetropoulos T, Johnson WG, Lazzarini AM, Duvoisin RC, Di Iorio G, Golbe LI, Nussbaum RL (1997) Mutation in the α-synuclein gene identified in families with Parkinson's disease. Science 276:2045–2047
Probst-Cousin S, Bergmann M, Kuchelmeister K, Schroder R, Schmid KW (1996) Ubiquitin-positive inclusions in different types of multiple system atrophy: distribution and specificity. Pathol Res Pract 192:453–461
Richter-Landsberg C, Gorath M, Trojanowski JQ, Lee VM-Y (2000) α-Synuclein is developmentally expressed in cultured rat brain oligodendrocytes. J Neurosci Res 2000 62:9–14
Schmidt ML, Murray J, Lee VM-Y, Hill WD, Wertkin A, Trojanowski JQ (1991) Epitope map of neurofilament protein domains in cortical and peripheral nervous system Lewy bodies. Am J Pathol 139:53–65
Schweers O, Schonbrunn-Hanebeck E, Marx A, Mandelkow E (1994) Structural studies of tau protein and Alzheimer paired helical filaments show no evidence for beta-structure. J Biol Chem 269:24290–24297
Sergeant N, Wattez A, Delacourte A (1999) Neurofibrillary degeneration in progressive supranuclear palsy and corticobasal degeneration: tau pathologies with exclusively "exon 10" isoforms. J Neurochem 72:1243–1249
Skoulakis EM, Davis RL (1998) 14-3-3 proteins in neuronal development and function. Mol Neurobiol 16:269–284
Spillantini MG, Schmidt ML, Lee VM-Y, Trojanowski JQ, Jakes R, Goedert M (1997) α-synuclein in Lewy bodies. Nature 388:839–840
Spillantini MG, Crowther RA, Jakes R, Hasegawa M, Goedert M (1998) α-Synuclein in filamentous inclusions of Lewy bodies from Parkinson's disease and dementia with Lewy bodies. Proc Natl Acad Sci USA 95:6469–6473
Spira PJ, Sharpe DM, Halliday G, Cavanagh J, Nicholson GA (2001) Clinical and pathological features of a parkinsonian syndrome in a family with an Ala53Thr α-synuclein mutation. Ann Neurol 49:313–319
Szendrei GI, Lee VM-Y, Otvos L Jr (1993) Recognition of the minimal epitope of monoclonal antibody Tau-1 depends upon the presence of a phosphate group but not its location. J Neurosci Res 34:243–249
Takeda A, Arai N, Komori T, Iseki E, Kato S, Oda M (1997) Tau immunoreactivity in glial cytoplasmic inclusions in multiple system atrophy. Neurosci Lett 234:63–66
Trojanowski JQ, Schuck T, Schmidt ML, Lee VM-Y (1989) Distribution of tau proteins in the normal human central and peripheral nervous system. J Histochem Cytochem 37:209–215
Tu PH,Galvin JE, Baba M, Giasson B, Tomita T, Leight S, Nakajo S, Iwatsubo T, Trojanowski JQ, Lee VM-Y (1998) Glial cytoplasmic inclusions in white matter oligodendrocytes of multiple system atrophy brains contain insoluble α-synuclein. Ann Neurol 44:415–422
Wakabayashi K, Hayashi S, Kakita A, Yamada M, Toyoshima Y, Yoshimoto M, Takahashi H (1998) Accumulation of α-synuclein/NACP is a cytopathological feature common to Lewy body disease and multiple system atrophy. Acta Neuropathol 96:445–452
Wakabayashi K, Yoshimoto M, Tsuji S, Takahashi H (1998) α-Synuclein immunoreactivity in glial cytoplasmic inclusions in multiple system atrophy. Neurosci Lett 249:180–182
Wakabayashi K, Engelender S, Tanaka Y, Yoshimoto M, Mori F, Tsuji S, Ross CA, Takahashi H (2002) Immunocytochemical localization of synphilin-1, an α-synuclein-associated protein, in neurodegenerative disorders. Acta Neuropathol 103:209–214
Weinreb PH, Zhen W, Poon AW, Conway KA, Lansbury PT (1996) NACP, a protein implicated in Alzheimer's disease and learning, is natively unfolded. Biochemistry 35:13709–13715
Wenning GK, Ben Shlomo Y, Magalhaes M, Daniel SE, Quinn NP (1994) Clinical features and natural history of multiple system atrophy. An analysis of 100 cases. Brain 117:835–845
Wenning GK, Tison F, Ben Shlomo Y, Daniel SE, Quinn NP (1997) Multiple system atrophy: a review of 203 pathologically proven cases. Mov Disord 12:133–147
Withers GS, George JM, Banker GA, Clayton DF (1997) Delayed localization of synelfin (synuclein, NACP) to presynaptic terminals in cultured rat hippocampal neurons. Brain Res Dev Brain Res 99:87–94
Acknowledgements
This work was funded by grants from the National Institutes of Health and by a Pioneer Award from the Alzheimer Association. B.I.G. is the recipient of a fellowship from a Canadian Institutes of Health Research. J.E.D. is the recipient of an advances career development award from the Department of Veterans Affairs Research. The Harvard Brain Tissue Resource Center contributed some of the cases used in this study. The authors would like to thank Dr. Sharon Xie for assistance with statistic analysis and the families of patients who made this research possible.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Giasson, B.I., Mabon, M.E., Duda, J.E. et al. Tau and 14-3-3 in glial cytoplasmic inclusions of multiple system atrophy. Acta Neuropathol 106, 243–250 (2003). https://doi.org/10.1007/s00401-003-0726-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-003-0726-x