Abstract
Background
This article summarizes the emerging field of hypertension over the last decades. It covers paradigm shifts on hypertension from an undefined cardiovascular condition to the most relevant cardiovascular modifiable risk factor and the developments of drug treatments and interventional treatments to improve cardiovascular outcomes.
Methods
We performed a selective literature research in PubMed on trials published in the past until 2018 without time restrictions and covered unpublished trials disclosed in ClinicalTrials.org.
Results
The development of treatments of hypertension is a success story covering many decades from the early attempts with drug treatments, development of tolerable and effective medications to interventional techniques involving renal denervation, AV fistulas, and autonomic devices. Novel guidelines define new definitions and treatment targets of hypertension, which are a matter of ongoing discussion.
Conclusion
Despite the development of tolerable and effective drugs, new treatments in the field of neuroendocrine modulation by drugs and devices are still under development trying to further improve treatment of patients with hypertension and to further reduce cardiovascular events in those individuals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
History of misconceptions and successes in the developments of hypertension treatments
High blood pressure is now recognized as one of the leading and most prevalent causes for cardiovascular death and cardiovascular hospitalizations [1]. It is regarded as a highly relevant risk factor rather than a risk mediator, because it has been shown that blood pressure reduction reduces cardiovascular outcomes like stroke, myocardial infarction, and cardiovascular death dependent on blood pressure levels at baseline, accompanying cardiovascular risk and achieved blood pressure reduction [2, 3]. Organ perfusion, as early recognized by William Harvey, has been suggested to be dependent on blood pressure [4]. The development of blood pressure measurement, which was first performed in a horse in 1733 and later further developed by Riva-Rocci [5] and Korotkoff [6], paved the way to recognize that blood pressure levels beyond the requirement of organ perfusion are associated with cardiovascular outcomes and death [7]. However, there was a longstanding uncertainty of whether it might be useful to reduce blood pressure. John Hay wrote, in 1931, that “High blood pressure is often the penalty of success…” [8]. He stated in his conclusion section: “The greatest danger to a man with high blood pressure lies in its discovery, because then some fool is certain to try and reduce it” [8]. The connotation that hypertension is essential to success and certain life styles founded or at least influenced the term “essential hypertension” still used today. However, the strong association of elevated blood pressure with outcomes, in particular of malignant blood pressure (diastolic blood pressure above 110 mmHg), resulted in death rates of 80% after 1 year (Fig. 1a) [9]. The potential use of blood pressure-reducing drugs was scrutinized by studies after the development and implementation of diuretics showing that, in a similar population of patients, death rate was markedly reduced (Fig. 1a) [10].
Survival of patients with resistant hypertension who were untreated in 1939 and treated with diuretics 1981 (a). Press note on the death of President Roosevelt 1946 according to a cerebral hemorrhage after longstanding hypertension (b). Blood pressure values over 10 years of President Roosevelt in association with different historical events (c). President Roosevelt died finally due to a cerebral hemorrhage
One famous case of untreated hypertension was that of Franklin D. Roosevelt, who was diagnosed with elevated blood pressure in 1937. The blood pressure rose progressively from 160/90 mmHg to levels of 220/150 mmHg, which was strongly dependent on historical events in the following 7–8 years (Fig. 1b, c) [11, 12]. President Roosevelt died of an intracerebral hemorrhage on April 12th, 1945 aged 63 years after having developed renal failure and heart failure before. From the 1940–1950s, there was still a misbelief in the necessity of treating hypertension, because it was assumed that blood pressure reduction could lead to inadequate perfusion pressure and could damage organs.
The first controlled studies, which marked the paradigm changes into the future, were performed by the Veterans Administration Cooperative Study Group on antihypertensive agents funded by the National Institute of Health [13]. The first controlled, randomized study in hypertension investigated the effects of treatment on mortality and morbidity in hypertensive patients with a diastolic blood pressure averaging 115–129 mmHg [13]. This study was based on 143 male hypertensive patients (no women!) showing in a randomized study against placebo that hydrochlorothiazide or reserpine plus hydralazine significantly reduced blood pressure and resulted in a reduction of outcome events with 27 events in the placebo group and 2 events in the actively treated group (with 4 versus 0 death). Among those events, there were typical deaths for hypertensive complications like intracerebral bleeding, ruptured abdominal aortic aneurysm, sudden cardiac death, and stroke, as well as myocardial infarction [13]. This was later extended to patients with a lower diastolic blood pressure of 90–114 mmHg with a similar outcome reduction [14]. These studies paved the way for future outcome trials and started extensive efforts to develop novel, effective drug treatments drug treatments, with acceptable tolerability.
Development of treatments
Nutrition
The first experience with a blood pressure lowering diet was generated by Kempner who introduced a nutrition regimen consisting of fruit, fruit juice, and rice containing only 20 g of proteins, 5 g of fat, and less than 200 mg of sodium per day. He observed that beyond a strong body weight reduction, heart failure decompensations were reduced and papilledema was cleared in 322 out of 500 patients after this diet [15]. In hypertensive crises, there were heroic attempts to produce vasodilatation by pyrogens [16], or other toxic vasodilatory drugs [17, 18]. One of the most exciting topics in blood pressure research is salt. Increased salt intake leads to inhibition of endothelial sodium pumps in vessels, increasing intercellular sodium and calcium. This ultimately induces vascular smooth muscles contraction and increases peripheral vascular resistance [19]. A general reduction of the absorbed salt is a cost-effective and safe method to prevent high blood pressure and other cardiovascular diseases. However, since most of the consumed salt comes from industrially processed food [20], salt depletion is not possible without governmental help. The UK salt reduction program could diminish salt intake from 2003 to 2011 by 1.4 g/day resulting in a decrease of blood pressure by 3/1.2 mmHg (Sys/Dia) and 41 and 22% reduction in stroke and ischemic heart disease, respectively [21]. Although not everything can be explained by the cut in salt intake, the previous studies could already demonstrate the advantages of a lower salt consumption [22, 23]. Nevertheless, it should be noted that the 24-h urine collection method used in these trials cannot reflect the exact salt concentration [24]. Furthermore, an individual salt reduction seems to be difficult and might easier be achieved by diuretics.
Sympathetic nervous system
The first demonstration of the role of the sympathetic nervous system in circulatory regulation, in particular the role of the kidney, was provided by Carl Ludwig [25]. His ideas were further developed by J. Rose Bradford, showing that stimulation of renal nerves elevated blood pressure [26]. This led to first surgical attempts to reduce blood pressure by surgical interventions to interrupt the sympathetic innervation. One of them was decapsulation of the kidneys in 1936 with a subsequent reduction in blood pressure [27]. Resection of renal nerves was done for pain relief in hydronephrosis [28]. Furthermore, sympathetic splanchnicectomy resulted in a significant blood pressure reduction with a remarkable reduction of death rate depending on cardiovascular comorbidities [29, 30]. This treatment was performed in more than 1200 cases in the United States until 1953 [31]. However, these procedures were accompanied by a high mortality and severe side effects and rehospitalizations due to orthostatic hypotension, syncopes, erectile dysfunction, and incontinence [32]. Nevertheless, the clarification of mechanisms how the sympathetic nervous activation stimulates blood pressure elevation [33] led to the development of more selective interventional techniques to reduce blood pressure like renal sympathetic denervation decades later [34].
Development of drugs
The medical student Albert Vogl observed that the medication merbaphen (Novasurol®) for the treatment of syphilis increased diuresis. Medical student applied this drug 1919 in Wenckebach Clinic in Vienna undercover and provided an illustrative documentation about their surprising observation of a unexpectedly “torrential” [35] urine excretion. This finding was further developed to another mercury-containing diuretic Mersalyl (Salyrgan®) by the company Hoechst in Germany, which remained a standard diuretic for more than 30 years. Starting from an antibacterial chemotherapeutic, the first sulfure containing diuretics was discovered in 1949. This led to the development of the carboxy anhydrase inhibitor acetazolamide (Diamox®). Chlorothiazide was first introduced 1958 as a first orally effective agent [36]. Furosemide was developed 1973 by Hoechst (Germany) [37]. Potassium-sparing diuretics like amiloride and spironolactone were following some years later.
Rauwolfia drugs
Stimulated by the findings of blood pressure reduction by splanchnicectomy to reduce sympathetic activity, rauwolfia alkaloids were introduced first in the United States in 1940 and 1950 [38]. These drugs were based on an old traditional medication from India. It was isolated from the Indian root Apocynacee rauwolfia serpentina-bentham, a plant which was named after the German physician Leonard Rauwolf, practicing in Augsburg in 1560. Modification of the reserpine molecule did not lead to better compounds. However, this discovery was followed by the development of guanethidine and alpha-methyldopa. Alpha-methyldopa was shown to inhibit dopamine decarboxylase to deplete sympathetic neurotransmitter stores due to the inhibition of noradrenaline formation and leading to a less active neurotransmitter reference as the concept of “false transmitter” [39]. Neurosympathetic inhibition was further developed by the development of clonidine by Boehringer-Ingelheim (Germany) activating presynaptic α2-adrenergic receptors [40]. Alpha-adrenoceptor blockers phentolamine, phenoxibenzalin, and prazosin were developed later. Some of these agents are still in use for pheochromocytoma.
Beta-blockers
The first beta-blocker for clinical use was developed in 1958 (dichloriso-proteronol). It was not used clinically. Further compounds like pronenalol were developed in England and followed later by propanolol, which was introduced 1965. This was the first step in the development of more specific blockers of the beta1-adrenoceptor-subtype.
Renin–angiotensin system inhibitors
It has been known since 1898 that extracts of harvested kidneys from rabbits reinjected into rabbits increased blood pressure. This first observation was made by Tigerstedt and Bergman [41, Fig. 2]. Already in 1958, Franz Gross (President of the German Society of Cardiology and founding president of the German Hypertension League) first suggested an association between the renin–angiotensin system and hypertension. The first angiotensin-converting enzyme inhibitor was teprotide isolated from the venom of the snake Bothrops jararaca. Captopril was the first orally available ACE inhibitor (1977) followed by the development of losartan, the first angiotensin AT1-receptor antagonist introduced in 1995.
Discovery of the renin–angiotensin system. Rabbit kidney extracts were injected into rabbits. After a short drop in blood pressure, there was a longstanding increase in blood pressure. After denervating the heart (below), the initial drop in blood pressure was not present, which was associated with the abolished reduction in heart rate which might have been potentially due to lost baroreceptor effects after denervation. Hemodynamic data in nephrectomized rabbits show blood pressure increases without direct effects on the kidney rather than on the peripheral circulation [35]
Calcium antagonists
The first calcium antagonist was developed by Lindner in Germany (Segontin propylamin), which was developed to produce dilation of the coronary arteries [42]. Verapamil, a combination hybrid molecule from veratrin and papaverine, was discovered later. Cardiac effects of calcium antagonism were discovered by Albrecht Fleckenstein [43]. The novel calcium antagonists binding to the dihydropyridine site of Ca2+ channels are now in widespread use for hypertension and are discovered later (nifedipin, nisoldipine, amlodipine, and others).
Epidemiology and cardiovascular risk
Hypertension remains the most prevalent risk factor worldwide and is closely associated with cardiovascular outcomes [2]. Blood pressure increases with age and older people have higher a prevalence of hypertension. It was estimated that 31% of the world’s adults had hypertension in 2010, and 75% of those with hypertension lived in low- and middle-income countries. Of those, only 7.7% of patients with hypertension had their blood pressure (BP) controlled to less than 140/90 mmHg [44]. The number of patients with hypertension is projected to increase by 60%, bringing a total number of hypertensives to 1.6 billion in 2025 [45]. A continuous log-linear association between blood pressure and vascular events has been reported to a BP of 115/75 mmHg, with no apparent threshold [3]. The association between BP and events has been documented for men and women, with and without established vascular disease, individuals aged 40–89 years, and from different ethnicities [46, 47]. In 2013, the leading causes of death worldwide were ischemic heart disease and stroke, accounting for 1 in 4 deaths globally [44], both of them closely related to hypertension. It has been shown that every 10 mmHg reduction in SBP, the risk of major cardiovascular disease events is lowered by 20%, coronary heart disease by 17%, stroke by 27%, heart failure by 28%, and all-cause mortality by 13% [2]. Treatment and control of hypertension are not only important for the prevention of cardiovascular and renal events but also to reduce costs to societies.
Diagnosis
Thresholds for the definition of hypertension are provided in Table 1. The most frequently used blood pressure measurement modality is office-based or clinic BP measurement. International guidelines have endorsed a standard approach for clinic BP measurement, which involves the patient being seated and relaxed for 5 min before BP is recorded in the nondominant arm with an appropriately sized cuff and a validated device, with readings taken 3 times, at least 1 min apart, with the average of the last two readings [48]. However, in clinical practice, very often less rigor is paid in obtaining clinic BP, which may significantly affect the documented values [49]. To reduce variability and improve standardization, automated devices have been developed that record a series of seated unobserved BP. When SBP is measured this way it may be 5–10 mmHg lower than when measured with manually or even when patients are being observed or talking. Of note, this BP measurement modality was utilized in the SPRINT trial, which has led to a controversial discussion about the generalizability of the observed results [50].
Ambulatory blood pressure monitoring (ABPM) has become frequently used in Europe and other geographies as it provides a more comprehensive assessment of blood pressure of the day and night. It also allows identifying patients with distinct BP profiles such as patients with normal office BP and high ABP (masked hypertension) and those with high office but normal ABP (white-coat hypertension). ABP data have further been suggested to predict outcome better than office-based BP measurements [51]. A recently published analysis from the large Spanish ABPM registry (n = 63,910) [52], elegantly documented that 24-h, day-time, and night-time ambulatory systolic BP were indeed all better predictors of all-cause and cardiovascular mortality than clinic BP, which was consistent across subgroups of age, sex, and status with respect to obesity, diabetes, cardiovascular disease, and antihypertensive treatment. Interestingly white-coat hypertension and masked hypertension were both associated with an increased risk of death with the strongest association being observed with masked hypertensive patients.
Treatment goals
Controversy exists currently on BP treatment goals. Following publication of the 2013 ESC/ESH guidelines on hypertension, there appeared to be consensus regarding a goal BP of < 140/90 mmHg for most hypertensive with few exceptions: (i) elderly patients (> 80 years) with the initial SBP ≥ 160 mmHg were recommended to be lowered to SBPs between 150 and 140 mmHg, (ii) patients with severe chronic kidney disease and proteinuria to SBP < 130 mmHg, and (iii) a DBP target of < 85 mmHg was recommended in diabetics. The publication of several studies has recently revived the discussion on lower treatment goals in hypertension [2, 53,54,55]. The prospective, randomized, controlled SPRINT [53] trial documented in patients at high risk for cardiovascular events but without diabetes or prior stroke, that an intensive BP control (SBP target of < 120 mmHg) when compared with standard control (SBP target of < 140 mmHg), resulted in lower rates of fatal and nonfatal major cardiovascular events and death from any cause. It should be noted that the intensified study attained blood pressure values of 121 mmHg, while the standard group reached 136 mmHg. Two more well-conducted meta-analyses [2, 54] in more than 610,000 and 247,000 patients confirmed that SBP lowering to < 130 mmHg was associated with significantly reduced cardiovascular risk. It is important to mention, that the new guidelines will be published soon [56].
An important aspect of treatment of goals is the association of lower BP values and increase in risk, which has been described as the J-curve phenomenon. A recently published analysis of the ONTARGET/TRANSCEND study [55] suggested that lowering SBP < 120 mmHg during treatment was associated with increased risk of cardiovascular outcomes except for myocardial infarction and stroke. Similar patterns were observed for DBP < 70 mmHg, plus increased risk for myocardial infarction and hospital admission for heart failure (Fig. 3). Very low blood pressure achieved on treatment was associated with increased risks of several cardiovascular disease events. This association is supported by data from the CLARIFY registry [57] in patient with coronary artery disease, in which BP values of < 120/< 70 mmHg were each associated with adverse cardiovascular outcomes, including mortality (Fig. 4). These two studies support the concept of the existence of a J-curve phenomenon and suggest that the lowest BP possible is not necessarily the optimal target for high-risk patients. Special attention has to be paid to lower BP not too intensively. In light of the available evidence, the optimal target blood pressure target appears to be between 120 and 130 mmHg for SBP and between 70 and 80 mmHg for DBP in patients with hypertension [58].
Risk of the primary endpoint (cardiovascular death, myocardial infarction, stroke, and hospital admission for heart failure) according to mean achieved systolic blood pressure of 30,937 patients at high cardiovascular risk [49]
Risk of cardiovascular death, myocardial infarction, or stroke according to baseline diastolic blood pressure in 22,672 patients with hypertension and coronary artery disease [51]
Medical treatment of hypertension
Beside lifestyle changes, medical treatment represents a cornerstone in the treatment of hypertension. While lifestyle changes may modify cardiovascular risk in many ways, the main benefits of antihypertensive treatment are due to lowering of BP per se. Diuretics, calcium antagonists, beta-blockers, angiotensin-converting enzyme (ACE) inhibitors, and angiotensin receptor blockers are all suitable for the initiation of antihypertensive therapy as they have been shown to reduce morbidity and mortality in large, randomized-controlled studies [59,60,61,62]. The European guidelines of 2013 and the latest US guidelines favor a combination therapy over a monotherapy in case of moderate or severe elevation of blood pressure and, if patients are at high risk [63, 64]. Which drug should be considered is dependent of the respective cardiovascular risk profile and cardiovascular as noncardiovascular comorbidities.
Drug treatment
Diuretics, calcium antagonists (CCBs), angiotensin-converting enzyme inhibitors (ACE-Is), and angiotensin-II receptor blockers (ARBs) have a class IA recommendation as monotherapy for the initial antihypertensive therapy. Their different application should be considered depending on concomitant diseases [63, 64]. Diuretics are superior in preventing heart failure, CCBs are superior in the prevention of stroke but inferior in the reduction of new-onset heart failure, and ACE-Is and ARBs are, if compared to CCBs, inferior in prevention of stroke but superior in prevention of chronic kidney disease [2, 65, 66]. Beta-blockers are controversial as they are inferior in the reduction of cardiovascular events, total mortality and especially inferior in preventing stroke, compared to ARBs [2, 67] (Table 2). Furthermore, they also appear to have more side effects [68].
The different substance classes can be combined as they have different synergistic effects on blood pressure reduction (Fig. 5).
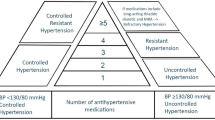
Resistant arterial hypertension
Resistant hypertension is defined as high blood pressure that is insufficiently controlled according to the current guidelines. Around 5–15% of all patients with hypertension have apparent resistant hypertension [69,70,71], the exact prevalence being unknown. The standard regimen for the treatment of resistant hypertension contains of ACE-I/ARB, diuretic, and CCB. According to recently published data, spironolactone appears to be the most effective fourth-line agent for the treatment of resistant hypertension [71,72,73], when compared with bisoprolol and doxazosin.
Adherence and combination therapy
Crucial for the success of every medical treatment is the adherence and persistence to the prescribed regimen. In a study of 255.000 patients, only 56.3% were still adherent after a 2-year period to their prescribed medication plan [74]. In a recent meta-analyses, nonadherence in hypertension appears to range from 23 to 66%, respectively [75]. Important risk factors for nonadherence are younger age, male sex, prescription of diuretics, a higher number of daily doses, and different drugs [76]. These finding suggest that, especially in patients with uncontrolled hypertension, fixed-dose combinations may help to improve adherence and persistence. Further work has shown that the combination therapy is superior to a doubling of monotherapy by 4–5 times [77]. Interestingly, a recent published cross-over study has shown that the initial treatment with a pill containing four different drugs with a quarter of the normal concentration is resulting in significantly more potent blood pressure reduction compared to monotherapy [78]. Other strategies like SMS-Text Adherence Support (StAR), Refill and Medication Scale (ARMS), and urine/plasma toxicological analysis may help to improve adherence [79,80,81]. In summary, several antihypertensive drugs can reduce blood pressure sufficiently, however mainly due to nonadherence and prescription of suboptimal drug combination, control rates remain unsatisfactorily low. Close collaboration between physicians and patients is crucial for treatment success.
Interventional treatment of hypertension
Renal denervation
Catheter-based renal denervation (RDN) is a safe and minimally invasive treatment option for patients with uncontrolled hypertension, and has been shown to reduce renal and central sympathetic activity [82, 83]. Several observational studies [84, 85], as well as national and international registries [86,87,88], have validated the outcomes of the pivotal Symplicity HTN-1 and HTN-2 trials. However, after 6 months, the randomized, blinded, sham-controlled Symplicity HTN-3 trial [89] could not prove the superiority of RDN in reducing blood pressure (BP) compared with a sham procedure. The neutral results of the Symplicity HTN-3 trial have been extensively discussed and attributed to several possible confounding factors, including inadequate patient selection, low operator experience, and inadequate procedural performance [90]. In contrast, the multicenter, randomized-controlled DENER-HTN study established the superiority of RDN and antihypertensive medication over pharmacotherapy alone [91]. The study enrolled 121 patients who received a standardized triple antihypertensive treatment during a 4-week run-in period; the remaining 106 patients with resistant hypertension (verified by the day-time ambulatory BP) were randomly allocated to undergo RDN or served control procedures. After randomization, if home BP was ≥ 135/85 mmHg, patients in both groups underwent stepped-care antihypertensive drug treatment from months 2–5. The primary efficacy endpoint at 6 months was met in the RDN group with a reduction in the mean ambulatory day-time systolic BP of 16 mmHg following RDN compared with a decreased systolic BP of 10 mmHg in the control group [91]. However, even this comprehensive and well-conducted investigation reported a substantial variation of interindividual 24-h ambulatory BP response because of various explanations after the detection of the procedure including nonadherence (Fig. 6) [92, 93].

Modified from Azizi et al. [87]
Fan plots of individual changes in day-time ambulatory systolic blood pressure (SBP) between baseline and 6 months in the renal denervation group (red lines) and control group (blue lines) in patients who were fully adherent and nonadherent (partially nonadherent plus completely nonadherent) to SSAHT. SSAHT indicates standardized stepped antihypertensive treatment.
A series of new studies have been designed after judiciously considering the limitations and learnings of the previous studies to address open questions and to elucidate the role of RDN in the armamentarium of antihypertensive treatments [85]. The prospective, randomized, double-blind, sham-controlled SPYRAL HTN studies were conducted to ascertain the effect of RDN in patients with uncontrolled BP without concomitant medication (OFF-MED) and in patients with concomitant medication (ON-MED) [94]. The studies enrolled patients with combined hypertension having an office systolic BP of 150–180 mmHg, office diastolic BP of > 90 mmHg, and 24-h systolic BP of 140–170 mmHg at 21 centers in the United States (US), Europe, Japan, and Australia [95, 96]. Compared with the SYMPLICITY HTN protocols, the study design of SPYRAL HTN comprises several critical modifications: (i) a multi-electrode catheter designed to facilitate reliable circumferential four-quadrant ablation; (ii) the main distal renal artery and all branches and accessory arteries will be treated, which has reportedly exhibited the highest change in the renal norepinephrine and axon density in pig [97]; (iii) the procedure was performed in advanced centers, with all involved in the study having experienced RDN, and has been conducted by one proceduralist per center only. The SPYRAL HTN OFF-MED trial obtained the primary outcomes from the interim analysis of 80 patients (the intervention group, n = 38; the sham-control group, n = 42), demonstrating a significant difference in the primary endpoint 24-h ambulatory BP and office BP in favor of RDN at 3 months (Fig. 7) [98]. In addition, no relevant adverse event was reported in the RDN and sham-controlled groups [98]. Notably, this trial provides the biological proof-of-principle for the efficacy of catheter-based RDN to reduce BP in patients with uncontrolled BP not treated with antihypertensive medications. Particular attention should be paid to two recently published renal denervation studies. The SPYRAL HTN-ON-MED [99] trial investigated the effect of RDN in the presence of blood pressure medication. The RADIANCE-HTN SOLO ([100]) trial used a balloon-based ultrasound ablation catheter. Both studies could de novo confirm the efficacy of renal denervation and show a significant reduction in blood pressure.

Modified from Townsend et al. [92]
Changes at 3 months in office and ambulatory SBP and DBP for renal denervation and sham-controlled groups 95% CIs and unadjusted p values shown. SBP systolic blood pressure, DBP diastolic blood pressure.
Carotid baroreceptor stimulation
The first human feasibility study with the implantation of the Rheos system (CVRx, Minneapolis, MN) was the nonrandomized DEBuT-HT open-label trial, which enrolled 45 patients with resistant hypertension. After 2-year follow-up, a significant decline in mean office BP by 33/22 mmHg was reported [101]. Recently, the 6-year long-term safety and efficacy results of three baroreflex activation therapy (BAT) studies (patients enrolled initially, n = 383; patients after 6 years, n = 48), namely the US Rheos Feasibility Trial (prospective, nonrandomized), the DEBuT-HT Trial (prospective, nonrandomized), and the Rheos Pivotal Trial (randomized, sham-controlled) [102]. Of note, all three trials used the first-generation Rheos system (CVRx), which was implanted in patients with resistant hypertension. The findings provided crucial information, suggesting that BAT exerted a sustained effect on BP over the entire follow-up period without major safety issues. However, some limitations, which now seem prerequisites for device-based hypertension trials, warrant consideration while interpreting the study results; these limitations comprise the lack of 24-h ambulatory BP data, the absence of a control group, and the lack of adherence testing to antihypertensive medication [103].
Central iliac arteriovenous anastomosis
The ROX Medical arteriovenous coupler (ROX Medical, San Clemente, CA, USA) is a stent-like device made of nitinol that displays preformed shape memory, thereby sustaining the constant pressure gradient and flow. Under fluoroscopic guidance, the device is percutaneously deployed between the external iliac vein and artery at the femoral head level, causing an arteriovenous shunt of approximately 800–1200 mL/min [104]. Immediately after the dilatation of the coupler using a 4-mm noncompliant balloon, the invasively measured BP declines with an elevation in the cardiac output, stroke volume, and ejection fraction and a reduction in the end-diastolic pressure [105]. The multicenter, open-label, randomized, controlled trial (ROX CONTROL HTN trial) investigated the effects of anastomosis and standard care (medication continuation), or standard care alone in patients with confirmed office and ambulatory resistant hypertension [104]. After 12 months, the intention-to-treat analysis (n = 39) revealed that the office BP and 24-h ambulatory BP were decreased by 25/21 and 13/15 mmHg, respectively [106]. The 1-year follow-up revealed that 14 patients (33%) developed ipsilateral venous stenosis after coupler therapy [106]. Remarkably, in contrast to RDN [95, 96], the BP decline was comparable in patients with either combined (office SBP, > 140 mmHg; DBP, > 90 mmHg) or isolated systolic BP (office SBP, > 140 mmHg; DBP, < 90 mmHg) [25]. Notably, the ROX coupler device is currently undergoing evaluation in the pivotal sham-controlled ROX CONTROL Hypertension (HTN)-2 (NCT02895386) study that started enrollment in 2017 in the US and Europe.
Endovascular baroreflex amplification
The CALM (Controlling and Lowering Blood Pressure with the MobiusHD) trial was the first-in-man, multicenter, open-label, and nonrandomized study that enrolled patients (n = 31) with resistant hypertension in the US and Europe with an objective to investigate the safety and efficacy of the MobiusHD implant (Vascular Dynamics, Inc.), a dedicated carotid stent developed to passively augment the pulsatile strain and reduce BP by increasing the carotid sinus baroreceptor activation and enhanced sympatho-inhibition. The carotid stent was percutaneously delivered to the carotid sinus using a rapid exchange catheter through a conventional 8-F guide catheter or a 6-F sheath. In the study, the average inclusion office-cuff BP and average inclusion 24-h ambulatory BP were 182/106 and 164/96 mmHg, respectively. Of note, 14 patients reached the 180-day safety endpoint, with an average variation in the office BP and 24-h ambulatory BP monitoring of − 23/−10 and − 14/−8 mmHg, respectively. Furthermore, nine patients with a 1-year follow-up exhibited a sustained lowering in the office BP of 26/16 mmHg [107]. Figure 8 depicts a summary of the different interventional treatments mentioned in this review.
Perspectives
Defining treatment goals (in particular lower boundaries of optimal blood pressure targets to achieve) as well as implementing innovative treatments providing the best tolerability and efficacy to patients is still a challenge in hypertension. New treatment options from the interventional field are on the horizon, which requires a close interdisciplinary collaboration between cardiologists, nephrologists, and hypertension specialists to achieve the optimal goals for patients with hypertension and to provide the best benefit concerning endpoint reduction and quality of life. Further research is needed to improve our understanding of pathophysiological backgrounds and novel treatment approaches; the majority of them need to be further studied in prospective randomized clinical trials.
References
World Health Organization (2013) A global brief on hypertension—World Health Day 2013
Ettehad D, Emdin CA, Kiran A et al (2016) Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 387:957–967
Lewington S, Clarke R, Qizilbash N et al (2002) Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 360:1903–1913
Harvey W, Sigerist HE (1628) Exercitatio anatomica de motu cordis et Sanguinis in animalibus. Movement of the heart and blood in animals. Sumptibus Guilielmi Fitzeri
Hales S (1733) Statical essays: Containing haemastaticks; Or, an account of some hydraulick and hydrostatical experiments made on the blood and blood-vessels of animals. Meet Counc R Soc 2:426
Multanowski M (1970) Korotkoff’s method. The history of its discovery, of its clinical and experimental interpretation and modern appreciation. The 50th anniversary of N.S. Korotkoff’s death. Cor Vasa 12:106
Paullin JE (1926) Ultimate results of essential hypertension. JAMA 87:925–928
Hay J (1931) A british medical association lecture on the significance of a raised blood pressure. Br Med J 2:43–47
Keith N, Wagener H, Barker N (1974) Some different types of essential hypertension: their course and prognosis. Am J Med SCI 268:336–345
Gudbrandsson T (1981) Malignant hypertension; A clinical follow-up study with special reference to renal and cardiovascular function and immunogenetic factors. Acta Med Scand 650:1–62
Ross CG (1945) “Came out of clear sky,” says President’s physician. St Louis Post-Dispatch A2
Messerli FH (1995) This day 50 years ago. N Engl J Med 332:1038–1039
Veterans Administration Cooperative Study Group on Antihypertensive Agents (1967) Effects of treatment on morbidity in hypertension. Results in patients with diastolic blood pressures averaging 115 through 129 mm Hg. JAMA 202:1028–1034
Veterans Administration Cooperative Study Group on Antihypertensive Agents (1970) Effects morbidity of treatment on in hypertension. Results in patients with diastolic blood pressures averaging 90 through 114 mm Hg. JAMA 213:1143–1152
Kempner W (1948) Treatment of hypertensive vascular disease with rice diet. Am J Med 4:545–577
Page I, Taylor R (1949) Pyrogens in the treatment of malignant hypertension. Mod Concepts Cardiovasc Dis 18:51
Freis E, Wilkins R (1947) Effect of pentaquine in patients with hypertension. Proc Soc Exp Biol Med 64:455–458
Hines EA (1946) The thiocyanates in the treatment of hypertensive disease. Med Clin North Am 30:869–877
Adrogué HJ, Madias NE (2007) Sodium and potassium in the pathogenesis of hypertension. N Engl J Med 356:1966–1978
Center for Disease Control (2010) Centers for disease control and prevention morbidity and mortality weekly report. MMWR Morb Mortal Wkly Rep 59(24):746–749
He FJ, Pombo-Rodrigues S, MacGregor GA (2014) Salt reduction in England from 2003 to 2011: its relationship to blood pressure, stroke and ischaemic heart disease mortality. BMJ Open 4:e004549. https://doi.org/10.1136/bmjopen-2013-004549
Sasaki N (1980) Epidemiological studies on hypertension in northeast Japan. In: Kesteloot H, Joossens JV (eds) Epidemiology of arterial blood pressure. Developments in cardiovascular medicine, vol 8. Springer, Dordrecht, pp 367–377
Karppanen H, Mervaala E (2006) Sodium intake and hypertension. Prog Cardiovasc Dis 49:59–75
Lerchl K, Rakova N, Dahlmann A et al (2015) Agreement between 24-hour salt ingestion and sodium excretion in a controlled environment. Hypertension 66:850–857
Ludwig C (1842) De viribus physicis secretionem urinae adjuvantibus: Marburge Cattorum. Elwert, Marburg
Bradford J (1889) The innervation of the renal blood vessels. J Physiol 10:358–432
Sen S (1936) Some observations on decapsulation and denervation of the kidney. Br J Urol 8:319–328
Papin E, Ambard L (1924) Resection of the nerves of the kidney for nephralgia and small hydronephroses. J Urol 11:337
Page I, Heuer G (1935) The effect of renal denervation on the level of arterial blood pressure and renal function in essential hypertension. J Clin Invest 14:27–30
Page I, Heuer G (1935) The effect of renal denervation on patients suffering from nephritis. J Clin Invest 14:443–458
Smithwick RH, Thompson JE (1953) Splanchnicectomy for essential hypertension: results in 1,266 cases. J Am Med Assoc 152:1501–1504
Grimson KS, Orgain ES, Anderson B, D’Angelo GJ (1953) Total thoracic and partial to total lumbar sympathectomy, splanchnicectomy and celiac ganglionectomy for hypertension. Ann Surg 138:532–547
Esler M (2010) The 2009 Carl Ludwig Lecture: pathophysiology of the human sympathetic nervous system in cardiovascular diseases: the transition from mechanisms to medical management. J Appl Physiol 108:227–237
Böhm M, Linz D, Ukena C et al (2014) Renal denervation for the treatment of cardiovascular high risk-hypertension or beyond? Circ Res 115:400–409
Vogl A (1950) The discovery of the organic mercurial diuretics. Am Heart J 39:881–883
Freis ED, Wanko A, Wilson IM, Parrish AE (1958) Treatment of essential hypertension with chlorothiazide (diuril): Its use alone and combined with other antihypertensive agents. J Am Med Assoc 166:137–140
Muschaweck R, Hajdú P (1964) Die salidiuretische Wirksamkeit der Chlor-N-(2-furylmethyl)5-sulfamy-anthranilsäure. Arzneimittelforschung 14:44–47
Moyer J (1954) Cardiovascular and renal hemodynamic response to reserpine (serpasil), and clinical results of using this agent for the treatment of hypertension. Ann N Y Acad Sci 59:82–94
Day M, Rand M (1963) A hypothesis for the mode of action of alpha-methyldopa in relieving hypertension. J Pharm Pharmacol 15:221–224
Hoefke W, Kobinger W (1966) Pharmakologische Wirkungen des 2-(2,6-Dichlorophenylamino)-2-Imidazolin-hydrochlorids, einer neuen antihypertensiven Substanz. Arzneimittelforschung 16:1038–1050
Tigerstedt R, Bergmann P (1898) Niere und Kreislauf. Scand Arch Physiol 7–8:223–271
Lindner E (1960) Phenyl-propyl-diphenyl-propyl-amin, eine neue Substanz mit coronargefäßerweiternder Wirkung. Arzneimittelforschung1 10:569–573
Fleckenstein A (1964) Die Bedeutung der energiereichen Phosphate für Kontraktilität und Tonus des Myokards. Verh Dtsch Ges Inn Med 70:81–99
Mills KT, Bundy JD, Kelly TN et al (2016) Global disparities of hypertension prevalence and control—global disparities of hypertension prevalence and control a systematic analysis of population-based studies from 90 countries. Circulation 134:441–450
Kearney PM, Whelton M, Reynolds K et al (2005) Global burden of hypertension: analysis of worldwide data. Lancet 365:217–223
Lawes CMM, Rodgers A, Bennett D et al (2003) Blood pressure and cardiovascular disease in the Asia Pacific region. J Hypertens 21:707–716
Rapsomaniki E, Timmis A, George J et al (2014) Blood pressure and incidence of twelve cardiovascular diseases: Lifetime risks, healthy life-years lost, and age-specific associations in 1·25 million people. Lancet 383:1899–1911
Parati G, Stergiou G, O’Brien E et al (2014) European society of hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens 32:1359–1366
Sheppard JP, Holder R, Nichols L et al (2014) Predicting out-of-office blood pressure level using repeated measurements in the clinic: an observational cohort study. J Hypertens 32:2171–2178
Kjeldsen SE, Lund-Johansen P, Nilsson PM, Mancia G (2016) Unattended blood pressure measurements in the systolic blood pressure intervention trial: Implications for entry and achieved blood pressure values compared with other trials. Hypertension 67:808–812
Mancia G, Verdecchia P (2015) Clinical value of ambulatory blood pressure: evidence and limits. Circ Res 116:1034–1045
Banegas JR, Ruilope LM, de la Sierra A et al (2018) Relationship between clinic and ambulatory blood-pressure measurements and mortality. N Engl J Med 378:1509–1520
SPRINT Research Group, Wright JT, Williamson JD, et al (2015) A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 373:2103–2116
Thomopoulos C, Parati G, Zanchetti A (2014) Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens 32:2285–2295
Böhm M, Schumacher H, Teo KK et al (2017) Achieved blood pressure and cardiovascular outcomes in high-risk patients: results from ONTARGET and TRANSCEND trials. Lancet 389:2226–2237
Williams B, Mancia G, Spiering W et al (2018) 2018 ESH/ESC Guidelines for the management of aterial hypertension. Eur Heart J (unpublished)
Vidal-Petiot E, Ford I, Greenlaw N et al (2016) Cardiovascular event rates and mortality according to achieved systolic and diastolic blood pressure in patients with stable coronary artery disease: an international cohort study. Lancet 388:2142–2152
Böhm M, Schumacher H, Teo KK et al (2018) Achieved diastolic blood pressure and pulse pressure at target systolic blood pressure (120–140 mmHg) and cardiovascular outcomes in high-risk patients: results from ONTARGET and TRANSCEND trials. Eur Heart J. https://doi.org/10.1093/eurheartj/ehy287
Psaty BM, Lumley T, Furberg CD et al (2003) Health outcomes associated with various antihypertensive therapies used as first-line agents: a network meta-analysis. J Am Med Assoc 289:2534–2544
Costanzo P, Perrone-Filardi P, Petretta M et al (2009) Calcium channel blockers and cardiovascular outcomes: a meta-analysis of 175,634 patients. J Hypertens 27:1136–1151
Van Vark LC, Bertrand M, Akkerhuis KM et al (2012) Angiotensin-converting enzyme inhibitors reduce mortality in hypertension: A meta-analysis of randomized clinical trials of renin–angiotensin–aldosterone system inhibitors involving 158 998 patients. Eur Heart J 33:2088–2097
Turnbull F, Neal B, Algert C et al (2005) Effects of different blood pressure-lowering regimens on major cardiovascular events in individuals with and without diabetes mellitus: results of prospectively designed overviews of randomized trials. Arch Intern Med 165:1410–1419
Mancia G, Fagard R, Narkiewicz K et al (2013) 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 34:2159–2219
Whelton PK, Carey RM, Aronow WS et al (2017) 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary. Hypertension 71(6):1269–1324
Ogihara T, Saruta T, Rakugi H et al (2010) Target blood pressure for treatment of isolated systolic hypertension in the elderly: valsartan in elderly isolated systolic hypertension study. Hypertension 56:196–202
Law MR, Morris JK, Wald NJ (2009) Use of blood pressure lowering drugs in the prevention of cardiovascular disease: Meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ 338:b1665
Dahlof B, Devereux BR, Kjeldsen SE (2002) Cardiovascular morbidity and mortality in the losartan intervention for end point reduction in hypertension study (LIFE): a randomised trial against atenolol. ACC Curr J Rev 11:26
Silvestri A, Galetta P, Cerquetani E et al (2003) Report of erectile dysfunction after therapy with beta-blockers is related to patient knowledge of side effects and is reversed by placebo. Eur Heart J 24:1928–1932
Calhoun D, Jones D, Textor S et al (2008) Resistant hypertension: diagnosis, evaluation, and treatment: a scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Circulation 117:e510–e526
Egan BM, Zhao Y, Axon RN et al (2011) Uncontrolled and apparent treatment resistant hypertension in the United States, 1988 to 2008. Circulation 124:1046–1058
Krieger EM, Drager LF, Giorgi DMA et al (2018) Spironolactone versus clonidine as a fourth-drug therapy for resistant hpertension novelty and significance. Hypertension 71:681–690
Williams B, Macdonald TM, Morant S et al (2015) Spironolactone versus placebo, bisoprolol, and doxazosin to determine the optimal treatment for drug-resistant hypertension (PATHWAY-2): a randomised, double-blind, crossover trial. Lancet 386:2059–2068
Václavík J, Sedlák R, Plachý M et al (2011) Addition of spironolactone in patients with resistant arterial hypertension (ASPIRANT): a randomized, double-blind, placebo-controlled trial. Hypertension 57:1069–1075
Schulz M, Krueger K, Schuessel K et al (2016) Medication adherence and persistence according to different antihypertensive drug classes: A retrospective cohort study of 255,500 patients. Int J Cardiol 220:668–676
Berra E, Azizi M, Capron A et al (2016) Evaluation of adherence should become an integral part of assessment of patients with apparently treatment-resistant hypertension. Hypertension 68:297–306
Gupta P, Patel P, Štrauch B et al (2017) Risk factors for nonadherence to antihypertensive treatment. Hypertension 69:1113–1120
Wald DS, Law M, Morris JK et al (2009) Combination therapy versus monotherapy in reducing blood pressure: meta-analysis on 11,000 participants from 42 trials. Am J Med 122:290–300
Chow CK, Thakkar J, Bennett A et al (2017) Quarter-dose quadruple combination therapy for initial treatment of hypertension: placebo-controlled, crossover, randomised trial and systematic review. Lancet 389:1035–1042
Bobrow K, Farmer AJ, Springer D et al (2016) Mobile phone text messages to support treatment adherence in adults with high blood pressure (SMS-Text Adherence Support [StAR]): a single-blind, randomized trial. Circulation 133:592–600
McNaughton CD, Brown NJ, Rothman RL et al (2017) Systolic blood pressure and biochemical assessment of adherence: a cross-sectional analysis in the emergency department. Hypertension 70:307–314
Gupta P, Patel P, Štrauch B et al (2017) Biochemical screening for nonadherence is associated with blood pressure reduction and improvement in adherence. Hypertension 70:1042–1048
Donazzan L, Mahfoud F, Ewen S et al (2016) Effects of catheter-based renal denervation on cardiac sympathetic activity and innervation in patients with resistant hypertension. Clin Res Cardiol 105:364–371
Hering D, Marusic P, Walton AS et al (2014) Sustained sympathetic and blood pressure reduction 1 year after renal denervation in patients with resistant hypertension. Hypertension 64:118–124
Ewen S, Zivanovic I, Böhm M, Mahfoud F (2015) Catheter-based renal denervation for hypertension treatment: update 2015. Eur Heart J 37:930–933
Mahfoud F, Böhm M, Azizi M et al (2015) Proceedings from the European clinical consensus conference for renal denervation: considerations on future clinical trial design. Eur Heart J 36:2219–2227
Böhm M, Mahfoud F, Ukena C et al (2015) First report of the global SYMPLICITY registry on the effect of renal artery denervation in patients with uncontrolled hypertension. Hypertension 65:766–774
De Jager RL, Sanders MF, Bots ML et al (2016) Renal denervation in hypertensive patients not on blood pressure lowering drugs. Clin Res Cardiol 105:755–762
Sharp ASP, Davies JE, Lobo MD et al (2016) Renal artery sympathetic denervation: observations from the UK experience. Clin Res Cardiol 105:544–552
Bhatt DL, Kandzari DE, O’Neill WW et al (2014) A controlled trial of renal denervation for resistant hypertension. N Engl J Med 370:1393–1401
Pathak A, Ewen S, Fajadet J et al (2014) From symplicity HTN-3 to the renal denervation global registry: where do we stand and where should we go. EuroIntervention 10:21–24
Azizi M, Sapoval M, Gosse P et al (2015) Optimum and stepped care standardised antihypertensive treatment with or without renal denervation for resistant hypertension (DENERHTN): a multicentre, open-label, randomised controlled trial. Lancet 385:1957–1965
Ewen S, Meyer MR, Cremers B et al (2015) Blood pressure reductions following catheter-based renal denervation are not related to improvements in adherence to antihypertensive drugs measured by urine/plasma toxicological analysis. Clin Res Cardiol 104:1097–1105
Azizi M, Pereira H, Hamdidouche I et al (2016) Adherence to antihypertensive treatment and the blood pressure-lowering effects of renal denervation in the renal denervation for hypertension (DENERHTN) trial. Circulation 134:847–857
Kandzari DE, Kario K, Mahfoud F et al (2016) The SPYRAL HTN Global Clinical Trial Program: rationale and design for studies of renal denervation in the absence (SPYRAL HTN OFF-MED) and presence (SPYRAL HTN ON-MED) of antihypertensive medications. Am Heart J 171:82–91
Ewen S, Ukena C, Linz D et al (2015) Reduced effect of percutaneous renal denervation on blood pressure in patients with isolated systolic hypertension. Hypertension 65:193–199
Mahfoud F, Bakris G, Bhatt DL et al (2017) Reduced blood pressure-lowering effect of catheter-based renal denervation in patients with isolated systolic hypertension: Data from SYMPLICITY HTN-3 and the Global SYMPLICITY Registry. Eur Heart J 38:93–100
Mahfoud F, Tunev S, Ewen S et al (2015) Impact of lesion placement on efficacy and safety of catheter-based radiofrequency renal denervation. J Am Coll Cardiol 66:1766–1775
Townsend RR, Mahfoud F, Kandzari DE et al (2017) Catheter-based renal denervation in patients with uncontrolled hypertension in the absence of antihypertensive medications (SPYRAL HTN-OFF MED): a randomised, sham-controlled, proof-of-concept trial. Lancet 390:2160–2170
Kandzari DE, Böhm M, Mahfoud F et al (2018) Effect of renal denervation on blood pressure in the presence of antihypertensive drugs: 6-month efficacy and safety results from the SPYRAL HTN-ON MED proof-of-concept randomised trial. Lancet 6736:1–10
Azizi M, Schmieder RE, Mahfoud F et al (2018) Endovascular ultrasound renal denervation to treat hypertension (RADIANCE-HTN SOLO): a multicentre, international, single-blind, randomised, sham-controlled trial. Lancet 6736:1–11
Scheffers IJM, Kroon AA, Schmidli J et al (2010) Novel baroreflex activation therapy in resistant hypertension: results of a European multi-center feasibility study. J Am Coll Cardiol 56:1254–1258
De Leeuw PW, Bisognano JD, Bakris GL et al (2017) Sustained reduction ofbBlood pressure with baroreceptor activation therapy: results of the 6-year open follow-up. Hypertension 69:836–843
Ewen S, Böhm M, Mahfoud F (2017) Long-term follow-up of baroreflex activation therapy in resistant hypertension: Another piece of the puzzle? Hypertension 69:782–784
Lobo MD, Sobotka PA, Stanton A et al (2015) Central arteriovenous anastomosis for the treatment of patients with uncontrolled hypertension (the ROX CONTROL HTN study): a randomised controlled trial. Lancet 385:1634–1164
Ewen S, Lauder L, Böhm M, Mahfoud F (2018) Real-time left ventricular pressure-volume loops during percutaneous central arteriovenous anastomosis. Eur Heart J (Epub ahead of press)
Lobo MD, Ott C, Sobotka PA et al (2017) Central iliac arteriovenous anastomosis for uncontrolled hypertension: one-year results from the ROX CONTROL HTN Trial. Hypertens (Dallas. Tex 1979) 70:1099–1105
Spiering W, Williams B, Van der Heyden J et al (2017) Endovascular baroreflex amplification for resistant hypertension: a safety and proof-of-principle clinical study. Lancet 390:2655–2661
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wolf, M., Ewen, S., Mahfoud, F. et al. Hypertension: history and development of established and novel treatments. Clin Res Cardiol 107 (Suppl 2), 16–29 (2018). https://doi.org/10.1007/s00392-018-1299-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-018-1299-y