Abstract
Purpose
Surgery is the standard of care for resectable colorectal liver metastases (CRC-LM). Unfortunately, 60 % of patients develop secondary metastatic recurrence (SMR) after R0-resection of CRC-LM. We investigated the impact of surgical re-intervention and chemotherapy (Ctx) on survival in a consecutive series of patients with SMR.
Methods
From 01/2001 to 11/2011, 104 out of 178 consecutive patients with R0-resection of CRC-LM developed SMR and were evaluated. The impact of surgical and Ctx re-interventions on recurrence free (RFS) and cancer-specific survival (CSS) was analyzed. Median follow-up was 28.0 (95 %CI: 19.4–37.4) months.
Results
SMR occurred in 81 patients at a single site (49× liver, 18× lung, 14× other) and in 23 patients at multiple sites. Forty-two patients were scheduled for primary surgery. Fifty-three patients were classified as non-resectable and treated with median 5.0 [IQR, 3.0–10.0] cycles of Ctx, combined with an EGFR/VEGF-antibody in 27 patients. Nine patients received best supportive care only. R0/R1 resection could be achieved in 35 patients primarily and even in 8 patients secondarily after Ctx. Surgical morbidity and mortality were 16 and 0 %, respectively. The 5-year RFS rates for patients with R0 versus R1-resection were 22 and 24 % (p = 0.948). The 5-year CSS rate for R0/R1-resected patients was 38 % versus 10 % for those patients treated by Ctx alone (p < 0.001).
Conclusion
In SMR, surgical re-intervention is feasible and safe in a remarkable number of patients and offers significantly longer CSS compared to patients without resection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Distant metastases are the predominant mode of failure of adjuvant or neoadjuvant multimodal treatment in CRC. More than 50 % of CRC patients experience distant metastases during the course of malignancy and the liver represents the predominant site of first metastatic relapse (CRC-LM). Regarding international guidelines, there is interdisciplinary consensus that complete (R0) resection is the only curative option in the treatment of patients with CRC-LM [1]. Five-year overall survival (OS) rates up to 58 % have been reported by specialized centers [2], but primary liver resection is an option only in 20 % of patients [3]. However, innovative treatment approaches like preoperative intensive intravenous chemotherapy (Ctx) combined with targeted therapy (CELIM trial [4]) and two-stage liver resection with portal vein ligation [5, 6] have achieved secondary resectability in 28–75 % of patients, initially deemed non-resectable. Recently, the updated survival analysis of the CELIM trial has shown a higher median OS of 46.7 months for R0-resected patients compared to 27.3 months for non-resectable patients (p = 0.002). These data demonstrate that a Ctx-induced conversion to secondary resectability is not only a technical issue but also associated with a survival benefit [7].
Unfortunately, approximately 60 % of patients develop early second metastatic recurrence (SMR) within 3 years after the first liver resection [8]. The main sites of these SMR are the liver or the lung but in 30 % of patients multiple sites can be affected [9]. Previous studies have demonstrated that in selected patients re-resection of isolated hepatic [10–14] or pulmonal [15, 16] SMR might result not only in encouraging survival rates similar to those after resection of the first metastatic recurrence but also in higher quality of life compared to continued palliative Ctx [17]. In their single-center experience, Adam et al. have even demonstrated a 5-year OS of 34 % after the third hepatectomy for recurrent liver metastases [18]. Therefore, efforts need to be focused on optimizing multidisciplinary treatment regimens to increase the number of patients suitable for resection of SMR. However, there is very rare evidence on the impact of surgery and Ctx in a consecutive cohort of patients suffering from SMR after previous R0-resection of first CRC-LM.
Therefore, in the present single-center study, we analyzed the feasibility as well as impact of surgical re-intervention and Ctx on survival in a series of consecutive patients with SMR.
Material and methods
Study population
From 01/2001 to 08/2011, 178 patients with liver-only colorectal metastasis (CRM) underwent histopathologically confirmed complete resection (R0-status was defined as tumor free resection margin ≥0.1 cm) of all CRC-LM at the Department of General and Visceral Surgery, University Medical Center Göttingen. Until the last date of observation (November 30th 2011), 104 of these patients developed SMR within a median recurrence free interval of 7.5 (95 %CI, 1.0–34.4) months. These patients represent the actual study cohort. All patient data had been prospectively collected in a database and study related procedures were approved by the local ethics committee and in accordance with the Helsinki Declaration of 1975, as revised in 2008.
Table 1 summarizes the clinicopathological data of all 104 patients including treatment procedures of both, the primary tumor and the first CRC-LM. Before resection of CRC-LM the standardized staging covered clinical examination, serum level of carcinoembryonic antigen (CEA), chest-X-ray or thoracic computed tomography (CT), contrast-enhanced abdominal CT or magnetic resonance imaging (MRI) and starting from 2006 on a fluorodeoxyglucose (18F)-positron emissions tomography (FDG-PET). Standard treatment recommendation after first liver resection was a “wait and see”-strategy according to national S3-guidelines [19]. Despite this fact, 35 patients were treated by anti-CEA-radioimmunotherapy with 131I-labetuzumab [20, 21] and 20 patients by Ctx according to the discretion of the interdisciplinary tumor board or referring oncologist. Prior to detection of SMR, 45 of 104 patients had received ≥2 systemic anticancer therapies (Ctx or radioimmunotherapy) for either the primary tumor and/or the CRC-LM.
After diagnosis of SMR staging procedures were concordant to those mentioned above. Given that there are neither controlled trials nor established guidelines for the treatment of SMR, interdisciplinary decision making in individual patients considered extent of disease, performance status, comorbidity, patients’ preference and investigators as well as institutional experience. Primary resection of SMR was intended only in patients with localized single-site recurrences. When non-resectability or unfavorable tumor biology, in particular rapid progression was expected, Ctx was indicated with re-evaluation for secondary resectability at regular intervals. Tumor response to Ctx was measured using the Response Evaluation Criteria In Solid Tumors criteria and classified as complete response, partial response, stable disease or progressive disease [22]. Resection of SMR was performed according to established surgical operating procedures. Intraoperative ultrasound was used routinely in all patients scheduled for repeated liver resection to detect occult hepatic CRM. Cases with intraoperative open radiofrequency ablation of single liver lesions in addition to surgery were classified as incomplete (R1) resection. Median follow-up interval from time of SMR diagnosis to last observation was 28.0 (95 %CI, 19.4–37.4) months.
Statistical analysis
Statistical analysis was performed using the Statistical Computing Software R (Free statistical software R, version 2.12.2, www.r-project.org). Recurrence free survival (RFS) was calculated only for those patients who experienced R0/R1-resection of SMR. Cancer-specific survival (CSS) was calculated from the date SMR had been diagnosed on time to cancer-specific death using the R package survival. Median survival data have to be interpreted as time to 50 % at risk. Survival data was visualized using Kaplan–Meier plots and significance was calculated using the Cox Proportional Hazards Model. Significance for comparison between groups was calculated using Fisher’s Exact Test for categorical variables or variables that were discretized (e.g., gender, tumor stage, type of therapy) and using the Wilcoxon Test for numeric variables (e.g., age, size of metastasis). p values < 0.05 were considered significant.
Results
Pattern of recurrence
The liver was the predominant site of second metastatic recurrence (n = 49). The second most common site was the lung (n = 18). Other localizations of single-site recurrences were abdominal/retroperitoneal lymph nodes (n = 4), locally in the small pelvis (n = 4), peritoneal (n = 3), cerebral (n = 2) and osseous (n = 1). Eleven patients developed simultaneous liver and lung recurrences. Other coincidental localizations included lung and brain (n = 3), lung and abdominal/retroperitoneal lymph nodes (n = 2) and other double and triple combinations in 7 additional patients. The pattern of SMR was not significantly different between those patients who initially had unilobar versus those who had bilobar CRC-LM (p = 0.554).
Treatment of second metastatic recurrence
The treatment algorithm of SMR for the whole study cohort is shown in Fig. 1. Forty-two of 104 patients were scheduled for primary resection of SMR while 53 patients were determined as non-resectable and treated by palliative Ctx. Nine patients denied any further therapy or the performance status was too poor for either surgery or Ctx. Therefore, these patients received best supportive care only.
Therapy algorithm for second metastatic recurrence. Primary and secondary R0/R1-resection could be achieved in 35 and 8 patients, respectively. The nine patients with R2-resection were postoperatively treated by palliative chemotherapy (n = 6), radiotherapy (n = 1) or chemotherapy with hyperthermia (n = 1) while one patient denied further therapy. CRC colorectal cancer
Detailed treatment data for all patients except those treated by best supportive care are displayed in Table 2. In seven patients scheduled for resection of SMR intraoperative findings prevented macroscopically complete resection because of occult disseminated peritoneal carcinomatosis (n = 2), extended lymph node metastases (n = 2), unresectable progressive disease following portal vein ligation (n = 1), inadequate remnant liver volume after previous extended hemihepatectomy and Ctx with oxaliplatin (n = 1) and adjacence to vital cerebral structures (n = 1). All these seven patients received palliative therapy. In detail, five patients were further treated by palliative Ctx, one patient with lymph node metastases requested Ctx with hyperthermia, and one patient suffering from cerebral metastasis received cerebral radiotherapy alone.
Of those 53 patients treated by Ctx, 19 had multi-site SMR and additional six patients had disseminated peritoneal, lymphatic, or osseous disease. Patients who received Ctx without either oxaliplatin or irinotecan were treated in the early study period. As a result of Ctx, three patients had complete radiographic remission of their metastases but developed third metastatic disease during follow-up (wait and watch strategy) localized at previous sites in all three patients. Partial response or at least stable disease was achieved in 16 patients. Of these 16 patients, 10 were scheduled for surgical exploration. Four of the remaining six patients had potentially resectable disease too, but three patients refused surgical re-intervention and 1 patient preferred brachytherapy of his residual metastases. In all ten patients scheduled for surgery, histopathologically confirmed R0-resection of targeted locoregional lesions could be achieved. Nevertheless, two cases were classified as incomplete (R2) resection because metastases at additional sites were not resected. In detail, one patient with hepatic and pulmonary SMR had divergent response to Ctx with stable liver metastases but slightly progressive pulmonary metastases. Based on good performance status and patients’ request all pulmonary lesions were resected by bilateral thoracotomy. Postoperatively, the patient received Ctx and was alive as of the last observation. A second patient had pulmonary and cerebral metastases and experienced resection of cerebral metastases only as the lung metastases remained in stable disease status. However, this patient suffered from cerebral recurrence and died 22 months after surgery. The residuary 33 patients, classified as non-resectable for SMR, had progressive disease under continued Ctx and received up to five lines of palliative Ctx.
To identify differences in CRC biology and disease stage between the subgroups (primary resection, secondary resection, Ctx only) we performed pairwise comparisons for SMR-related parameters, in particular RFS (from previous liver resection to diagnosis of SMR) and number as well as largest diameter of SMR (Table 3). RFS and number of lesions were not statistically different distributed between the subgroups. The diameter of metastases was significantly greater in patients treated by Ctx only compared to those with primary resection of SMR (p = 0.0465). Furthermore, metastatic affection of multiple sites was more often in patients treated by Ctx only compared to patients with primary or secondary resection (p < 0.001).
Survival
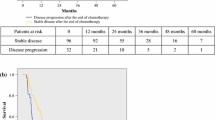
RFS rates were calculated for patients with R0- and R1-status after resection of SMR. The 5-year RFS rates between R0 and R1 status were nearly identical with 22 versus 24 %, respectively (p = 0.948, Fig. 2a). During follow-up, one patient with non-resectable intrahepatic relapse and three patients without evidence of recurrent disease died non-cancer related. For comparison of CSS rates between different oncological treatment procedures, all patients receiving best supportive care were excluded. Patients receiving potentially curative resection (R0/R1) of SMR had a 5-year survival rate of 38 % versus 10 % for patients with non-resectable malignancy continuously treated by palliative Ctx alone (p < 0.001, Fig. 2b).
Kaplan–Meier curve for recurrence free and cancer-specific overall survival. a Recurrence free survival for patients with R0 versus R1 resection of second metastatic recurrence (n = 43). Five-year RFS rates for R0- and R1-resected patients were 22 and 24 % (p = 0.948). b Overall cancer-specific survival for patients with R0/R1 resection versus R2-resection + palliative chemotherapy/palliative chemotherapy only for second metastatic disease (n = 95). Five-year CSS rate was 38 % for R0/R1-resected patients versus 10 % for patients treated by palliative chemotherapy (p < 0.001)
Discussion
During the last 10 years, treatment options in patients with metastatic colorectal cancer have been evolved by initiation of multidisciplinary therapeutic strategies. Most of these are using modern chemotherapeutic regimens including agents for targeted therapy as well as extended surgery to remove (residual) metastases. Thereby, the number of primarily or secondarily resected patients is increasing. Given that approximately two thirds of these patients experience relapse again, surgeons as well as medical oncologists are faced in clinical practice with a growing number of patients with SMR requesting further treatment. Therefore, data on what can be achieved in these patients by surgery and/or Ctx are needed.
Our single-center series of consecutive patients after R0-resection of CRC-LM has shown that repeated resection of SMR is feasible and safe in 40 % of patients. After re-resection of SMR patients showed a significantly longer CSS compared to non-resected patients treated by palliative Ctx alone.
Pattern of recurrence and previous oncological treatment
The pattern of SMR observed in our series was comparable to previous reports [8, 9, 23]. Stratifying patients according to the hepatic spread (unilobar versus bilobar) of initial CRC-LM, we could not observe the expected higher rate of intrahepatic SMR in the bilobar cohort. Repeated liver resection needed to be canceled only in one patient due to small remnant liver volume as reported. In contrast, in 10 of 28 patients with intrahepatic SMR scheduled for re-resection extended hemihepatectomies had been performed for initial CRC-LM. The postoperative course in all 28 patients was uneventful. In consequence, extended previous liver resections do not necessarily prohibit repeated resections for SMR as long as individual limitations, in particular liver tissue damage and involvement of vital anatomic structures are absent.
Treatment of second metastatic recurrence
There is very limited evidence on what can be recommended in patients with SMR. However, the goal of therapeutic intervention should be prolonged OS with acceptable quality of life and, if possible, without ongoing cytotoxic therapy. German guidelines [24] on the treatment of metastatic colorectal cancer do not include algorithms for patients with SMR after R0-resection of CRC-LM In contrast, the National Comprehensive Cancer Network guidelines mention that SMR limited to either liver or lung can be considered for re-resection in selected patients [25]. The crucial aspect of reasonable weighting treatment decisions is how to interpret the occurrence of SMR. Premature data from the SECA-trial evaluating the impact of liver transplantation in selected patients with unresectable CRC-LM showed that different from patients after resection of CRC-LM the majority of patients treated by liver transplantation developed extrahepatic recurrence [26]. These data support the hypothesis that to a certain extent occurrence of SMR more likely represents outgrowth of previously occult micrometastases instead of increasing aggressiveness. Therefore, when resection is the standard in initial CRC-LM, it would be consequent to aim for resection in SMR as well. Given that only 20 % of initial CRC-LM are considered resectable [3], our primary resection rate of 34 % in patients with SMR is encouraging. Resection rate and low morbidity, which has also been reported by Brachet et al. [27], further support multimodal treatment concepts including repeated surgery in patients suffering from SMR.
In the setting of initially unresectable CRC-LM Ctx-related conversion rates of 38–60 % to secondary resectability have been observed by using monoclonal EGFR/VEGF-antibodies in addition to Ctx [4, 28, 29]. In our study, secondary resection of SMR was performed in 15 % of patients initially treated with Ctx. Considering that four additional patients had resectable disease after Ctx, the percentage of resectable patients in this cohort even raised up to 23 %. However, monoclonal EGFR/VEGF-antibodies were introduced into clinical routine not until the second half period of the present study. We hypothesize that an even larger proportion of patients would qualify for secondary resection by using intensified Ctx protocols as investigated for example in the CELIM trial [8].
Although van der Pool et al. [30] found no difference in survival between patients with recurrent hepatic CRM treated by either RFA or liver resection, we classified patients sufficiently treated by RFA as R1 (n = 5). A further four patients classified with R1-status had liver resections with the tumor being adjacent to remnant liver veins (n = 2), resection of local recurrence limited by the sacrum (n = 1) and resection of local peritoneal carcinomatosis (n = 1). In all these patients, macroscopically complete resection was achieved. De Haas et al. [31] reported that survival following R1-liver resection is comparable to R0-resection. RFS in our nine patients classified as R1 was not significantly different compared to R0-resected patients. Therefore, we grouped patients with R0 and R1-resection together for CSS analysis and observed a significantly longer CSS compared to patients treated by palliative Ctx only. In concordance with Mise et al. [32] who evaluated resection in selected patients with single and multiple sites SMR, we consider a survival benefit when resection of SMR can be achieved.
Very recently, Hill et al. [33] proposed a scoring system to predict survival in patients with SMR based on three different parameters: CEA > 200 ng/ml, >1 liver metastases and >5 cm liver metastases. Such scoring system would be very useful to stratify patients into different treatment concepts in particular primary resection versus preoperative chemotherapy. As we observed significant influence of treatment on survival, we advocate validating this initial experience in a larger independent patient cohort including treatment data.
It should be noted that the data of this retrospective study on patients in this advanced stage of disease with SMR are biased. Patients were not prospectively randomized into different treatment arms. The indication for the chemotherapy regimens was based on tumor biology (progression), toxicity and efficacy of previously applied therapies, introduction of innovative agents into clinical routine and physicians’ discretion (multidisciplinary tumor board decision). However, in contrast to previous reports focusing on highly selected patients we present a consecutive series of patients with SMR. All patients have been treated in our center after introduction of advanced surgical techniques. The treatment decisions were consistently made by the same multidisciplinary team. Thereby, patients with resectable and non-resectable SMR were included and randomization could not be realized. Addressing disease aggressiveness, multiple site recurrences were significantly more frequent in the Ctx only group. However, although first-line trials suggest that multiple site recurrences have poorer survival compared to single-site recurrences [34] these data have not been confirmed in a well described patient cohort with SMR treated in a multimodality concept including resection. Pairwise comparisons between the study groups (Table 3) showed that parameters expressing more aggressive disease were mainly balanced. Therefore, selection bias considering patients with more favorable tumor biology or lower tumor load for primary resection seems to be unlikely. Recently, the meta-analysis of Gonzales et al. did not find a significant impairment of survival by previous liver resection for concomitant liver metastases compared to lung only metastases [35].
Conclusion
Surgical re-intervention is a feasible and safe treatment option in a remarkable number of patients with SMR following R0-resection of CRC-LM. Secondary resection after Ctx is possible in a remarkable proportion of patients initially deemed to be non-resectable. In our single-center series, patients who were treated within a multidisciplinary concept including R0/R1-resection of SMR had a significantly longer CSS compared to those who were treated by Ctx only. Therefore, all patients with SMR after R0-resection of CRC-LM should be discussed in a multidisciplinary team prior to any treatment onset. The possibility of repeated surgical intervention needs to be assessed by a surgeon experienced in oncological strategies as well as liver surgery.
References
Abdalla EK, Adam R, Bilchik AJ, Jaeck D, Vauthey JN, Mahvi D (2006) Improving resectability of hepatic colorectal metastases: expert consensus statement. Ann Surg Oncol 13:1271–1280
Abdalla EK, Vauthey JN, Ellis LM et al (2004) Recurrence and outcomes following hepatic resection, radiofrequency ablation, and combined resection/ablation for colorectal liver metastases. Ann Surg 239:818–827
Hackl C, Gerken M, Loss M, Klinkhammer-Schalke M, Piso P, Schlitt HJ (2011) A population-based analysis on the rate and surgical management of colorectal liver metastases in Southern Germany. Int J Colorectal Dis 26:1475–1481
Folprecht G, Gruenberger T, Bechstein WO et al (2010) Tumour response and secondary resectability of colorectal liver metastases following neoadjuvant chemotherapy with cetuximab: the CELIM randomised phase 2 trial. Lancet Oncol 11:38–47
Homayounfar K, Liersch T, Schuetze G et al (2009) Two-stage hepatectomy (R0) with portal vein ligation-towards curing patients with extended bilobar colorectal liver metastases. Int J Colorectal Dis 24:409–418
Jaeck D, Oussoultzoglou E, Rosso E, Greget M, Weber JC, Bachellier P (2004) A 2-stage hepatectomy procedure combined with portal vein embolization to achieve curative resection for initially unresectable multiple and bilobar colorectal liver metastases. Ann Surg 240:1037–1051
Folprecht G, Gruenberger T, Bechstein WO et al (2012) Survival with cetuximab/FOLFOX or cetuximab/FOLFIRI of patients with nonresectable colorectal liver metastases in the CELIM study. J Clin Oncol (suppl 4; abstr 540)
De Jong MC, Pulitano C, Ribero D et al (2009) Rates and patterns of recurrence following curative intent surgery for colorectal liver metastases. Ann Surg 250:440–448
D’Angelica M, Kornprat P, Gonen M, DeMatteo RP, Fong Y, Blumgart LH, Jarnagin WR (2011) Effect on outcome of recurrence patterns after hepatectomy for colorectal metastases. Ann Surg Oncol 18:1096–1103
Ishiguro S, Akasu T, Fujimoto Y et al (2006) Second hepatectomy for recurrent colorectal liver metastasis: analysis of preoperative prognostic factors. Ann Surg Oncol 13:1579–1587
Yamamoto J, Kosuge T, Shimada K, Yamasaki S, Moriya Y, Sugihara K (1999) Repeat liver resection for recurrent colorectal liver metastases. Am J Surg 178:275–281
Shaw IM, Rees M, Welsh FKS, Brygrave S, John TG (2006) Repeat hepatic resection for recurrent colorectal liver metastases is associated with favrourable long-term survival. Br J Surg 93:457–464
Petrowsky H, Gonen M, Jarnagin W, Lorenz M, DeMatteo R, Heinrich S, Encke A, Blumgart L, Fong Y (2002) Second liver resections are safe and effective treatment for recurrent hepatic metastases from colorectal cancer. Ann Surg 235:863–871
Pessaux P, Lermite E, Brehant O, Tuech JJ, Lorimier G, Arnaud JP (2006) Repeat hepatectomy for recurrent colorectal liver metastases. J Surg Oncol 93:1–7
Borasio P, Gisabella M, Billé A, Righi L, Longo M, Tampellini M, Ardissone F (2011) Role of surgical resection in colorectal lung metastases: analysis of 137 patients. Int J Colorectal Dis 26:183–190
Park JS, Kim HK, Choi YS et al (2010) Outcomes after repeated resection for recurrent pulmonary metastases from colorectal cancer. Ann Oncol 21:1285–1289
Wiering B, Oyen WJG, Adang EMM et al (2011) Long-term global quality of life in patients treated for colorectal liver metastases. Br J Surg 98:565–571
Adam R, Pascal G, Azoulay D, Tanaka K, Castaing D, Bismuth H (2003) Liver resection for colorectal metastases. The third hepatectomy. Ann Surg 238:871–884
Schmiegel W, Pox C, Adler G et al (2004) S3-Guidelines Conference “Colorectal Carcinoma” 2004. Z Gastroenterol 42:1129–1177
Liersch T, Meller J, Bittrich M, Kulle B, Becker H, Goldenberg DM (2007) Update of carcinoembryonic antigen radioimmunotherapy with (131)I-labetuzumab after salvage resection of colorectal liver metastases: comparison of outcome to a contemporaneous control group. Ann Surg Oncol 14:2577–2590
Liersch T, Meller J, Sahlmann CO, Langer C, Ghadimi M, Becker H, Goldenberg DM (2009) Efficacy of repeated anti-CEA-radioimmunotherapy (RAIT) with 131iodine(I)-labetuzumab (phase-II study) in patients with colorectal cancer (CRC) after salvage resection of multiple liver metastases (CRLM). 2009 Gastrointestinal Cancers Symposium Proceedings; Abstract 459
Therasse P, Arbuck SG, Eisenhauer EA et al (2000) New guidelines to evaluate response to treatment in solid tumors. J Natl Cancer Inst 92:205–216
Vigano L, Ferrero A, Lo Tesoriere R, Capussotti L (2008) Liver surgery for colorectal metastases: results after 10 years of follow-up. Long-term survivors, late recurrences, and prognostic role of morbidity. Ann Surg Oncol 15:2458–2464
Schmiegel W, Reinacher-Schick A, Arnold D et al (2008) Update S3-guideline "colorectal cancer" 2008. Z Gastroenterol 46:799–840
NCCN Clinical practice guidelines in oncology: rectal cancer, version 3.2012. http://www.nccn.org/professionals/physician_gls/pdf/rectal.pdf (accessed 01/27/2012)
Dueland S, Hagness M, Line PD et al (2012) Liver transplantation (Ltx) in patients with nonresectable liver metastases from colorectal carcinoma. J Clin Oncol; (suppl 4; abstr 577)
Brachet D, Lermite E, Rouquette A, Lorimier G, Hamy A, Arnaud JP (2009) Prognostic factors of survival in repeat liver resection for recurrent colorectal metastases: review of sixty-two cases treated at a single institution. Dis Colon Rectum 52:475–483
Masi G, Loupakis F, Salvatore L et al (2010) Bevacizumab with FOLFOXIRI (irinotecan, oxaliplatin, fluorouracil, and folinate) as first-line treatment for metastatic colorectal cancer: a phase 2 trial. Lancet Oncol 11:845–852
Garufi C, Torsello A, Tumolo S et al (2010) Cetuximab plus chronomodulated irinotecan, 5-fluorouracil, leucovorin and oxaliplatin as neoadjuvant chemotherapy in colorectal liver metastases: POCHER trial. Br J Cancer 103:1542–1547
Van der Pool AEM, Lalmahomed ZS, de Wilt JHW, Eggermont AMM, Ijzermans JMN, Verhoef C (2009) Local treatment for recurrent colorectal hepatic metastases after partial hepatectomy. J Gastrointest Surg 13:890–895
De Haas RJ, Wicherts DA, Flores E, Azoulay D, Castaing D, Adam R (2008) R1 resection by necessity for colorectal liver metastases: is it still a contraindication to surgery? Ann Surg 248:626–637
Mise Y, Imamura H, Hashimoto T et al (2010) Cohort study of the survival benefit of resection for recurrent hepatic and/or pulmonary metastases after primary hepatectomy for colorectal metastases. Ann Surg 251:902–909
Hill CR, Chagpar RB, Callender GG et al (2012) Recurrence following hepatectomy for metastatic colorectal cancer: development of a model that predicts patterns of recurrence and survival. Ann Surg Oncol 19:139–144
Kohne C, Bokemeyer C, Heeger S, Sartorius S, Rougier P, Van Cutsem E (2011) Efficacy of chemotherapy plus cetuximab according to metastatic site in KRAS wild-type metastatic colorectal cancer (mCRC): Analysis of CRYSTAL and OPUS studies. J Clin Oncol (suppl; abstr 3576)
Gonzalez M, Poncet A, Combescure C, Robert J, Ris HB, Gervaz P (2012) Risk factors for survival after lung metastasectomy in colorectal cancer patients: A systematic review and meta-analysis. Ann Surg Oncol. doi:10.1245/s10434-012-2726-3
Gayowski TJ, Iwatsuki S, Madariaga JR, Selby R, Todo S, Irish W, Starzl TE (1994) Experience in hepatic resection for metastatic colorectal cancer: analysis of clinical and pathologic risk factors. Surgery 116:703–710
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH (1999) Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer. Analysis of 1001 consecutive cases. Ann Surg 230:309–321
Nordlinger B, Guiguet M, Vaillant JC, Balladur P, Boudjema K, Bachellier P, Jaeck D (1996) Surgical resection of colorectal carcinoma metastases to the liver. A prognostic scoring system to improve case selection, based on 1568 patients. Cancer 77:1254–1262
Acknowledgments
This work has been generated as a collaboration project of the Clinical Research Unit 179 (Biological basis of individual tumor response in patients with rectal cancer, subproject 5) and the Research Unit 942 (FOR942 BE 2552/4-1), both funded by the German Research Council (DFG).
Conflict of interests
The authors declare that no conflicts of interest exist.
Author information
Authors and Affiliations
Corresponding author
Additional information
K. Homayounfar and A. Bleckmann contributed equally to this manuscript and study
T. Liersch and B.M. Ghadimi share senior authorship
Data have in part been presented at the 2012 ASCO Gastrointestinal Cancers Symposium, January 19–21 2012 in San Francisco, USA
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Homayounfar, K., Bleckmann, A., Conradi, L.C. et al. Metastatic recurrence after complete resection of colorectal liver metastases: impact of surgery and chemotherapy on survival. Int J Colorectal Dis 28, 1009–1017 (2013). https://doi.org/10.1007/s00384-013-1648-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-013-1648-2