Abstract
Purpose
The aim of this study is to investigate clinicopathologic characteristics and to identify prognostic factors in patients undergoing pulmonary metastasectomy for colorectal carcinoma.
Methods
This study is a single-institution retrospective study of 137 consecutive patients who underwent 158 pulmonary resections for metastatic colorectal carcinoma between January 1989 and June 2008.
Results
Median disease-free interval between colorectal resection and pulmonary metastasectomy was 35.6 months (range, 0.6 to 154.3 months). No perioperative deaths occurred. Follow-up was 100% complete and mean follow-up was 41.6 ± 27.6 months. Median survival was 36.2 months (range, 4.6 to 126 months). Overall 5- and 10-year survival rates were 55.4% and 30.8%, respectively, after pulmonary metastasectomy. At univariate analysis of patient survival, number of lung metastases (p = 0.002), disease-free interval of more than 24 month (p = 0.013), and absence of residual tumor (p = 0.024) were significant prognostic factors. At multivariate analysis, presence of solitary lung metastasis and disease-free interval of more than 24 months remained significant prognostic factors. There was no significant difference in the 5-year survival for 121 patients undergoing single thoracotomy compared with 16 patients undergoing repeated resection(s) for recurrent colorectal lung metastasis (55.1% vs 59.5%; p = 0.79). Nor was the presence of hepatic metastasis associated with lower outcome (p = 0.77).
Conclusions
Disease-free interval and number of metastases are the most significant prognostic factors for survival after pulmonary metastasectomy for colorectal carcinoma. Recurrent pulmonary disease can benefit from repeated resection. Prior hepatectomy for liver involvement does not influence survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal carcinoma (CRC) is a leading cause of cancer morbidity and mortality. In 2006, according to comprehensive estimates of cancer incidence and mortality in Europe [1], CRC was the second most common form of cancer (12.9% of all incident cases) and, despite recent improvements in age-adjusted 5-year survival [2], it was the second major cause of cancer mortality (12.2% of all cancer deaths), almost equally distributed between sexes.
Nearly two thirds of patients with CRC present localized disease and undergo surgery with potentially curative intent. However, 30–50% of these patients will develop a recurrence, mostly within 2 to 3 years of surgery and in the form of distant metastases [3, 4]. Patients with metastatic CRC face a dismal prognosis. The first site of recurrence is the liver, followed by the lung. Surgical resection of lung metastases of CRC is generally considered an effective treatment option for properly selected patients with resectable isolated lung metastases. Inconsistency in prognostic factors and lack of randomized outcome data remain, however, the main points of criticism of lung metastasectomy in patients with CRC [5, 6].
The aims of this study were to investigate clinicopathologic characteristics and to shed further light on factors influencing survival of patients undergoing pulmonary metastasectomy for CRC in order to identify which subset of patients can benefit optimally from surgery.
Patients and methods
Patient population
This is a single-institution retrospective study performed on a prospectively computerized database including 137 consecutive patients who underwent 158 pulmonary resections for metastatic CRC between January 1989 and June 2008. During this time period, a further 658 patients were clinically diagnosed as having pulmonary metastases from CRC unsuitable for surgical resection. The extent of metastatic disease precluded surgery in 569 (86.5%) of these patients. The remaining 89 patients were not selected for resection because of the following reasons: comorbidity and/or impaired pulmonary reserve (n = 48), refusal of surgery (n = 12), and not documented reason (n = 29). The institutional review board approved the study and informed consent was obtained from all included patients.
Selection criteria for pulmonary metastasectomy were as follows: controlled primary CRC, absence of extrathoracic metastases with the exception of prior hepatic metastases radically resected, presence of unilateral or bilateral lung metastases suitable for curative resection, adequate lung function, and no contraindication due to comorbidity.
Preoperative staging consisted of clinical examination, blood chemistry, and computed tomography (CT) scan of the chest and abdomen. In the majority of the patients (96/125 = 76.8%) evaluated since 1997, contrast-enhanced helical chest CT (5-mm-slice thickness) was performed at our institution. In the last 24 patients (17.5%) in the series, integrated positron emission tomography and computed tomography was used to screen for additional metastatic foci. Further imaging studies were performed as clinically indicated. Colonscopy (not older than 6 months) was used to confirm local control of primary CRC. Fiberoptic bronchoscopy was performed in patients with pulmonary lesion(s) located in the central one third of lung field. Finally, pulmonary function tests, including spirometry, lung diffusion capacity for carbon monoxide and arterial blood gases, were carried out on all 137 patients.
Data collection
Data collection included background demographic information such as age and sex, details about the primary tumor (CRC) which included location and Duke's stage, disease-free interval (DFI) from colorectal resection to pulmonary metastasectomy, prethoracotomy carcinoembryonic antigen (CEA) level, details about the lung metastases which included distribution, number, maximum size, and intrathoracic lymph node involvement, details about the surgery which included the surgical approach, type of pulmonary resection, presence of residual tumor, postoperative morbidity and mortality, and re-do surgery for local recurrence. As a matter of fact, complete palpation of the lung was considered a prerequisite for potentially curative resection, so that an open approach was used in most of the patients. At operation, macroscopically suspicious pulmonary and mediastinal lymph nodes were resected. Liver metastases previously resected and other treatments given were also recorded. Postoperative mortality was defined as any death occurring within the first 30 days after operation or during the same hospitalization.
Study endpoint and follow-up
The endpoint of analysis was survival time which was estimated by the Kaplan–Meier method using the date of first pulmonary metastasectomy as the starting point and the date of death or last follow-up as the endpoint.
Follow-up was complete and continued until December 2008.
Data analysis
Data are reported as absolute number and percentage or as mean and standard deviation (SD), unless otherwise specified. Differences between patient groups were analyzed with the χ 2 test. The effects of potential prognostic indicators on survival time were evaluated with both univariate and multivariate analysis. In the univariate analysis, Kaplan–Meier curves were compared by means of the log-rank test. Those variables with a univariate significance of p less than 0.10 were included in the multivariate analysis. Cox proportional hazards regression analysis was performed to investigate which variables remained independently associated with survival. The final model included prognostic indicators that remained significant with a p value less than 0.05. Hazard ratios and 95% confidence intervals (CI) were calculated.
The analysis was performed by using the SPSS statistical software (SPSS version 17.0 for Windows, SPSS Inc., Chicago, IL).
Results
Patient's demographic and clinical data
Of the 137 patients, 82 (59.8%) were men and 55 (40.2%) were women with a mean age at the time of the first pulmonary metastasectomy of 63.8 years (range, 35 to 82 years). Thirty-five (25.5%) were 70-years old or older. Demographic and clinical characteristics of the study population are summarized in Table 1.
All patients underwent a radical resection of the primary tumor. The majority of tumors arose from the colon and advanced tumor stages predominated. In 12 (8.7%) patients, liver metastases were identified and radically resected at the time of the original colorectal surgery, whereas in seven (5.1%) patients, lung metastases were present at the time of diagnosis of the primary tumor. Following primary colon or rectum resection, 73 (53.3%) patients received adjuvant chemotherapy (n = 51) or radiochemotherapy (n = 22). Widely varied regimens were used according to the local preferred practice of the unit where the resection was performed.
The median DFI from colorectal resection to pulmonary resection was 35.6 months (range, 0.6 to 154.3 months). The percentages of patients with a DFI of less than 12, 12–24, 24–36 months, and more than 36 months were 16.1%, 14.6%, 20.4%, and 48.9%, respectively.
The prethoracotomy CEA level was documented in 113 (82.5%) patients and was found to be elevated (>5 ng/ml) in 27 (23.9%).
In all patients, histopathology of the excised metastasis matched the histologic diagnosis from the colorectal resection. On the basis of pathologic assessment, pulmonary metastases were unilateral in 120 (87.6%) patients (73 right and 47 left) and bilateral in 17. Eighty-two (59.9%) patients had a solitary lung metastasis whereas 55 (40.1%) patients had two or more lung metastases. Median diameter of the metastases was 20.0 mm (range, 2.5 to 70.0 mm). Pulmonary and/or mediastinal lymph node involvement was found in seven (11.7%) out of 60 patients with suspicious nodes at surgery.
Location, size, and number of pulmonary lesions dictated the surgical approach and the type of pulmonary resection. In most patients, an open procedure was performed. One hundred and seventeen (85.4%) patients underwent lateral muscle sparing thoracotomy while 17 (12.4%) patients with bilateral lung metastases underwent median sternotomy (n = 16) or staged bilateral thoracotomy (n = 1). Finally, three (2.2%) patients deemed to be marginal surgical candidates because of poor lung function reserve underwent video-assisted thoracoscopic wedge resection for single, peripheral lesions measuring 2 cm or less in maximum diameter. Whenever possible, wedge resection was the procedure of choice with a view to preserve the maximum amount of functioning lung tissue. At operation, suspicious mediastinal and pulmonary lymph nodes were excised in 60 (43.8%) patients. Complete resection of all known pulmonary disease was achieved in 134 (97.8%) patients while residual tumor was microscopically documented in the surgical margins in three patients. No postoperative deaths occurred within the first 30 days after surgery or during the same hospitalization. Major morbidity was observed in 18 (13.1%) patients including atrial fibrillation (n = 7), lung infection (n = 5), bleeding requiring transfusions (n = 2), prolonged air leak (n = 2), respiratory distress (n = 1), and wound infection (n = 1).
Ten (7.3%) patients received induction chemotherapy before resection of pulmonary metastases, while 25 (18.2%) patients received adjuvant treatment, mostly consisting of 5-fluorouracil-based chemotherapy, after lung metastasectomy.
A total of 158 pulmonary resections were performed on 137 patients during the study period. Some patients underwent two (n = 11) or three (n = 5) surgical procedures for recurrent lung metastases. The median time interval between first and second lung metastasectomy, and second and third lung metastasectomy was 52.4 months (range, 23.1 to 87.9 months) and 14.9 months (range, 0.8 to 22.9 months), respectively. At re-do surgery, 14 patients underwent wedge resection, six patients underwent lobectomy, and one patient underwent bilobectomy. Following 21 surgical procedures, seven (33.3%) major complications occurred which included atrial fibrillation (n = 3), prolonged air leak (n = 2), bleeding requiring transfusions (n = 1), and bleeding requiring re-operation (n = 1). Although major morbidity following repeat metastasectomy was significantly higher than major morbidity following first metastasectomy (χ 2 test p = 0.018), no postoperative deaths were observed.
Finally, 43 (31.4%) patients had liver metastases radically resected before lung metastasectomy. The median time interval between primary CRC and liver resection was 12 months (range, 0 to 49 months). As stated above, in 12 patients liver metastatic involvement was found at the time of primary tumor diagnosis.
Survival data
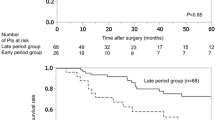
At the conclusion of this study in December 2008, with a median follow-up period of 36.2 months (range, 4.6 to 126 months), 58 patients (42.3%) had died (median survival, 28.8 months; range, 6–99.3 months). Deaths resulted from recurrent CRC in 49 patients, unrelated causes in three, and unknown causes in six. Median follow-up of 79 surviving patients (57.7%) was 41.3 months (range, 4.6 to 126 months). Twenty-four (30.4%) of the 79 surviving patients faced tumor recurrence. Overall 5-year and 10-year survival rates after initial pulmonary metastasectomy were 55.4% and 30.8%, respectively (Fig. 1).
Univariate analysis
Prognostic indicators that were determined as significant at univariate analysis included number of pulmonary metastases (p = 0.002), disease-free interval (p = 0.013), and presence of microscopic residual tumor after pulmonary resection (p = 0.024; Table 2).
Factors that marginally predicted worse prognosis were presence of bilateral lung metastases (p = 0.074), undergoing adjuvant chemotherapy after pulmonary metastasectomy (p = 0.086), age younger than 50 years (p = 0.087), elevated CEA level exceeding 10 ng/ml (p = 0.092), and surgical approach (median sternotomy vs unilateral thoracotomy; p = 0.094).
The remaining parameters failed to be significant predictors of survival in the univariate analysis. Worthy of note is the fact that no difference of survival was found between patients undergoing sequential pulmonary metastasectomy after hepatic metastasectomy and patients undergoing simple pulmonary metastasectomy (p = 0.77). Nor was any difference of survival found between patients undergoing single pulmonary metastasectomy and patients undergoing re-do surgery for local recurrent disease (p = 0.79).
Multivariate analysis
At the multivariate analysis, disease-free interval and number of pulmonary metastases were the parameters that retained significant independent prognostic impact (Table 3). All the remaining variables did not enter the model.
Prognostic factors which were confirmed as significant at the multivariate analysis were used to divide patients into three groups: group 1—patients with single metastasis and DFI ≥24 months (n = 56); group 2—patients with multiple metastases or DFI <24 months (n = 65); group 3—patients with multiple metastases and DFI <24 months (n = 16). Highly significant differences in survival were identified (p = 0.00029). Five-year survival rate was 75.1% for group 1, 52.1% for group 2, and 11.6% for group 3.
Discussion
The first aim of this study was to investigate clinicopathologic characteristics of patients undergoing pulmonary metastasectomy for CRC. The majority were males in their sixties who had been treated with colonic resection for primary carcinoma in advanced pathologic stage. Unilateral, single metastatic foci predominated. Lateral muscle sparing thoracotomy and wedge resection were the surgical approach and procedure of choice, respectively. There was no postoperative mortality and major morbidity occurred in 18 (13.1%) patients. After first resection of pulmonary metastasis, overall median survival and 5-year survival rate was 36.2 months (95% CI 31.5–39.2) and 55.4%, respectively.
Pfannschmidt and coworkers [7], in a systematic review of published series reporting the results of surgical resection of pulmonary metastases from CRC, found that the most consistently identified independent prognostic indicators were prethoracotomy CEA level, number of pulmonary metastases, and intrathoracic lymph node involvement.
In general, patient demographics (i.e., age and sex) have not been shown to be independent prognostic factors for survival. In our experience, patients younger than 50 years tended to have shortened survival compared to older patients but the difference was not significant. However, according to Iizasa and coworkers [8], age greater than 60 years was an ominous prognostic factor for survival, while, according to Onaitis and coworkers [9], age younger than 65 years and female sex were significant predictors of recurrence.
Conflicting information exists regarding a number of potential prognostic indicators which are preoperatively evaluated in candidates for surgical resection of pulmonary metastases from CRC: location, histology and stage of primary CRC, CEA level, disease-free interval, previous extrathoracic disease, and previous pulmonary metastasectomy. In the present study as well as in copious literature [8], neither location nor pathologic stage of primary CRC had a significant impact on survival. However, Melloni and coworkers [10] as well as Inoue and coworkers [11] showed that primary tumor stage (T1/T2 vs T3/T4 and Duke's stage A vs B–D, respectively) was significantly associated with survival (hazard ratio, 2.947 and 0.326, respectively).
An elevated prethoracotomy CEA level has often been reported as an independent prognostic factor in patients undergoing surgery for lung metastasis from CRC [8, 9, 12, 13]. However, in our study, only when analyzing with a twofold cut-off value limit, patients with an elevated CEA level had a marginally worse survival than those with a low CEA level. Interestingly, by using CEA level as a continuous variable, a significant relationship between increasing CEA level and shorter survival was found at univariate analysis (p = 0.0035).
Our data show that a disease-free interval between primary CRC resection and pulmonary metastasectomy of less than 2 years was significantly and independently associated with poor survival. Additional series, published since Pfannschmidt and coworkers' systematic review [7], have confirmed the statistical significance of disease-free interval. Yedibela and coworkers [14], in a series of 141 patients with curative resection of pulmonary metastases from CRC, found a significant survival advantage (hazard ratio, 0.423) in patients who developed pulmonary metastases more than 3 years after treatment of their primary tumor. Onaitis and coworkers [9], in a series of 378 patients who underwent pulmonary resection for CRC metastases with curative intent, demonstrated that a disease-free interval of less than 1 year was an independent predictor of recurrence (hazard ratio, 1.6).
Finally, in agreement with previous reports [8, 11, 12, 15–17], no significant difference in survival was demonstrated between patients with and without history of previously resected hepatic (5-year survival rate, 53.2% and 56.5%, respectively) or pulmonary (5-year survival rate, 59.5% and 55.1%, respectively) metastases. According to several authors [18, 19], also selected patients with simultaneous presentation of technically resectable liver and lung metastases may benefit from an aggressive multidisciplinary surgical approach. Nevertheless, it is worthy of consideration that these favorable results might be due to selection mechanisms [5].
Following pulmonary metastasectomy for CRC, numerous operative and postoperative measurements are available which may have important prognostic implications for survival. Both the majority of previous series and our experience show that surgical approach, type of pulmonary resection as well as distribution (unilateral vs bilateral) of lung metastases do not influence prognosis. However, Saito and coworkers [16] found that the survival of patients who underwent simultaneous bilateral metastasectomy was significantly lower than that of patients undergoing unilateral or bilateral sequential metastasectomy while Inoue and coworkers [11] reported that unilateral location of pulmonary metastasis was an independent predictor of longer survival by multivariate analysis. Furthermore, although wedge resection is generally considered as the procedure of choice, Yedibela and coworkers [14] observed a significantly longer survival for patients undergoing an anatomical resection. Finally, three recent series questioned the traditional open approach to pulmonary metastasectomy in CRC. Nakaijma and coworkers [20] questioned the role of manual palpation in the detection of small pulmonary nodules; in their study of 102 patients, they found ipsilateral recurrent pulmonary metastases in 27 (34.2%) of 79 thoracoscopies and 27 (62.8%) of 43 open thoracotomies (p = 0.0023) within 2 years of surgery. Nakas and coworkers [21] in their study of 52 patients undergoing pulmonary metastasectomy for CRC (27 open and 25 video-assisted approach) reported no difference in the incidence of missed lesions, pulmonary disease progression, recurrence in the same lobe, and estimated actuarial survival. Similarly, Onaitis and coworkers [9] found no recurrence-free survival difference between the open and the thoracoscopic approach, after controlling for all other factors.
One of the main findings of the present study was that the number of pulmonary metastatic foci of CRC significantly and independently influenced long-term survival after surgery. Median survival and 5-year survival rate were 38.6 (95% CI 34.2–44.6) months and 69.7%, respectively, in patients with single metastasis, and 31.3 (95% CI 22.4–36.8) months and 35.5%, respectively, in patients with multiple metastases. Similar results were reported by several authors who used a variety of cut-off points to evaluate the prognostic significance of the number of pulmonary metastases [8, 9, 12–15, 22, 23].
On the other hand, in our experience, tumor size, intrathoracic lymph node involvement, and completeness of resection were not found to be independent prognostic factors. Interestingly, according to Iizasa and coworkers [8], maximum tumor size (≤3 cm vs >3 cm) was not determined as significant by univariate analysis. However, multivariate analysis demonstrated the prognostic significance of maximum tumor size represented as a continuous variable. As for intrathoracic lymph node involvement and completeness of resection, pulmonary and mediastinal lymph nodes were examined in 60 (43.8%) out of 137 patients, while residual tumor was microscopically documented in the surgical margins in three (2.2%) patients only. Most likely, the small sample size of these patient groups prevented lymph node involvement and completeness of resection from emerging as being significant prognostic factors.
This study has several limitations. First, the single-center retrospective design and the highly selected patient population could have introduced biased information. Second, further bias could have been introduced by the selection of “data-derived” cut-off points when evaluating the prognostic importance of continuous variables, such as disease-free interval and number of pulmonary metastases. Finally, the role of multimodality therapy, including induction and/or adjuvant chemotherapy, is not discernible in our series.
In conclusion, although surgery for pulmonary metastases from CRC is a controversial area in which there is insufficient evidence to inform definitive management decisions, it is possible to make a few non-controversial statements.
Patients with metastatic lung involvement from CRC face a poor prognosis, despite modern chemotherapy regimens. A minority of these patients may be offered surgery with a potential survival advantage. Ideal candidates to surgery are the patients with a solitary metastasis and metachronous disease with a long disease-free interval. Patients undergoing surgery are exposed to iatrogenic complications. However, chances of long-term survival are better for resection of a solitary lung metastasis from CRC than for resection of a primary bronchogenic carcinoma [24].
Further work, hopefully in the form of a randomized controlled trial comparing pulmonary metastasectomy in CRC to other treatment regimens [25], is needed to definitely establish the effectiveness of surgery in this disease.
References
Ferlay J, Autier P, Boniol M, Heanue M, Colombet M, Boyle P (2007) Estimates of the cancer incidence and mortality in Europe in 2006. Ann Oncol 18:581–592. doi:10.1093/annonc/mdl498
Verdecchia A, Francisci S, Brenner H, Gatta G, Micheli A, Mangone L, EUROCARE-4 Working Group (2007) Recent cancer survival in Europe: a 2000-02 period analysis of EUROCARE-4 data. Lancet Oncol 8:784–796. doi:10.1016/S1470-2045(07)70246-2
Renehan AG, Egger M, Saunders MP, O'Dweyr ST (2002) Impact on survival of intensive follow up after curative resection for colorectal cancer: systematic review and meta-analysis of ramdomized trials. BMJ 324:813. doi:10.1136/bmj.324.7341.813
Manfredi S, Bouvier AM, Lepage C, Hatem C, Dancourt V, Faivre J (2006) Incidence and patterns of recurrence after resection for cure of colonic cancer in a well defined population. Brit J Surg 93:1115–1122. doi:10.1002/bjs.5349
Aberg T (1997) Selection mechanisms as major determinants of survival after pulmonary metastasectomy. Ann Thorac Surg 63:611–612. doi:10.1016/S0003-4975(97)00006-4
Treasure T (2008) Pulmonary metastasectomy for colorectal cancer: weak evidence and no randomized trial. Eur J Cardiothorac Surg 33:300–302. doi:10.1016/j.ejcts.2007.10.015
Pfannschmidt J, Dienemann H, Hoffmann H (2007) Surgical resection of pulmonary metastases from colorectal cancer: a systematic review of published series. Ann Thorac Surg 84:324–338. doi:10.1016/j.athoracsur.2007.02.093
Iizasa T, Suzuki M, Yoshida S, Motahashi S, Yasufuku K, Iyoda A, Shibuya K, Hiroshima K, Nakatani Y, Fujisawa T (2006) Prediction of prognosis and surgical indications for pulmonary metastasectomy from colorectal cancer. Ann Thorac Surg 82:254–260. doi:10.1016/j.athoracsur.2006.02.027
Onaitis MW, Petersen RP, Haney JC, Saltz L, Park B, Flores R, Rizk N, Bains MS, Dycoco J, D'Amico TA, Harpole DH, Kemeny N, Rusch VW, Downey R (2009) Prognostic factors for recurrence after pulmonary resection of colorectal cancer metastases. Ann Thorac Surg 87:1684–1689. doi:10.1016/j.athoracsur.2009.03.034
Melloni G, Doglioni C, Bandiera A, Carretta A, Ciriaco P, Arrigoni G, Zannini P (2006) Prognostic factors and analysis of microsatellite instability in resected pulmonary metastases from colorectal carcinoma. Ann Thorac Surg 81:2008–2013. doi:10.1016/j.athoracsur.2006.01.007
Inoue M, Ohta M, Iuchi K, Matsumura A, Ideguchi K, Yasumitsu T, Nakagawa K, Fukuhara K, Maeda H, Takeda S, Minami M, Ohno Y, Matsuda H (2004) Benefits of surgery for patients with pulmonary metastases from colorectal carcinoma. Ann Thorac Surg 78:238–244. doi:10.1016/j.athoracsur.2004.02.017
Pfannschmidt J, Muley T, Hoffmann H, Dienemann H (2003) Prognostic factors and survival after complete resection of pulmonary metastases from colorectal carcinoma: experiences in 167 patients. J Thorac Cardiovasc Surg 126:732–739. doi:10.1016/S0022-5223(03)00587-7
Kanemitsu Y, Kato T, Hirai T, Yasui K (2004) Preoperative probability model for predicting overall survival after resection of pulmonary metastases from colorectal cancer. Brit J Surg 91:112–120. doi:10.1002/bjs.4370
Yedibela S, Klein P, Feuchter K, Hoffmann M, Meyer T, Papadopoulos T, Göhl J, Hohenberger W (2006) Surgical management of pulmonary metastases from colorectal cancer in 153 patients. Ann Surg Oncol 13:1538–1544. doi:10.1245/s10434-006-9100-2
Zink S, Kayser G, Gabius H-J, Kayser K (2001) Survival, disease-free interval, and associated tumor features in patients with colon/rectal carcinomas and their resected intra-pulmonary metastases. Eur J Cardiothorac Surg 19:908–913. doi:10.1016/S1010-7940(01)00724-2
Saito Y, Omiya H, Kohno K, Kobayashi T, Itoi K, Teramachi M, Sasaki M, Suzuki H, Takao H, Nakade M (2002) Pulmonary metastasectomy for 165 patients with colorectal carcinoma: a prognostic assessment. J Thorac Cardiovasc Surg 124:1007–1013. doi:10.1067/mtc.2002.125165
Welter S, Jacobs J, Krbek T, Krebs B, Stamatis G (2007) Long-term survival after repeated resection of pulmonary metastases from colorectal cancer. Ann Thorac Surg 84:203–210. doi:10.1016/j.athoracsur.2007.03.028
Shah SA, Haddad R, Al-Sukhni W, Kim RD, Greig PD, Grant DR, Taylor BR, Langer B, Gallinger S, Wei AC (2006) Surgical resection of hepatic and pulmonary metastases from colorectal carcinoma. J Am Coll Surg 202:468–475. doi:10.1016/j.jamcollsurg.2005.11.008
Barlow AD, Nakas A, Pattenden C, Martin-Ucar AE, Dennison AR, Berry DP, Lloyd DM, Robertson GS, Waller DA (2009) Surgical treatment of combined hepatic and pulmonary colorectal cancer metastases. Eur J Surg Oncol 35:307–312. doi:10.1016/j.ejso.2008.06.012
Nakajima J, Murakawa T, Fukami T, Sano A, Sugiura M, Takamoto S (2007) Is finger palpation at operation indispensable for pulmonary metastasectomy in colorectal cancer? Ann Thorac Surg 84:1680–1684. doi:10.1016/j.athoracsur.2007.06.005
Nakas A, Klimatsidas MN, Entwisle J, Martin-Ucar AE, Waller DA (2009) Video-assisted versus open pulmonary metastasectomy: the surgeon's finger or the radiologist's eye? Eur J Cardiothorac Surg 36:469–474. doi:10.1016/j.ejcts.2009.03.050
Welter S, Jacobs J, Krbek T, Poettgen C, Stamatis G (2007) Prognostic impact of lymph node involvement in pulmonary metastases from colorectal cancer. Eur J Cardiothorac Surg 31:167–172. doi:10.1016/j.ejcts.2006.11.004
Rama N, Monteiro A, Bernardo JE, Eugénio L, Antunes MJ (2009) Lung metastases from colorectal cancer: surgical resection and prognostic factors. Eur J Cardiothorac Surg 35:444–449. doi:10.1016/j.ejcts.2008.10.047
Corman ML (2005) Carcinoma of the colon. In: Corman ML (ed) Colon and rectal surgery, 5th edn. Lippincott Williams & Wilkins, Philadelphia, p 871
Treasure T, Fallowfield L, Farewell V, Ferry D, Lees B, Leonard P, Macbeth F, Utley M (2009) Pulmonary metastasectomy in colorectal cancer: time for a trial. Eur J Surg Oncol 35:686–689. doi:10.1016/j.ejso.2008.12.005
Acknowledgements
We would like to thank Valentina Fava, (MSc) and Stefano Panetta, (MSc) for providing invaluable assistance in the statistical data analysis.
Conflict of Interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Borasio, P., Gisabella, M., Billé, A. et al. Role of surgical resection in colorectal lung metastases: analysis of 137 patients. Int J Colorectal Dis 26, 183–190 (2011). https://doi.org/10.1007/s00384-010-1075-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-010-1075-6