Abstract
Background
The role of preoperative neoadjuvant chemotherapy (NAC) in patients with resectable colorectal liver metastases (CRLM) remains undetermined. This study aimed to assess the efficacy of NAC in patients with resectable CRLM, especially in high-risk subgroups for recurrence, with special reference to synchronicity and the CRLM grade in the Japanese classification system.
Methods
A retrospective analysis of a multi-institutional cohort who was diagnosed with resectable CRLM was performed. CRLM was classified into three grades (A, B, and C) according to the combination of H stage (H1: ≤ 4 lesions and ≤ 5 cm, H2: ≥ 5 lesions or > 5 cm, H3: ≥ 5 lesions and > 5 cm), nodal status of the primary tumor (pN0/1: ≤ 3 metastases, pN2: ≥ 4 metastases), and the presence of resectable extrahepatic metastases.
Results
Among 222 patients with resectable CRLM, 97 (43.7%) had synchronous CRLM. The surgical failure-free survival (SF-FS) of patients with synchronous CRLM (without NAC) was significantly worse than that of patients with metachronous CRLM (P = 0.0264). The SF-FS of patients with Grade B/C was also significantly worse than that of Grade A (P = 0.0058). Among the 53 patients with synchronous and Grade B/C CRLM, 31 were assigned to NAC, and all of them underwent liver surgery. In this high-risk subgroup, the SF-FS and OS in the NAC group were significantly better than those in the upfront surgery group (P < 0.0001 and P = 0.0004, respectively).
Conclusions
Patients with synchronous and Grade B/C CRLM could be good candidates for indication of NAC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical resection of liver metastases is the only chance for cure in patients with colorectal liver metastases (CRLM), with reported 5-year survival of 28–51% [1,2,3,4]. Recent advancements in chemotherapy, including the molecular targeted agents, enabled previously unresectable patients to undergo resection, and consequently, the outcome of these patients has improved [5,6,7,8]. However, whether preoperative neoadjuvant chemotherapy (NAC) is beneficial for resectable CRLM patients remains controversial [9,10,11,12]. Nordlinger et al. reported a randomized controlled trial (EORTC 40,983) showing that perioperative chemotherapy with FOLFOX4 increased the progression-free survival compared with surgery alone in patients with resectable CRLM [13]. However, subsequent long-term analysis could not demonstrate the superiority of perioperative chemotherapy in terms of overall survival (OS) [14]. Although the final results were somewhat disappointing, several issues were raised regarding the baseline setting of the trial; that is, patients who had five or more metastatic tumors were excluded, and more than half of the patients had a single tumor. Thus, the participating patient group was considered to be at relatively low-risk for recurrence. Meanwhile, several recent studies revealed that only patients with high-risk profile for recurrence could receive survival benefit from NAC in patients with resectable CRLM [11, 15].
In 2008, Yamaguchi et al. [16] reported four independent prognostic factors of CRLM in a retrospective, multicenter study: five or more hepatic nodules, size larger than 5 cm, nodal status (N2) of primary colorectal tumor, and presence of extrahepatic metastases (EM). Based on these prognostic factors, CRLM was classified into Grade A, B, and C. Since this classification system involves not only hepatic tumor information but also nodal status, which reflects the malignant potential of the primary tumor, it is known to well stratify the prognosis of patients with CRLM, and is currently endorsed by the Japanese Society for Cancer of the Colon and Rectum [17].
Based on previous evidences, we thought that stratification of the risk profile was crucial to maximize the benefits of NAC in patients with resectable CRLM. This study aimed to define the high-risk subset in patients with resectable CRLM, with special reference to the CRLM grade by the Japanese classification system, and to assess the efficacy of NAC in its subset in the era of modern chemotherapy.
Patients and methods
Patients
Between January 2013 and December 2019, 310 patients were diagnosed with colorectal liver metastases (CRLM) at Fukuoka City Hospital (Fukuoka, Japan), Saiseikai Fukuoka General Hospital (Fukuoka, Japan), and Matsuyama Red Cross Hospital (Matsuyama, Japan). Among them, 222 patients were diagnosed with resectable CRLM and the other 88 were diagnosed with unresectable CRLM. Diagnosis of CRLM was established basically using contrast-enhanced computed tomography (CT) and Gd-EOB-DTPA-enhanced magnetic resonance imaging. Positron emission tomography CT was also used in most patients for detection of extrahepatic metastases. The Charlson comorbidity index was used to evaluate preoperative comorbidities [18]. Resectable CRLM was defined as follows: (1) tumors that could be technically resectable, leaving at least 30% of the residual liver volume regardless of tumor number and size; (2) primary tumor was curatively resectable or already resected; (3) no unresectable EM [19]; and (4) Eastern Cooperative Oncology Group performance status of the patient was 0/1, and the general condition of the patients was sufficient to receive liver surgery or, in some cases, pulmonary surgery. Synchronous CRLM was defined as CRLM that detected at the time of diagnosis of the primary tumor, and metachronous CRLM was as CRLM that detected later than that time.
The treatment strategy for resectable CRLM was principally determined based on the institution’s policy. In Saiseikai Fukuoka General Hospital, NAC for resectable CRLM was aggressively conducted when patients were considered to be at high risk of postoperative recurrences. In Matsuyama Red Cross Hospital, the principle policy for resectable CRLM was upfront surgery regardless of tumor condition until April 2017. After that time, NAC was introduced for high-risk resectable CRLM. In Fukuoka City Hospital, NAC for resectable CRLM was aggressively conducted until April 2016. After that time, policy was changed to upfront surgery according to personnel changes. In all institutes, principal strategy regarding the timing of hepatectomy was primary first, two-stage surgery, except for some limited cases. Parenchymal-sparing liver resections were performed in principal; in some cases, anatomical liver resection was performed when this procedure offered advantages in operative time, blood loss, safety, or invasiveness. NAC and palliative chemotherapy after unresectable relapse were conducted by experienced oncologists at each institution. In cases with pulmonary metastases, assessment of resectability and surgery, if needed, were performed by experienced thoracic surgeons. A written informed consent was obtained from all patients before the treatment. This study was conducted in compliance with the ethical principles of the Declaration of Helsinki, and the study protocol was approved by the institutional review board of each institution (approval number: 789, 2019-9-7 and 204).
Grading system of CRLM
In the Japanese classification system of colorectal carcinoma, CRLM was classified into three grades according to combination of H stage (H1: ≤ 4 lesions and maximum tumor size ≤ 5 cm, H2: ≥ 5 lesions or > 5 cm, H3: ≥ 5 lesions and > 5 cm), nodal status of primary tumor (pN0/1: ≤ 3 metastases, pN2: ≥ 4 metastases), and presence of EM. Briefly, Grade A was H1 and pN0/1; Grade B was H2 and pN0/1, or H1 and pN2; and Grade C was H2 and pN2, or H3 with any pN, or EM with any H/pN (Fig. 1). In this study, Grade C was limited to those without unresectable EM because resectable CRLM was defined as those without unresectable EM.
Grading of colorectal liver metastasis by the Japanese classification system. CRLM was classified into three grades according to combination of H stage, nodal status of primary tumor (pN0/1: ≤ 3 metastases, pN2: ≥ 4 metastases), and the presence of extrahepatic metastases (EM). H stage was defined by the number and maximum diameter of liver metastases: H1, ≤ 4 lesions and ≤ 5 cm; H2, ≥ 5 lesions or > 5 cm; H3, ≥ 5 lesions and > 5 cm. In this study, Grade C was limited to those without unresectable EM (shaded area), because resectable CRLM was defined as those without unresectable EM
Patient follow-up
After liver surgeries, patients were followed up every 3 months during the first 2 years and 6 months thereafter. Recurrent CRLM was treated in the same fashion as the initial treatment. OS was defined as the interval from the date of initial diagnosis of CRLM to the date of death by any cause. As a parameter to assess recurrence, the concept of time to surgical failure (TSF) was employed instead of recurrence-free survival (RFS). In CRLM patients with resectable recurrences, re-resection of recurrent tumors is known to provide survival benefits [20]. Thus, TSF is considered a better surrogate endpoint of OS than RFS [21]. In this study, the event-free survival of TSF was defined as surgical failure-free survival (SF-FS), which was the interval from the date of initial diagnosis of CRLM to the date of unresectable recurrence or death by any cause.
Statistical analysis
Nonparametric variables were expressed by median (range), and compared using the Mann–Whitney U tests. Categorical data were compared using the Chi-square test. OS and SF-FS were estimated using Kaplan–Meier method and compared using log-rank test. Deaths from all causes were included in the calculation of survival. Cox proportional hazard models were created to evaluate the risk associated with prognostic variables. Statistical analyses were performed using JMP Pro 14 software (SAS Institute, Cary, NC, USA). A value of P < 0.05 was considered significant.
Results
Analysis of the entire cohort
Table 1 shows the baseline characteristics of the 222 patients diagnosed with resectable CRLM. Among them, 97 patients (43.7%) had synchronous CRLM and the remaining 125 patients (56.3%) had metachronous CRLM. Characteristics representing tumor malignancy, such as tumor markers, maximum tumor diameter, and lymph node positivity of primary tumors in patients with synchronous CRLM were significantly worse than those in patients with metachronous CRLM. For the entire cohort, the median follow-up period for survivors was 36 months. Figure 2A shows the Kaplan–Meier curves of the SF-FS according to the synchronicity of CRLM. Although the SF-FS curve of patients with synchronous CRLM (n = 97) seemed worse than that of those with metachronous CRLM (n = 125), the difference was not statistically significant (P = 0.1223). To exclude the possibility that NAC had influenced the results, an analysis of patients without NAC was performed (Fig. 2B). The SF-FS of synchronous CRLM (n = 59) was significantly worse than those of metachronous CRLM (n = 110) (P = 0.0264). Figure 3A shows the Kaplan–Meier curves of the SF-FS according to the liver metastasis grade (A, B, or C), which revealed significant differences among the three grades (P = 0.0064). When SF-FS was compared between Grade A (n = 124) and Grade B/C (n = 98) (Fig. 3B), the SF-FS of Grade B/C CRLM was significantly worse than that of Grade A CRLM (P = 0.0058).
Analysis of the synchronous CRLM cohort
In the analysis of the patients with synchronous CRLM, the 1-/3-year SF-FS rates of the NAC (n = 38) and Upfront surgery (n = 59) groups were 86.8/52.5% and 56.9/43.1%, respectively (P = 0.0694). The cohort was further divided according to the liver metastasis grade to assess the efficacy of NAC in a more high-risk subgroup for recurrence. Defining the patients with synchronous, Grade B/C CRLM as the high-risk group, the efficacy of NAC was analyzed. Table 2 summarizes the baseline characteristics of the NAC (n = 31) and Upfront surgery (n = 22) groups among patients with synchronous, Grade B/C CRLM. There were no significant differences in the preoperative tumor characteristics representing malignancy, such as tumor markers, maximum tumor diameter, number of tumor nodules, and lymph node positivity of primary tumor. On the other hand, the rates of patients with resectable EM in the NAC group were significantly higher than those in the Upfront surgery group.
Among 31 patients who received NAC, 18 (58.1%) received FOLFOX-based regimens, and 26 (83.9%) received a combination with anti-EGFR or anti-VEGF antibodies. The median number of NAC cycles performed was 7. The carcinoembryonic antigen levels and the carbohydrate antigen 19-9 level significantly decreased after NAC (P < 0.0001 and P = 0.0017). The shrinkage rate of the maximum tumor diameter in the NAC group was 36.8%. None of the patients became unresectable due to progression after receiving NAC.
Table 3 shows the surgical outcomes of the two groups. There were no significant differences in the rates of major hepatectomy, operative time, blood loss, postoperative morbidity, and hospital stay. Adjuvant chemotherapy after liver surgery was performed in 67.7% of patients in the NAC group and 63.6% in the Upfront surgery group (P = 0.7558). Although it was not statistically significant, the rates of early recurrence (within 6 months) after liver resection were higher in the upfront surgery group than that in the NAC group (54.6% and 32.3%, P = 0.1047).
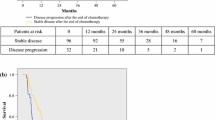
The Kaplan–Meier curves of the SF-FS and OS after initial diagnosis in synchronous, Grade B/C patients are shown in Fig. 4. The SF-FS in the NAC group (n = 31) was significantly better than that in the Upfront surgery group (n = 22) (the 1-/3-year SF-FS rates: 87.1/54.2% and 32.2/9.0%, P < 0.0001). Furthermore, significant survival benefit was also observed by NAC (the 1-/3-year OS rates: 100/75.0% in the NAC group and 90.5/31.0% in the Upfront surgery group, P = 0.0004).
Kaplan–Meier curves of the SF-FS and OS in patients with synchronous and Grade B/C resectable CRLM. A Comparison of the SF-FS between the NAC (n = 31) and Upfront surgery (n = 22) groups. B Comparison of the OS between the NAC (n = 31) and Upfront surgery (n = 22) groups. SF-FS, surgical failure-free survival; OS, overall survival; NAC, neoadjuvant chemotherapy
In the analysis of synchronous, Grade A patients (Supplementary Fig. 1A), there was no significant difference in SF-FS between the NAC (n = 7) and the Upfront surgery (n = 37) group (P = 0.9413).
Since Grade B CRLM can be divided into two subgroups (H2 and pN0/1, and H1 and pN2), analysis in these subgroups were also performed in resectable CRLM patients (Supplementary Fig. 2). In the synchronous cohort, the SF-FS in the H1 and pN2 group (n = 12) was significantly worse than that in the H2 and pN0/1 group (n = 15) (P = 0.0490). When synchronous Grade B subgroups were compared between NAC and upfront surgery group, both Grade B subgroups showed better SF-FS in the NAC group.
Prognostic factors after liver resection in synchronous CRLM patients
Table 4 shows the results of univariate and multivariate analyses of variables associated with SF-FS and OS in patients with synchronous CRLM. In the multivariate analysis, Grade B/C, without NAC, primary node positive, CA19-9 levels more than 50, and presence of EM were independent prognostic factors for SF-FS, while without NAC, CA19-9 levels more than 50, and presence of EM were for OS. NAC was identified as a common independent prognostic factor for both SF-FS and OS.
Analysis of the metachronous CRLM cohort
In the analysis of patients with metachronous CRLM, no significant differences were observed in SF-FS between the NAC and Upfront surgery group, even if the cohort was divided into Grade A (Supplementary Fig. 1B) and Grade B/C (Supplementary Fig. 1C).
Discussion
The current retrospective study demonstrated that patients with resectable, synchronous Grade B/C CRLM, namely, with high-risk profiles for recurrence showed significant improvement in SF-FS and OS by NAC. Meanwhile, such beneficial effect by NAC was not observed in patients who had relatively low-risk profiles such as synchronous Grade A, or metachronous CRLM.
Regarding the role of NAC in patients with resectable CRLM, several previous studies with various range of evidence levels have been reported to date, which must be interpreted with caution. In the EORTC 40,983 trial, the largest prospective randomized controlled trial that analyzed the role of NAC in patients with resectable CRLM, although the recurrence-free survival was improved, the survival benefit of NAC was not demonstrated [14]. However, approximately half of the study participants had a single or metachronous tumor. Thus, when the patient’s risk profile was not high enough, NAC could not offer survival benefit for those with resectable CRLM [22, 23] Another example is a retrospective case–control study from a single center, wherein patients with high-risk profiles tend to be allocated to the NAC group, with the consequence that different background characteristics due to selection bias led to the inappropriate results [12, 24]. In the current study, although it was retrospective, the study subjects were enrolled from three institutions with different treatment policies for resectable CRLM. Accordingly, patients with high-risk profiles were equally distributed into the NAC group and upfront surgery group.
Seeking the mechanism of beneficial effects of NAC, we have realized the shift of the event-free survival curves toward right side in the NAC group (Fig. 4). Namely, the beginning of the decrease in the survival curves in the NAC group was delayed approximately 1 year compared with that in the upfront group. In this patient group, the median number of NAC cycles was seven, which almost corresponds to a period of half a year. These findings suggest that, not only ameliorating event-free survivals, NAC might have canceled the early occurrence of surgical failure within about 6 months after liver surgery. In the high-risk patient group, the early recurrence after liver surgery was remarkable. Especially in the upfront group, it occurred in more than 50% of patients. The early recurrence after resection of CRLMs is thought to be attributable to micrometastases that cannot be detected before surgery [25]. The mechanism of beneficial effects of NAC might be, at least in part, a suppression of micrometastases.
In a recent retrospective study by Ichida et al. pursuing the optimal indication criteria for NAC in patients with resectable CRLM, they defined the patients having ≥ 4 metastases, ≥ 5 cm in maximum tumor diameter, or resectable EM as borderline resectable CRLM. They found that favorable survival outcomes were achieved by NAC in patients with borderline resectable CRLM. Their insistence that the beneficial effect of NAC can be maximized by defining the high-risk patient group is quite identical to that of our study. The difference is the range of defined criteria of high-risk patient groups that are supposed to benefit from NAC. Their definition of borderline resectable CRLM was almost identical to H2/3 in the Japanese classification plus resectable EM. Compared with our criteria, namely, Grade B/C CRLM without unresectable EM, the patients with H1 and primary N2 were categorized as high-risk group in our study, but not in the definition of borderline resectable CRLM. In the cohort of current study, 12 patients had H1 and primary N2 CRLM, and their 3-year SF-FS rate was 27.8%, which was sufficient to consider them as a high-risk patient group. Furthermore, when they were compared between the group with or without NAC, although the number of patients was quite small, the SF-FS of the patient who underwent NAC was significantly better than that without NAC (data not shown). Therefore, we believe that our definition of high-risk patients is better than their definition, borderline resectable CRLM.
In an analysis of metachronous CRLM patients, the beneficial effect of NAC was not observed even in patients with the Grade B/C subset. However, the proportion of patients who received NAC among the metachronous cohort was only 12%. Therefore, we cannot exclude the possibility of false negatives due to the small statistical power. Therefore, the effectiveness of NAC for patients with metachronous CRLM still needs to be verified in a future investigation. In previous reports, Beppu et al. developed a nomogram that predicts the disease-free survival of CRLM patients based on six prognostic factors [26]. Interestingly, the validation study of the nomogram revealed that, in patients with no risk factors, NAC provided significantly worse outcome than upfront surgery [27]. Although the reason of such an odd phenomenon is uncertain, it seems likely that the patients with low-risk for recurrence cannot receive survival benefit by NAC. CHARISMA is an ongoing randomized phase 3 clinical trial evaluating the efficacy of NAC in patients with resectable CRLM, especially with high clinical risk score [28]. The results of the trial will be of great interest because they hypothesized that, similarly to our results, NAC will provide a survival benefit in patients bearing a high-risk profile.
This study had several limitations. The study period was set after 2013, when the modern chemotherapy regimens had become fully available in our institutions. Therefore, the follow-up period of the patients was not sufficient enough to assess the long-term outcomes of CRLM patients. Therefore, the concept of TSF was employed as a surrogate endpoint for OS in this study. The first relapse event after initial liver resection for CRLM does not necessarily indicate treatment failure because repeat resection of recurrent tumors can have curative potential in some patients. Oba et al. revealed that the correlation between TSF and OS was stronger than that between RFS and OS, and recommended TSF, rather than RFS, as a surrogate endpoint for OS in a clinical study of CRLM [21]. Furthermore, in patients with synchronous CRLMs, relatively high proportion of patients experience an event of surgical failure within 1 year. Especially in patients with Grade B/C CRLMs in the current cohort, it was more than 40%. Therefore, we believe that analyzing the SF-FS of such patients with short observation period would be meaningful. Thus, taking a relatively short follow-up period into consideration, we employed TSF as a more reliable endpoint and found a significant difference in SF-FS in an analysis of high-risk patient group, although statistical difference was confirmed even in an analysis of OS. Another limitation is that our study was retrospective, and the number of study subjects became small when analysis was divided into subgroups. However, the background characteristics of the two groups were similar because the participating institutions had different policies for NAC. At least, we believe that the results of the current study are sufficient to become a clue to consider larger prospective study for validation.
The SF-FS and OS of patients with synchronous and Grade B/C resectable CRLM were significantly improved by NAC. On the other hand, such beneficial effects were not observed in the other patients with synchronous Grade A or metachronous CRLM. The high-risk subset discovered in the current study could be a good candidate for the indication of NAC in patients with resectable CRLM, although a randomized controlled trial is needed for verification.
References
Hallet J, Sa Cunha A, Adam R et al (2016) Factors influencing recurrence following initial hepatectomy for colorectal liver metastases. Br J Surg 103:1366–1376. https://doi.org/10.1002/bjs.10191
Primrose J, Falk S, Finch-Jones M et al (2014) Systemic chemotherapy with or without cetuximab in patients with resectable colorectal liver metastasis: the new EPOC randomised controlled trial. Lancet Oncol 15:601–611. https://doi.org/10.1016/S1470-2045(14)70105-6
Kopetz S, Chang GJ, Overman MJ et al (2009) Improved survival in metastatic colorectal cancer is associated with adoption of hepatic resection and improved chemotherapy. J Clin Oncol 27:3677–3683. https://doi.org/10.1200/JCO.2008.20.5278
Saiura A, Yamamoto J, Hasegawa K et al (2012) Liver resection for multiple colorectal liver metastases with surgery up-front approach: bi-institutional analysis of 736 consecutive cases. World J Surg 36:2171–2178. https://doi.org/10.1007/s00268-012-1616-y
Hebbar M, Pruvot FR, Romano O et al (2009) Integration of neoadjuvant and adjuvant chemotherapy in patients with resectable liver metastases from colorectal cancer. Cancer Treat Rev 35:668–675. https://doi.org/10.1016/j.ctrv.2009.08.005
Folprecht G, Gruenberger T, Bechstein WO et al (2010) Tumour response and secondary resectability of colorectal liver metastases following neoadjuvant chemotherapy with cetuximab: the CELIM randomised phase 2 trial. Lancet Oncol 11:38–47. https://doi.org/10.1016/S1470-2045(09)70330-4
Beppu T, Emi Y, Tokunaga S et al (2014) Liver resectability of advanced liver-limited colorectal liver metastases following mFOLFOX6 with bevacizumab (KSCC0802 study). Anticancer Res 34:6655–6662
Oki E, Emi Y, Yamanaka T et al (2019) Randomised phase II trial of mFOLFOX6 plus bevacizumab versus mFOLFOX6 plus cetuximab as first-line treatment for colorectal liver metastasis (ATOM trial). Br J Cancer 121:222–229. https://doi.org/10.1038/s41416-019-0518-2
Wang ZM, Chen YY, Chen FF et al (2015) Peri-operative chemotherapy for patients with resectable colorectal hepatic metastasis: a meta-analysis. Eur J Surg Oncol 41:1197–1203. https://doi.org/10.1016/j.ejso.2015.05.020
Bonney GK, Coldham C, Adam R et al (2015) Role of neoadjuvant chemotherapy in resectable synchronous colorectal liver metastasis; an international multi-center data analysis using LiverMetSurvey. J Surg Oncol 111:716–724. https://doi.org/10.1002/jso.23899
Zhu D, Zhong Y, Wei Y et al (2014) Effect of neoadjuvant chemotherapy in patients with resectable colorectal liver metastases. PLoS ONE 9:1–6. https://doi.org/10.1371/journal.pone.0086543
Hirokawa F, Asakuma M, Komeda K et al (2019) Is neoadjuvant chemotherapy appropriate for patients with resectable liver metastases from colorectal cancer? Surg Today 49:82–89. https://doi.org/10.1007/s00595-018-1716-x
Nordlinger B, Sorbye H, Glimelius B et al (2008) Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup trial 40983): a randomised controlled trial. Lancet 371:1007–1016. https://doi.org/10.1016/S0140-6736(08)60455-9
Nordlinger B, Sorbye H, Glimelius B et al (2013) Perioperative FOLFOX4 chemotherapy and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC 40983): long-term results of a randomised, controlled, phase 3 trial. Lancet Oncol 14:1208–1215. https://doi.org/10.1016/S1470-2045(13)70447-9
Ichida H, Mise Y, Ito H et al (2019) Optimal indication criteria for neoadjuvant chemotherapy in patients with resectable colorectal liver metastases. World J Surg Oncol 17:1–9. https://doi.org/10.1186/s12957-019-1641-5
Yamaguchi T, Mori T, Takahashi K et al (2008) A new classification system for liver metastases from colorectal cancer in Japanese multicenter analysis. Hepatogastroenterology 55:173–178
Shinto E, Takahashi K, Yamaguchi T et al (2015) Validation and modification of the Japanese Classification System for liver metastases from colorectal cancer: a multi-institutional study. Ann Surg Oncol 22:3888–3895. https://doi.org/10.1245/s10434-015-4470-y
Yamashita K, Watanabe M, Mine S et al (2018) The impact of the Charlson comorbidity index on the prognosis of esophageal cancer patients who underwent esophagectomy with curative intent. Surg Today 48:632–639. https://doi.org/10.1007/s00595-018-1630-2
Hwang M, Jayakrishnan TT, Green DE et al (2014) Systematic review of outcomes of patients undergoing resection for colorectal liver metastases in the setting of extra hepatic disease. Eur J Cancer 50:1747–1757. https://doi.org/10.1016/j.ejca.2014.03.277
Oba M, Hasegawa K, Shindoh J et al (2016) Survival benefit of repeat resection of successive recurrences after the initial hepatic resection for colorectal liver metastases. Surgery 159:632–640. https://doi.org/10.1016/j.surg.2015.09.003
Oba M, Hasegawa K, Matsuyama Y et al (2014) Discrepancy between recurrence-free survival and overall survival in patients with resectable colorectal liver metastases: a potential surrogate endpoint for time to surgical failure. Ann Surg Oncol 21:1817–1824. https://doi.org/10.1245/s10434-014-3504-1
Allard MA, Nishioka Y, Beghdadi N et al (2019) Multicentre study of perioperative versus adjuvant chemotherapy for resectable colorectal liver metastases. BJS open 3:678–686. https://doi.org/10.1002/bjs5.50174
Ratti F, Fuks D, Cipriani F et al (2019) Timing of perioperative chemotherapy does not influence long-term outcome of patients undergoing combined laparoscopic colorectal and liver resection in selected upfront resectable synchronous liver metastases. World J Surg 43:3110–3119. https://doi.org/10.1007/s00268-019-05142-4
Hewes JC, Dighe S, Morris RW et al (2007) Preoperative chemotherapy and the outcome of liver resection for colorectal metastases. World J Surg 31:353–364. https://doi.org/10.1007/s00268-006-0103-8
Nishioka Y, Shindoh J, Yoshioka R et al (2017) Clinical impact of preoperative chemotherapy on microscopic cancer spread surrounding colorectal liver metastases. Ann Surg Oncol 24:2326–2333. https://doi.org/10.1245/s10434-017-5845-z
Beppu T, Sakamoto Y, Hasegawa K et al (2012) A nomogram predicting disease-free survival in patients with colorectal liver metastases treated with hepatic resection: multicenter data collection as a project study for hepatic surgery of the Japanese Society of Hepato-Biliary-Pancreatic Surgery. J Hepatobiliary Pancreat Sci 19:72–84. https://doi.org/10.1007/s00534-011-0460-z
Okuno M, Hatano E, Seo S et al (2014) Indication for neoadjuvant chemotherapy in patients with colorectal liver metastases based on a nomogram that predicts disease-free survival. J Hepatobiliary Pancreat Sci 21:881–888. https://doi.org/10.1002/jhbp.149
Ayez N, van der Stok EP, de Wilt H et al (2015) Neo-adjuvant chemotherapy followed by surgery versus surgery alone in high-risk patients with resectable colorectal liver metastases: the CHARISMA randomized multicenter clinical trial. BMC Cancer 15:1–7. https://doi.org/10.1186/s12885-015-1199-8
Acknowledgements
We thank all the patients and the investigators involved in this study.
Funding
This study received no financial support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interests for this article.
Ethical approval
This study was approved by the Institutional Review Board in each institution (approval number: 789, 2019–9-7 and 204).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.

10147_2021_2024_MOESM1_ESM.jpg
Supplementary file1 Supplementary Figure 1. Kaplan-Meier curves of the SF-FS in patients with (A) synchronous Grade A CRLM, (B) metachronous Grade A CRLM, (C) metachronous Grade B/C CRLM. Comparison between the NAC and Upfront surgery groups. SF-FS, surgical failure-free survival; NAC, neoadjuvant chemotherapy (JPG 1200 KB)

10147_2021_2024_MOESM2_ESM.jpg
Supplementary file2 Supplementary Figure 2. Kaplan-Meier curves of the SF-FS in patients with Grade B subgroups. Comparison between H2 and pN0/1 subgroup and H1 and pN2 subgroup in synchronous (A) and metachronous (B) CRLM patients, and comparison between NAC and Upfront surgery group in H1 and pN2 subgroup (C) and H2 and pN0/1 subgroup (D). SF-FS, surgical failure-free survival; NAC, neoadjuvant chemotherapy. (JPG 941 KB)
About this article
Cite this article
Ninomiya, M., Emi, Y., Motomura, T. et al. Efficacy of neoadjuvant chemotherapy in patients with high-risk resectable colorectal liver metastases. Int J Clin Oncol 26, 2255–2264 (2021). https://doi.org/10.1007/s10147-021-02024-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-021-02024-5