Abstract
Aim
The impact of 3-dimensional vector manometry (VM) for characterization of the functional outcome of restorative proctocolectomy (RP) was studied in 61 patients at a median of 86 months after RP for ulcerative colitis.
Methods
A 14-day continence diary was utilized to quantify continence, urgency, and the frequency of defecation. The clinical outcome data were correlated to the physiology parameters of VM and volumetry.
Results
VM parameters at rest correlated with postoperative continence but not substantially with stool frequency and urgency. High radial asymmetry was significantly correlated with the degree of incontinence (r = 0.333, p = 0.013). Resting pressures demonstrated a better correlation with the degree of incontinence when documented for the high-pressure zone (HPZ; portion of the sphincter with at least 50% of the maximum pressure; r = 0.301, p = 0.025) and when performed in the continuous pull-through technique. Stool frequency and urgency were better characterized by volumetry parameters like threshold volumes and pouch compliance. The specificity and sensitivity of the vector volume at rest of the HPZ for the prediction of incontinence was 63.6% and 59.1%, respectively. The corresponding values were 67% and 68%, respectively, for radial asymmetry at rest. Stool frequency and urgency were better characterized by volumetry parameters like threshold volumes and pouch compliance.
Conclusion
A strong anal sphincter at rest and a consistent radial distribution of the sphincter pressure are the most reliable indicators of continence after RP obtained by VM, but their clinical usefulness is limited.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Restorative proctocolectomy is the surgical treatment of choice for most patients with ulcerative colitis because the large bowel as the source of the disease is completely removed and continence can be preserved [1–4]. However, in many cases the functional outcome is far from perfect. The frequency of defecation ranges between six and eight in 24 h, and more than one third of the patients complain of at least some kind of incontinence [1, 2, 4–6]. Additionally, the liquid and aggressive small-bowel stool may affect the perianal skin leading to painful skin lesions [2].
In spite of some physiology studies, the knowledge concerning the pathophysiological background of these adverse outcome criteria is still limited. One reason for this is the difficulty to quantify the functional outcome. The frequency of defecation is easy to determine but is probably not the most important criterion of overall functional success. Continence and urgency seem to be much better criteria, but in most studies only crudely defined categories are used for quantification [7, 8]. A quantitative analysis of the relation between the clinical criteria of functional outcome and physiological parameters is difficult under these conditions.
In the present study, 3-dimensional vector manometry (VM) and pouch volumetry were used to obtain data on pouch-anal physiology. Three-dimensional VM gives a more detailed impression on both radial and longitudinal pressure distribution over the entire length of sphincter as conventional manometry does. Especially radial asymmetry, the degree of radial pressure inconsistency, has repeatedly been demonstrated as a manometric criterion of localized anal sphincter injuries [9–11]. In this study, we focused on the question whether 3-dimensional vector-manometry may substantially contribute to characterization and understanding of the physiology after restorative proctocolectomy. Therefore, these parameters were related to functional outcome parameters as continence, urgency, and frequency of defecation which were quantitatively documented in a diary.
Materials and methods
Patients treated with restorative proctocolectomy with a hand-sewn anastomosis for ulcerative colitis or indeterminate colitis between January 1990 and December 2002 at our institution were identified by a chart review and were invited for an interview and a follow-up investigation between January 2003 and August 2004.
Surgical technique
All restorative proctocolectomies were done personally by the first (ADR) or the senior author (KHV). The ileum pouch was designed as a 15–20 cm J-shaped reservoir using linear staplers (two 90-mm cartridges and optionally an additional 50-mm cartridge) inserted from the oral side, leaving behind a small bridge of not dissected bowel wall close to the apex. Mucosectomy was performed transanally in all cases. A 2–3 cm muscular cuff was preserved. The ileopouch-anal anastomosis was performed by placing four to eight anchoring sutures (polyglactin, Vicryl® 3–0, Ethicon, Norderstedt) to the muscular cuff to fix the pouch wall approximately 2 cm above the apex. Then, the apex was incised, and the actual ileopouch-anal anastomosis (IPAA) was fashioned with 12–18 polyglactin 3-0 stitches (Vicryl® 3-0, Ethicon, Norderstedt) suturing the whole bowel wall to the anoderm. The pouch was drained using a 24 Ch urinary catheter inserted through the anus for 5–7 days.
A protective ileostomy was performed in most cases. Ileostomy closure was intended 12 weeks after initial surgery or later, on patient’s demand or in case of adverse events demanding a prolongation of stoma protection, respectively.
Anorectal physiology testing
Anal vector manometry was performed using perfused catheters with eight radially oriented channels (Zinetics Medical). The catheters were connected to a pneumohydraulic capillary perfusion system and perfused with 0.5 ml H2O per minute per channel. The perfusion ports were located 5 cm from the catheter tip radially at 45° intervals. Each lumen was separately connected to an external pressure transducer. Data were transmitted to a PC, and the Polygram software (Medtronic) was used to calculate the variables of interest.
All manometry parameters were recorded with both the continuous and the station pull-through technique. The examination was performed with the patient in the left lateral position. In a first step, the catheter was inserted 6 cm and moved back with 0.5 cm/s using a catheter puller (CAMT, Germany). The procedure was repeated at least six times. The first three measurements were always disposed in order to reduce the effect of involuntary squeezing which we found to be most significant at the beginning of the procedure. After at least three pulls resulting in a repeated smooth curve without squeeze artefact, patients were asked to squeeze during pulling back the catheter. This procedure was repeated at least three times or more often if necessary to obtain at least three reproducible pressure profiles. The valid pulls were integrated by the computer to one rest and one squeeze profile. Then the catheter was inserted 6 cm, and patients were asked to squeeze for 10 s. Squeeze pressures were recorded as modal values over a period of 10 s. Patients than were asked to relax, and after the pressures had stabilized, resting pressures were also recorded as modal values over a period of 10 s. This procedure was repeated at 5, 4, 3, 2, and 1 cm.
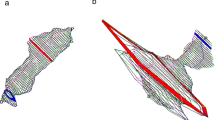
Three-dimensional manometric images of the anal sphincter were generated by the computer program Polygram for Windows (Medtronic), according to Perry et al. with some minor modifications [12]. All parameters were determined with both the station pull-through and the continuous pull-through methods. The functional length of the entire anal sphincter (EAS) was defined as the section of the sphincter in which 15% or more of the maximum pressure measured over the entire sphincter was reached in at least four of eight channels. The length of the high-pressure zone (HPZ) was defined as that section of the vectogram in which 50% or more of the maximum pressure was reached in at least four of eight channels (see Fig. 1). The mean anal rest and squeeze pressures were documented in the segment of highest mean anal pressure (SHMAP). Asymmetry is defined as the degree to which the pressure cross-section deviates from a perfect circle [13]. Segmental radial asymmetry (SRA) was documented in the SHMAP.
a and b Three-dimensional vectorgram of the anal sphincter. Entire sphincter length was defined as the portion of the sphincter in which the mean of the eight radial pressures exceeded 15% of the maximum pressure. Accordingly, the HPZ was defined as the portion of the sphincter in which this mean exceeded 50% of the maximum pressure. The segment of highest mean anal pressure was utilized for segmental analysis of mean pressure and radial asymmetry
According to Damon et al., we calculated asymmetry by adding up the pressures of the eight channels, dividing the number by the maximum pressure multiplied by the number of channels (n = 8) and subtracting the value from 1 [11]. This value was multiplied with 100 in order to give a percentage of asymmetry, with 0% indicating perfect symmetry and 100% worst asymmetry. The mean SRA of all segments of the EAS or HPZ was documented as the radial asymmetry index (RAI) of the EAS or the HPZ. In the 3-dimensional analysis, pressure was documented as both the average mean segmental pressures of all segments included in the EAS or HPZ, respectively, and the vector volume defined as sum of all segmental pressure volumes. Segmental pressure volumes were calculated as the pressure area of a specific segment times the length of this segment. Thus, the vector volume presents the product of sphincter length and pressure area.
The neorectal capacity was evaluated by a stepwise injection of air into a condom-like balloon fixed to a polyvinyl catheter. Fifty milliliters of air was injected over a period of 5 s. After the pressure in the balloon had been stabilized, this procedure was repeated until the maximum tolerated volume was reached. The volumes and pressures of first sensation of filling (V1, P1), first sensation of urge to defecate (V2, P2), and the maximum tolerated volume with its corresponding pressures (V3, P3) were recorded. The neorectal compliance C was calculated as the ratio of volume and pressure according to Jorge and Wexner [14] using the following equation:
Clinical evaluation of functional outcome
For quantification of the functional outcome, patients were asked to document all events of incontinence over a period of 14 days in a diary. We used a German translation of a diary, which has been used for the validation of incontinence scores [15]. Briefly, patients were asked for a daily quantitative documentation of
-
nature and amount of incontinence
-
sensation of urgency and both occurrence and amount of incontinence in consequence of urgency
-
necessity of using plugs and pads
-
use of loperamide, codeine, or other medication specifically directed against incontinence
-
interference with daily activity
According to Vaizey’s original presentation, each item was allocated with a numerical value ranging from 0.5 to 2. The daily maximum score was 10. As the diary was used over a period of 14 days, a maximum of 140 points could be reached [15].
For the purpose of this study, we used the first set of questions to quantify incontinence as the frequency and quantity of involuntary loss of stool or flatus. A maximum of 56 points (worst incontinence) could be reached over the period of 14 days. Urgency was defined as the sensation of urge with the consequence of involuntary loss of stool before reaching the toilet. It was quantified by the frequency of such episodes over the period of 14 days. Finally, the frequency of defecation over 24 h was documented.
In addition to the diary, global continence function was determined with the incontinence score of Vaizey and coworkers [15].
Statistical analysis
All physiology parameters were set in relation to the three clinical outcome criteria incontinence, urgency, and frequency of defecation.
In a first step, all patients were stratified into subgroups according to incontinence (0 vs. >0 incontinence points in diary), urgency (0 vs. >0 urgency points in diary), or frequency of defecation (≤6 or >6 per 24 h) and examined for significant differences in their physiology variables by the non-parametric Mann and Whitney U test. Subsequently the relation of the physiology parameters to the clinical outcome parameters was investigated by calculating Pearson correlation coefficients. For all analyses, a p value <0.05 was considered statistically significant.
For those vector-manometry variables which showed both a significant stratification between patients with or without the above-mentioned criteria of functional disorders and a significant correlation of the variable with the degree of this disorder, specificity and sensitivity of the variable were determined. Sensitivity was calculated as percentage of patients who were identified to have the criterion by the test variable among those patients with the clinical diagnosis of this criterion. Similarly specificity was calculated as percentage of patients suffering on one criterion of functional disorder by the test variable among those patients who really met this criterion. These calculations were performed with different cut-off points, and the results with the highest clinical relevance are reported.
Results
Restorative proctocolectomy with hand-sewn IPAA was performed in a consecutive series of 142 patients (80 men) with chronic inflammatory bowel diseases between January 1990 and December 2002 at our institution. One hundred thirty-four patients had the diagnosis of ulcerative colitis. Eight patients with the likely diagnosis of ulcerative colitis also had some evidence of Crohn’s disease and were classified as indeterminate colitis.
Ninety-eight patients (57 men) had a personal (n = 78) or a telephone (n = 20) interview. The incontinence diary was completed by 92 patients (53 men) at a median of 80.8 (14–143) months after the pouch operation. Sixty-four of these patients (41 men) also had a physiology examination with 61 patients having the investigation completed according to the protocol. Only these patients were taken into consideration for the further analysis. These patients had been 33.6 (14–60) years old at the time of surgery and 41.5 (23–68) years at the time of follow-up. Median follow-up time was 86 (26–129) months. The duration of the disease at the time of surgery had been 100 (13–325) months.
Functional outcome
The median global Vaizey’s incontinence score of the study group was 3 (0–17). The results of the incontinence diary for the group of 61 patients with clinical evaluation are summarized in Table 1. The median score from the diary was 9 (0–101). There were 17 (27.9%) with a score of zero, indicating a perfect functional outcome. Twenty-nine patients (47.5%) never experienced any involuntary loss of stool or gas, whereas 32 (52.5%) had at least one minor event over the 14-day period. In most cases, this was rather rare and of little quantity. The median frequency of defecation over 24 h was 7 (3–19). Of the 61 patients, 29 (47.5%) had a frequency of six or less, and 32 (52.5%) had more than six bowel movements over 24 h. Fourteen patients (23%) experienced some urgency, with 13 (21%) actually loosing stool in relation to the urge sensation. However, 45 patients (74%) documented that loss of stool or the fear of stool loss did not affect their daily life.
Relation of physiology parameters to clinical outcome
Continuous and station pull-through vector manometry was performed at rest and at squeeze. The results were evaluated concerning the relationship to the clinical criteria incontinence, urgency, and frequency of defecation. The data obtained from manometry at rest was significantly related to incontinence but not to urgency and frequency of defecation (Table 2). Overall, parameters determined with the continuous pull-through method were slightly better correlated to the functional outcome. Low resting pressures characterize incontinence, as mean pressures were repeatedly found to be inversely correlated with the severity of incontinence basically independent of the question whether the pressure was measured with the continuous or station pull-through technique or whether it was determined as the mean over the EAS length, the length of the HPZ, or only in the segment of the highest mean pressure. Functional length of the anal sphincter did not turn out to be related to any of the investigated outcome parameters.
Accordingly, the vector volume which presents the product of pressure and sphincter length was found to correlate with the degree of incontinence but not better than the mean pressure values alone.
Radial asymmetry was found to stratify significantly between patients with incontinence and those without (p = 0.003) and showed a reasonable correlation with the degree of incontinence (r = 0.333, p = 0.013) but only when determined with the continuous pull-through technique in the HPZ. However, sphincter asymmetry determined over both the entire sphincter length and in the best segment failed to show a relation with the functional outcome parameters as did asymmetry when determined in the station pull-through technique.
The squeeze pressure parameters did not show a strong relationship to the clinical outcome criteria (data not shown). Concerning incontinence, the only significant correlation was found between the degree of incontinence and the overall sphincter length (r = 0.277, p = 0.028). A mild correlation existed between the frequency of defecation and the RAI (r = -0.261, p = 0.044); however, clinical relevance seemed to be low because the medians were similar, and RAI failed to discriminate between patients with high and low stool frequency. One interesting finding was that patients with urgency seem to have better voluntary squeeze function than those patients without. Both vector volumes and squeeze pressures in the high-pressure zone were lower in the patients not suffering from urgency [102 (5.2–441) mmHg2·cm vs. 123 (18–746) mmHg2·cm, and 104 (33–213) mmHg vs. 140 (78–299) mmHg, respectively), but they were not correlated with the degree of urgency.
Among all vector-manometry parameters, only the vector volume and the radial asymmetry of the high-pressure zone at rest measured with the continuous pull-through method turned out to stratify significantly between patients with incontinence and those without and to correlate significantly with the degree of incontinence. If a cut-off level of 13.726 mmHg2·cm was used, a low vector volume was found to predict incontinence with a specificity of 63.6% and a sensitivity of 59.1%. For radial asymmetry, the specificity and sensitivity were 67% and 68%, respectively, when determined with a cut-off level of 22.4%.
Compared with vector manometry, volumetry resulted in more impressive correlations to other clinical criteria of functional outcome (Table 3). The frequency of defecation is characterized by the maximum tolerated volume, and the pouch compliance also demonstrates a good correlation to the stool frequency. Notably, the volume necessary to elect first sensation was significantly lower in patients suffering from urgency, as the compliance was. Although patients with incontinence had an approximately 30% lower maximum tolerated volume, no significant correlation of the maximum tolerated volume and the severity of incontinence was found.
Discussion
Restorative proctocolectomy is the surgical intervention of choice for the treatment of patients with ulcerative colitis and familial adenomatous polyposis coli [3]. However, postoperatively a significant number of patients suffer from some functional deficits. The frequency of defecation ranges from six to eight over 24 h; perfect continence, if defined as the complete absence of any involuntary loss of intestinal content at day and night, is only achieved in about one third of the patients as shown in studies with long-term follow-up [2, 4, 6], and only a minority of the patients never have problems with discrimination between stool and gas [1].
So far, our functional outcome data are in accordance with the literature. The median frequency of defection over 24 h matches well with the above-mentioned trials. The proportion of only 28% of the patients with a perfect continent diary and a proportion of approximately 50% of patients actually documenting involuntary stool loss appears quite unfavorable. However, the median incontinence score of our patients was 3. Hueting and co-workers, who used the same incontinence score in a group of patients with IPAA, reported a median of 7, which is significantly inferior to our data [16]. Another aspect is the wide variety of functional outcomes, indicated by a range of incontinence diary points between 0 and 101 of 140 possible points and a range of 0–17 of 24 possible points in Vaizey’s incontinence score.
Various factors contribute to functional outcome after IPAA. Lewis and co-workers studying 100 patients with double-stapling IPAA found four variables to be associated with a good functional outcome, namely, a low anal electrosensitivity threshold in the upper and middle anal canal, the presence of a pouch-anal inhibitory reflex, a good compliance of the reservoir, and a good anal resting pressure [7]. We did not make use of electrophysiology examinations, but the significance of the neuronal control was also supported by studies performed by Tomita and co-workers, who found anal canal electrosensitivity and a prolongation in pudendal nerve terminal motor latency as a factor associated with soiling [17, 18].
In our study, pouch compliance as well as other volumetry data did turn out as appropriate criteria for the characterization of the functional outcome after IPAA. This is in accordance with other trials [7, 19]. Especially the neorectal compliance, as well as the threshold volumes for first sensation, urge and the maximum tolerated volume were closely related to the functional outcome, but they correlated better with the median stool frequency than with continence. For continence, the integrity of anal sphincter resting pressure function seems to be more important, which is also in accordance with data from other trials [8, 20–22]. There is wide consent in the literature that global anal resting pressure deteriorates significantly after the pouch procedure [8, 20, 21, 23–25], with postoperative values as low as one half of the preoperative results [20], while an effect on the squeeze pressure is absent or irrelevant [8, 25, 26]. The reasons for this loss of internal anal sphincter activity may result from direct sphincter trauma during mucosectomy [27–29] or stapler anastomosis [21, 22, 30] or may result from insufficient efferent neuronal support [23, 31, 32]. Most of these studies used conventional anal manometry to investigate the significance of the anal sphincter function for the functional outcome after IPAA, which gives only a global view of the integrity of the anal sphincter. However, pressure distribution is not consistent over the anal HPZ neither radially nor longitudinally [33–35], and therefore, conventional manometry might miss some aspects of sphincter dysfunction caused by IPAA. The vector volume is probably a much better indicator of the sphincter function because it includes the functional length of the anal sphincter and therefore represents the overall amount of sphincter power. Additionally, the radial pressure distribution appeared as an interesting candidate parameter because high radial asymmetry was found to be associated with sphincter injuries as a result of vaginal delivery or fistula surgery [9–11].
The only study in which vector manometry was used in patients with a hand-sewn IPAA was performed by Kroesen and co-workers, who aimed to investigate whether the loss of internal anal sphincter function after IPAA is caused by direct sphincter trauma or rather by a lack of neuronal support [32]. There was a significant reduction in both anal resting and squeezing pressures and a significant increase in radial asymmetry after IPAA, but these changes were not restricted to the oral part of the sphincter, where mucosectomy and the formation of the anastomosis might have caused a localized sphincter trauma. Neurogenic damage was therefore thought to be more likely the cause of impaired function. However, vector-manometry data in this study were not related with the functional outcome.
We found the vector volume at rest to correlate significantly with the functional outcome in terms of continence. In accordance with the literature, the squeeze values did not demonstrate a convincing relationship to the functional outcome. [25, 36] Both urgency and the frequency of defecation were not characterized convincingly by any of the VM parameters but rather by parameters of pouch capacity and compliance. Sphincter asymmetry at rest in the HPZ was significantly higher in incontinent than in continent patients and did also demonstrate a good correlation with the degree of incontinence. However, this was only true if determined in the continuous pull-through technique, although the same trend was obvious in the station pull-through technique. Both vector volume and asymmetry were closer related to continence when determined in the HPZ of the sphincter which represents the proportion of the sphincter in which the mean pressure exceeds 50% of the maximum sphincter. The probable reason for this observation was that, from the segment of highest mean pressure, asymmetry increases and pressure decreases continuously in oral direction [34]. This oral low-pressure portion of the sphincter does not contribute a lot to the function but is fully included in the calculation of the asymmetry index and mean pressure for the entire sphincter, as indicated by higher mean pressures and lower asymmetry indices in the HPZ. Therefore, the portion of the sphincter with a mean pressure of at least 50% of the maximum level should be used for analysis, as earlier proposed by Jorge and Wexner [14].
Overall, vector-manometry parameters determined with the continuous pull-through technique appeared more reliable and better associated with the clinical outcome than data obtained with the station pull-through method. The station pull-through is thought to be more accurate in determining the single point pressures [37], but the continuous pull through is probably more appropriate in assessment of overall pressure profile [38] and therefore more suitable for 3-dimensional VM.
One major question is whether these 3-dimensional data are more valuable than conventional data. When vector volume at rest is compared to the mean resting pressure in the segment of highest mean anal pressure, which is pretty similar to conventional manometry, it was not convincingly better. Furthermore, for all VM parameters that were significantly correlated to functional outcome, this correlation was rather weak or moderate at best. Sensitivity and specificity to indicate incontinence after IPAA according to the incontinence diary were 63.6% and 59.1% for the vector-volume at rest in the high-pressure zone, which was slightly better than the accuracy of the mean pressure with corresponding values of 54.5% and 60%. Although the accuracy of the radial asymmetry was slightly better (sensitivity of 67% and specificity of 68%), overall these parameters appear to be of limited value to characterize the individual patient’s functional outcome.
Another problem might be that for radial asymmetry, a poor reproducibility has been described [39]. Therefore, although high radial asymmetry and low mean pressure and vector volume at rest seem to be indicators of poor continence, the clinical value is limited, as earlier proposed by others for VM in general [40, 41].
In summary, our data demonstrate that vector manometry characterizes continence after restorative proctocolectomy, whereas both urgency and frequency of defecation are better indicated by pouch physiology parameters like threshold volumes and compliance. A high vector volume at rest is a good parameter for superior anal sphincter function and points to a good continence, whereas (and) a low radial asymmetry appears to be a useful cofactor. As vector manometry is a time-consuming procedure and the 3-dimensional parameters contribute only mildly to the characterization of the overall functional outcome, with a limited (and their) value to predict the individual patient’s continence, it is mainly valuable to investigate anal sphincter function and pathophysiology in clinical trials on pouch surgery rather than in the clinical routine.
References
Michelassi F, Lee J, Rubin M, Fichera A, Kasza K, Karrison T, Hurst RD (2003) Long-term functional results after ileal pouch anal restorative proctocolectomy for ulcerative colitis: a prospective observational study. Ann Surg 238:433–441 (discussion 442–445)
Delaney CP, Fazio VW, Remzi FH, Hammel J, Church JM, Hull TL, Senagore AJ, Strong SA, Lavery IC (2003) Prospective, age-related analysis of surgical results, functional outcome, and quality of life after ileal pouch-anal anastomosis. Ann Surg 238:221–228
McGuire BB, Brannigan AE, O'Connell PR (2007) Ileal pouch-anal anastomosis. Br J Surg 94:812–823
Hahnloser D, Pemberton JH, Wolff BG, Larson DR, Crownhart BS, Dozois RR (2007) Results at up to 20 years after ileal pouch-anal anastomosis for chronic ulcerative colitis. Br J Surg 94:333–340
McIntyre PB, Pemberton JH, Wolff BG, Beart RW, Dozois RR (1994) Comparing functional results one year and ten years after ileal pouch-anal anastomosis for chronic ulcerative colitis. Dis Colon Rectum 37:303–307
Bullard KM, Madoff RD, Gemlo BT (2002) Is ileoanal pouch function stable with time? Results of a prospective audit. Dis Colon Rectum 45:299–304
Lewis WG, Miller AS, Williamson ME, Sagar PM, Holdsworth PJ, Axon AT, Johnston D (1995) The perfect pelvic pouch—what makes the difference? Gut 37:552–556
Williamson ME, Lewis WG, Miller AS, Sagar PM, Holdsworth PJ, Johnston D (1995) Clinical and physiological evaluation of anorectal eversion during restorative proctocolectomy. Br J Surg 82:1391–1394
Jorge JM, Habr-Gama A (2000) The value of sphincter asymmetry index in anal incontinence. Int J Colorectal Dis 15:303–310
Fynes MM, Behan M, O’Herlihy C, O’Connell PR (2000) Anal vector volume analysis complements endoanal ultrasonographic assessment of postpartum anal sphincter injury. Br J Surg 87:1209–1214
Damon H, Henry L, Barth X, Mion F (2002) Fecal incontinence in females with a past history of vaginal delivery: significance of anal sphincter defects detected by ultrasound. Dis Colon Rectum 45:1445–1450 (discussion 1450–1451)
Perry RE, Blatchford GJ, Christensen MA, Thorson AG, Attwood SE (1990) Manometric diagnosis of anal sphincter injuries. Am J Surg 159:112–116 (discussion 116–117)
Roberts PL, Coller JA, Schoetz DJ Jr., Veidenheimer MC (1990) Manometric assessment of patients with obstetric injuries and fecal incontinence. Dis Colon Rectum 33:16–20
Jorge JM, Wexner SD (1993) Anorectal manometry: techniques and clinical applications. South Med J 86:924–931
Vaizey CJ, Carapeti E, Cahill JA, Kamm MA (1999) Prospective comparison of faecal incontinence grading systems. Gut 44:77–80
Hueting WE, Gooszen HG, van Laarhoven CJ (2004) Sexual function and continence after ileo pouch anal anastomosis: a comparison between a meta-analysis and a questionnaire survey. Int J Colorectal Dis 19:215–218
Tomita R, Igarashi S (2007) Assessments of anal canal sensitivity in patients with soiling 5 years or more after colectomy, mucosal proctectomy, and ileal J pouch-anal anastomosis for ulcerative colitis. World J Surg 31:210–216
Tomita R, Kurosu Y, Munakata K (1996) Electrophysiologic assessments in pudendal and sacral motor nerves after ileal J-pouch-anal anastomosis for patients with ulcerative colitis and adenomatosis coli. Dis Colon Rectum 39:410–415
O'Connell PR, Pemberton JH, Brown ML, Kelly KA (1987) Determinants of stool frequency after ileal pouch-anal anastomosis. Am J Surg 153:157–164
Farouk R, Duthie GS, Bartolo DC (1994) Recovery of the internal anal sphincter and continence after restorative proctocolectomy. Br J Surg 81:1065–1068
Hallgren T, Fasth S, Delbro D, Nordgren S, Oresland T, Hulten L (1993) Possible role of the autonomic nervous system in sphincter impairment after restorative proctocolectomy. Br J Surg 80:631–635
Gosselink MP, West RL, Kuipers EJ, Hansen BE, Schouten WR (2005) Integrity of the anal sphincters after pouch-anal anastomosis: evaluation with three-dimensional endoanal ultrasonography. Dis Colon Rectum 48:1728–1735
Church JM, Saad R, Schroeder T, Fazio VW, Lavery IC, Oakley JR, Milsom JW, Tuckson W (1993) Predicting the functional result of anastomoses to the anus: the paradox of preoperative anal resting pressure. Dis Colon Rectum 36:895–900
Becker JM, LaMorte W, St Marie G, Ferzoco S (1997) Extent of smooth muscle resection during mucosectomy and ileal pouch-anal anastomosis affects anorectal physiology and functional outcome. Dis Colon Rectum 40:653–660
Pescatori M (1992) The results of pouch surgery after ileo-anal anastomosis for inflammatory bowel disease: the manometric assessment of pouch continence and its reservoir function. World J Surg 16:872–879
Reissman P, Piccirillo M, Ulrich A, Daniel N, Nogueras JJ, Wexner SD (1995) Functional results of the double-stapled ileoanal reservoir. J Am Coll Surg 181:444–450
Winter DC, Murphy A, Kell MR, Shields CJ, Redmond HP, Kirwan WO (2004) Perioperative topical nitrate and sphincter function in patients undergoing transanal stapled anastomosis: a randomized, placebo-controlled, double-blinded trial. Dis Colon Rectum 47:697–703
Ho YH, Tsang C, Tang CL, Nyam D, Eu KW, Seow-Choen F (2000) Anal sphincter injuries from stapling instruments introduced transanally: randomized, controlled study with endoanal ultrasound and anorectal manometry. Dis Colon Rectum 43:169–173
Farouk R, Drew PJ, Duthie GS, Lee PW, Monson JR (1996) Disruption of the internal anal sphincter can occur after transanal stapling. Br J Surg 83:1400
Silvis R, van Eekelen JW, Delemarre JB, Gooszen HG (1995) Endosonography of the anal sphincter after ileal pouch-anal anastomosis. Relation with anal manometry and fecal continence. Dis Colon Rectum 38:383–388
Morgado PJ Jr., Wexner SD, James K, Nogueras JJ, Jagelman DG (1994) Ileal pouch-anal anastomosis: is preoperative anal manometry predictive of postoperative functional outcome? Dis Colon Rectum 37:224–228
Kroesen AJ, Runkel N, Buhr HJ (1999) Manometric analysis of anal sphincter damage after ileal pouch-anal anastomosis. Int J Colorectal Dis 14:114–118
Taylor BM, Beart RW Jr., Phillips SF (1984) Longitudinal and radial variations of pressure in the human anal sphincter. Gastroenterology 86:693–697
Williams N, Barlow J, Hobson A, Scott N, Irving M (1995) Manometric asymmetry in the anal canal in controls and patients with fecal incontinence. Dis Colon Rectum 38:1275–1280
Morgado PJ Jr., Wexner SD, Jorge JM (1994) Discrepancies in anal manometric pressure measurement—important or inconsequential? Dis Colon Rectum 37:820–823
Scott NA, Pemberton JH, Barkel DC, Wolff BG (1989) Anal and ileal pouch manometric measurements before ileostomy closure are related to functional outcome after ileal pouch-anal anastomosis. Br J Surg 76:613–616
Coller JA (1987) Clinical application of anorectal manometry. Gastroenterol Clin North Am 16:17–33
McHugh SM, Diamant NE (1987) Anal canal pressure profile: a reappraisal as determined by rapid pullthrough technique. Gut 28:1234–1241
Clewing MKA, Buhr HJ (1999) Evaluation and validation of anal sphincter function by anal manometry. Langenbecks Arch Chir Suppl 99:397–402
Zbar AP, Kmiot WA, Aslam M, Williams A, Hider A, Audisio RA, Chiappa A, deSouza N (1999) Use of vector volume manometry and endoanal magnetic resonance imaging in the adult female for assessment of anal sphincter dysfunction. Dis Colon Rectum 42:1411–1418
Yang YK, Wexner SD (1994) Anal pressure vectography is of no apparent benefit for sphincter evaluation. Int J Colorectal Dis 9:92–95
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rink, A.D., Nagelschmidt, M., Radinski, I. et al. Evaluation of vector manometry for characterization of functional outcome after restorative proctocolectomy. Int J Colorectal Dis 23, 807–815 (2008). https://doi.org/10.1007/s00384-008-0473-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-008-0473-5