Abstract
Background and aims
Ileo pouch anal anastomosis (IPAA) is the standard restorative procedure for patients with ulcerative colitis and familial adenomatous polyposis, but its pros and cons have not been explored in depth. This study analyzed the long-term complications such as incontinence and sexual dysfunction after IPAA.
Patients and methods
Netherlands Society for Crohn’s disease and Ulcerative Colitis) A questionnaire on complications, sexual dysfunction, and continence was sent to all 137 members of the Netherlands Society for Crohn’s disease and Ulcerative Colitis who had IPAA; the questionnaire was returned by 111. Results of the questionnaire were compared with those of a meta-analysis on pooled incidences of complications after IPAA, as previously performed and reported.
Results
Pelvic sepsis was reported by 15.3% of respondents. The reported incidence of sexual dysfunction (19.8%), passive incontinence (23.4%), and soiling (39.3%) was significantly higher than that in the meta-analysis. Nevertheless, 90% of the population was satisfied with the results of the IPAA.
Conclusion
This study underlines that the operation itself, freeing patients of their disease, provides the major satisfaction and improvement of quality of life, even when patients have pouch-related complications such as sexual dysfunction and some degree of fecal incontinence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The pros and cons of the ileo pouch anal anastomosis (IPAA), the standard restorative procedure for patients with ulcerative colitis (UC) and familial adenomatous polyposis (FAP), have not been explored in full depth. Undergoing an IPAA procedure is not an essential step to cure UC or FAP but does offer a way in which to avoid permanent ileostomy and to improve quality of life. IPAA is an established procedure with an overall good outcome and a high satisfaction score. A recently performed meta-analysis [1], however, has shown that due to the relatively high complication rate an optimal quality of life is not always obtained. Therefore the ileo neorectal anastomosis (INRA) was developed as an alternative restorative procedure [2, 3], which theoretically overcomes the drawbacks of the IPAA procedure. The INRA technique is very laborious and technically demanding, and most of the theoretical advantages still await definite confirmation.
To assess the arguments for further development of the INRA technique we carried out a study on long-term complications known to interfere with quality of life such as incontinence and sexual dysfunction, using not only the above meta-analysis covering all relevant studies published in the past decade but also a questionnaire survey among patients who have an IPAA
Material and methods
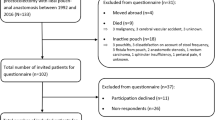
A detailed questionnaire was sent to all 137 members of the Netherlands Society for Crohn’s Disease and Ulcerative Colitis, Crohn en Colitis Ulcerosa Vereniging Nederland, CCUVN) who had an IPAA. The study was approved by the Board of CCUVN and was unique as the patients involved had undergone restorative surgery at the majority of Dutch centers rather than at only one single center. The patients had been operated on between 1989 and 2000. They were requested to fill out and return a general section on IPAA and a continence section based on the Vaizey score. The questionnaire was returned by 111 patients (81%; 35 men, 76 women; median age at operation 35.4 years, range 15–64), 93% of whom had been diagnosed as having UC before the IPAA procedure. Median follow-up was 3.5 years (0.4–12.5), in 101 cases (91%) longer than 1 year.
The findings of this questionnaire survey were compared with those of a meta-analysis [1]. The data of the meta-analysis were supplemented by a Medline and cross-reference search of studies reporting results from more than 50 IPAA procedures. Two authors independently performed the data extraction on epidemiological characteristics, diagnosis, and type of operation, pouch-related complications, pouch failure, and functional results. Estimates of pouch failure, pouch-related complications, and functional results were described as pooled percentages with 95% confidence interval.
The questionnaire
The general questionnaire contained questions on epidemiology, surgical procedures, comorbidity, medication, complications, sexual function, and functional results after IPAA. Complications such as pelvic sepsis, fistula, stricture, and pouchitis were explained in the questionnaire to help the patients provide reliable answers to questions on the occurrence of these complications in their postoperative course. Sexual dysfunction was subdivided into impotence, retrograde ejaculation, and dyspareunia. The complications were explained as follows:
-
Pelvic sepsis: abscess in the pelvis with a need for drainage by puncture or operation and production of pus for at least 1 day, leakage or dehiscence of the suture line of the pouch, pelvic/perineal wound infection
-
Fistula: any pouch-related fistula between pouch and surrounding structures or vagina, without pelvic sepsis
-
Stricture: narrowing of the suture line above the anus with a need for dilatation
-
Sexual dysfunction: retrograde ejaculation and impotence in men, dyspareunia in women
-
Soiling: soiling, spotting in underwear for at least once a week
-
Passive fecal incontinence: fecal loss for at least once a week
-
Urge fecal incontinence: inability to defer defecation more than 15 min after first urge
Fecal continence, the Vaizey score
The Vaizey et al. [4] score was also used to investigate fecal incontinence to gain an objective outcome of the IPAA. This incontinence scale combines the assessment of incontinence for solid stool, liquid stool, and gas, the alteration in life-style, the need to wear a pad or plug, the requirement of antidiarrheal medicine, and the ability to defer defecation. Perfect continence, minor, moderate, and severe incontinence are (arbitrarily) set on a Vaizey score of 0–5, 6–10, 11–15, and 16–28, respectively (see Table 1).
Satisfaction and quality of life
Patients were questioned on several indirect parameters for their general quality of life after IPAA, including restrictions in daily life, satisfaction with the procedure, and willingness to undergo the procedure again, if necessary. Quality of life was also expressed in a visual analogue scale score on a scale of 0–10.
Statistical analysis
The results obtained from the questionnaire were compared to those of the meta-analysis, focusing on pelvic sepsis, fistula, strictures, sexual dysfunction and continence. Using a normal approximation we compared the proportions with complications as reported in the questionnaire study with the pooled data from the meta-analysis. Differences with a (two-tailed) P value of 0.05 or less were considered statistically significant.
Results
Complications
The incidence of complications and sexual function are presented in Table 2. Of the questionnaire respondents 41% reported no complications. Pelvic sepsis was the most common and severe pouch-related complication (15.3%). At least one or more episodes of pouchitis was reported by 38%, which was not significantly higher than the comparable figure in the meta-analysis. Most of the of other pouch-related complications were also not significantly higher than the incidences calculated in the meta-analysis. The overall incidence of sexual dysfunction was 19.8%, also not significantly higher than in the meta-analysis.
Continence
Table 3 compares functional results and continence as reported in the questionnaire study with those of the meta-analysis. The 24-h defecation frequency was not significantly higher than that in the meta-analysis; 43% of the patients reported full continence. The incidence of passive incontinence and soiling were significantly higher than reported in the meta-analysis, and urgency was not significantly higher. Table 4 presents the results using the Vaizey score; on this scale 9.8% of this population had severe incontinence. The median Vaizey score was 7 (Table 5).
Satisfaction and quality of life
Of the questionnaire respondents 90% were satisfied with the IPAA, and 95% would undergo the procedure again; 71% felt no restriction in general after IPAA. IPAA improved general quality of life in 78% of the population. The general satisfaction assessed with a VAS score was 8 (range 3–10).
Discussion
This study based on a questionnaire with a high response rate shows a high number of pouch-related complications, a high incidence of sexual dysfunction in both women and men, and a varying degree of incontinence. This study differs from other reports because it is free of publication and investigator bias, although it does suffer from selection bias. The results are anonymous and reflect results from the majority of Dutch centers performing restorative surgery. Approximately 120 pouch operations are performed yearly in more than 10 centers in The Netherlands. The 111 respondents to this questionnaire study are representative not of the entire population of IPAA patients but of those who have joined the CCUVN. It is not possible to speculate why patients join the CCUVN. Is it because they are assertive, dissatisfied, preoccupied, or lonely, or do they want to exchange experience and help their fellow patients? The results are less positive than those obtained in larger centers who report better figures on complications, sexual dysfunction, and continence. It is remarkable that in spite of these apparently mediocre results, patients rate their quality of life and their satisfaction with the procedure as high.
Differences in outcome regarding sexual function and continence between the meta-analysis studies and this questionnaire investigation can also be partly explained by a potential surgeon or physician bias, either because this does not adequately come into the discussion, or because of the patient’s tendency to underreport this very personal issue.
The figures on sexual dysfunction and incontinence are both very high. Sexual dysfunction after IPAA is a difficult endpoint to measure. Only a few studies describe sexual dysfunction in detail [5, 6]. Definition and completeness in scoring of these endpoints vary between studies, and few use a validated questionnaire. The present questionnaire study focused only on impotence, retrograde ejaculation, and dyspareunia after IPAA, and the respective incidences were much higher than those reported in the literature. A prospective study with validated questionnaires on sexual function in a large population before and after IPAA should give more insight the effect of this procedure on sexual function as an outcome measure for quality of life after restorative surgery.
To assess continence as accurately as possible we used the Vaizey scoring system. This is a validated incontinence scale that is simple to use and reproducible. It combines components of generally accepted scales such as the Jorge and Wexner [7], Pescatori et al. [8], and American Medical System scores and also includes an assessment of fecal urgency and the need to take antidiarrheal medication. The wide variation in presentation of functional results in the literature and the use of different continence scales make it very difficult to combine the results as they have been published. Even with strict definitions and the validated Vaizey scale the incidence of incontinence is much higher than reported in the literature. Even though the outcomes reported here are inferior to most reports in the literature, it is surprising that this also does not seem to affect the overall quality of life or the satisfaction with the procedure. Quality of life after IPAA in this study showed good results, with scores that are only slightly inferior to those of a population-based reference group [6, 9, 10, 11, 12]. This study underlines that the operation itself, freeing patients of their disease and their stoma, provides a major satisfaction and improvement in quality of life, even when patients have pouch-related complications, sexual dysfunction, or considerable limitations in pouch function.
Although our findings may lead to the impression that the patients studied represent a negative selection, this is not reflected in the overall rate of satisfaction expressed with the procedure or the willingness of the patients to undergo it again if necessary. This high level of overall satisfaction thus suggests that the populations examined included in other studies reflect a positively biased selection of patients.
Reference
Hueting WE, Buskens E, van der Tweel I, Gooszen HG, van Laarhoven CJHM (2001) Ileo pouch anal anastomosis: meta analysis on results and complications of 44 studies with 9435 patients. Colorectal Dis 3 [Suppl 1]:19
Laarhoven CJ van et al (1999) Ileoneorectal anastomosis: early clinical results of a restorative procedure for ulcerative colitis and familial adenomatous polyposis without formation of an ileoanal pouch. Ann Surg 230:750–757
Andriesse GI et al (2001) Functional results and visceral perception after ileo neo-rectal anastomosis in patients: a pilot study. Gut 48:683–689
Vaizey CJ, Carapeti E, Cahill JA, Kamm MA (1999) Prospective comparison of faecal incontinence grading systems. Gut 44:77–80
Metcalf AM, Dozois RR, Kelly KA (1986) Sexual function in women after proctocolectomy. Ann Surg 204:624–627
Damgaard B, Wettergren A, Kirkegaard P (1995) Social and sexual function following ileal pouch-anal anastomosis. Dis Colon Rectum 38:286–289
Pescatori M, Anastasio G, Bottini C, Mentasti A (1992) New grading and scoring for anal incontinence. Evaluation of 335 patients. Dis Colon Rectum 35:482–487
Jorge JM, Wexner SD (1993) Etiology and management of fecal incontinence. Dis Colon Rectum 36:77–97
Steens J et al (2000) Limited influence of pouch function on quality of life after ileal pouch-anal anastomosis. Hepatogastroenterology 47:746–750
van Duijvendijk P et al (2000) Quality of life after total colectomy with ileorectal anastomosis or proctocolectomy and ileal pouch-anal anastomosis for familial adenomatous polyposis. Br J Surg 87:590–596
Dunker MS, Bemelman WA, Slors JF, van Duijvendijk P, Gouma DJ (2001) Functional outcome, quality of life, body image, and cosmesis in patients after laparoscopic-assisted and conventional restorative proctocolectomy: a comparative study. Dis Colon Rectum 44:1800–1807
Jimmo B, Hyman NH (1998) Is ileal pouch-anal anastomosis really the procedure of choice for patients with ulcerative colitis? Dis Colon Rectum 41:41–5
Acknowledgements
The authors are indebted to Erik Buskens, MD, of the Julius Center for General Practice and Patient-Oriented Research, for his critical comments and suggestions on the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hueting, W.E., Gooszen, H.G. & van Laarhoven, C.J.H.M. Sexual function and continence after ileo pouch anal anastomosis: a comparison between a meta-analysis and a questionnaire survey. Int J Colorectal Dis 19, 215–218 (2004). https://doi.org/10.1007/s00384-003-0543-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-003-0543-7