Abstract
Background
Specific symptom outcomes after craniovertebral decompression for patients with Chiari type 1 malformation, without accompanying syringomyelia, are not well characterised and poorly reported.
Methods
We performed a retrospective review of all patients diagnosed with Chiari type 1, without syringomyelia, who underwent craniovertebral decompression in our unit.
Results
We identified 129 individuals with a minimum of 2 years’ follow-up. The most common pre-operative symptoms were pressure dissociation headaches (78%), visual disturbances (33%), dizziness/balance disturbances (24%) and blackouts (17%). The symptoms most likely to respond to surgery included Valsalva-induced headache (74% response, p < 0.0001) and blackouts (86% response, p < 0.001).
Conclusions
After successful craniovertebral decompression, most patients presenting with pressure dissociation headaches and blackouts will improve. However, the large variety of other symptoms patients often present with may not improve after surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chiari type 1 malformation consists of herniation of the cerebellar tonsils into the upper cervical spinal canal. This cerebellar ectopia impedes normal movement of cerebrospinal fluid (CSF) across the craniovertebral junction, causing the affected individual to suffer from typical CSF pressure-dissociation headaches, brought on by coughing, sneezing, laughing, blowing up party balloons or simply bending over. Tonsillar pressure on the brain stem and upper cervical cord can also produce a variety of somatic sensory disturbances and subtle motor symptoms, as well as disturbances of bulbar and lower cranial nerve function.
The specific responses of these various symptoms to decompressive surgery are not well documented, and when surgical results are reported, data are often derived from small numbers of cases. Furthermore, reported outcomes are often summarised in an understandably general way, into categories such as cured, better, same or worse. The Chicago Chiari Outcome Score (CCOS) does provide a means of quantifying outcomes [1], although the assessments remain somewhat subjective, offering general outcomes in broad categories.
In this paper, we have focussed on the specific symptom outcome in 129 patients with Chiari type 1, without syringomyelia, who underwent decompressive surgery using a generally uniform operative technique. The report does not include patients with Chiari type 1 and syringomyelia, who form a different cohort of our patients and who are the subject of a separate study. For this reason also, we have not attempted to audit all aspects of craniovertebral decompression surgery, such as early gains and complications We have aimed, instead, to identify which symptoms are likely to respond, in the medium to longer term, to an anatomically successful craniovertebral decompression. We have further tried to explain why some symptoms, in contrast to others, improve after surgery.
Materials and methods
To audit the outcome of this method of craniovertebral decompression, clinical notes, operation records, electronic records and radiological images were reviewed for all patients who underwent craniovertebral decompression for Chiari type 1 malformation without associated syringomyelia in our unit by the senior author, up until April 2015. Patients were only included for analysis if adequate information was clearly documented regarding their pre- and post-operative clinical symptoms and signs. Documentation had to be explicit as regards whether a specific symptom was cured, improved, unchanged or worse. Patients were excluded if this information was not clear in the records. Patients were also excluded if a period of follow-up of less than 24 months had passed since their surgery. Furthermore, if, despite persisting symptoms, follow-up imaging had either not been done, or if such imaging showed persisting anatomical abnormalities, which were clearly responsible for the patient symptoms (i.e. inadequate decompression), then these patients were also excluded from our analysis. This was done, not to exclude surgical failures from our series, but because we were assessing the symptomatic benefit that can be achieved if the underlying anatomical abnormality at the craniovertebral junction is adequately corrected. In total, 197 patients were identified. For these patients, only sparse information could be identified in 22 cases, beyond basic data such as date of birth and the date and nature of their surgery; all of these patients were operated on before 1997. Of the remaining patients, information regarding specific symptoms, including presentation and outcome, was inadequate in 46 cases. These data limitations resulted in usable outcome measures being available in only 129 of the original 197 cases.
Subject to the above selection criteria, patients’ symptoms were itemised as being either a specific, commonly reported complaint, or as belonging to a group of less frequently occurring symptoms. Baseline characteristics, including age at surgery, gender and length of follow-up, were noted for all patients. For outcome measurement, we used the pain and non-pain measures of the Chicago Chiari Outcome Scale, these being as follows: “resolved”, “improved”, “unchanged” or “worse”. Any change in symptoms after surgery was recorded on an ordinal scale, with the “worse”, “unchanged”, “improved” and “resolved” categories being assigned values of − 1, 0, 1 and 2, respectively. In order to then assess whether individual symptoms had improved post-operatively, the “improved” and “resolved” categories were first combined. The data were then analysed using a sign test, to assess whether the change in symptoms was significantly different to zero.
The nature of the specific symptoms that we recorded is generally made obvious by the terminology used, e.g. Valsalva headaches, limb sensory symptoms. The term “Body symptoms” refers to the variety of non-specific somatic sensory symptoms that patients often described as numbness or tingling on the trunk or back. One particular category, however, warrants further definition. The term “blackouts” is used frequently by patients, in describing their symptoms. In recording this as a symptom, we were referring to a volunteered history of collapse, sometimes (but not invariably) induced by a Valsalva-like manoeuvre, or by an episode of physical exertion. To be included in this category, such events needed to be unaccompanied or preceded by any aura or other neurological symptoms. They were also required, when witnessed, not to have any features suggestive of epileptic seizures. Patient also had to have regained awareness immediately after the collapse, without displaying any features suggestive of any other, underlying pathology. Several of the patients in this group had also been reviewed by a neurologist or a cardiologist, to exclude epilepsy or cardiac pathology as a cause of the blackouts.
Surgical technique
There are several different techniques adopted by surgeons, in carrying out a craniovertebral decompression for Chiari type 1 malformation. The only detail they have in common is removal of bone, and even then, the extent of bone removal will vary from one surgeon to another. Dural opening, its extent and whether or not it is subsequently repaired, are details over which practices differ. So too is whether or not the cerebellar tonsils are reduced in size and, if so, by what method. Techniques of any subsequent duraplasty or cranioplasty and the materials used are also details which vary from one surgeon to another.
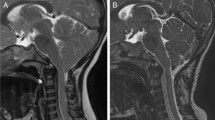
In our series, all patients underwent bony removal between the inferior nuchal line and the posterior rim of the foramen magnum, together with removal of the posterior arch of C1. The dura was opened as an inverted “U”, the resultant flap being sewn down taut across the spinous process of C2. The dural edges were also hitched up laterally across the craniovertebral junction. All patients underwent tonsillar reduction, usually using bipolar diathermy but occasionally by sub-pial aspiration of tissue. In some cases the tonsillar residues were hitched up to the adjacent, cut dural edges, in order to ensure patency of Magendie. Dural patch grafting was never performed and wound closure consisted of approximation of muscle, fat and skin, in layers. This method of closure creates a small pseudomeningocoele in the sub-occipital plane, which acts as an artificial cisterna magna, into which the IVth ventricle opens freely, and which itself communicates freely with the basal cisterns and the spinal CSF channels.
Results
A total of 129 patients were identified, with a mean age at surgery of 37 ± 12 years, of whom the majority (71%) were female. The patients had minimum follow-up of 24 months with median interval of 36 months.
We identified 19 separate symptoms or symptom groups for analysis (Table 1, Fig. 1). A minority of patients (28%) presented with just one symptom but most exhibited two or more, with a maximum of eight concurrent symptoms reported in two patients. The most commonly reported symptom was Valsalva-related headache (78%). Next most common were visual disturbances (33%), with non-specific visual blurring reported by 22 patients, one patient complaining of transient visual loss and 4 patients describing oscillopsia. Diplopia was complained of by 5 patients, one of whom exhibited a VIth nerve palsy. Nystagmus was recorded as a physical sign in 11 patients. Dizziness or subjective balance disturbances troubled a quarter of our patients (Fig. 1).
Twenty-two patients reported blackouts as a symptom. Fifteen of these 22 described the blackout as being associated with Valsalva manoeuvres, such as laughing, coughing sneezing and straining. Of these 15, one described a flushing episode preceding the collapse. Another patient described typical pressure dissociation headache developing just prior to the collapse. In two patients, the blackouts were associated with non-specific headache and, in one patient, non-specific dizziness. One patient experienced regular blackouts on the toilet, albeit not related to straining; he also experienced alternating hemiplegia, hemisensory loss and paraesthesias lasting for 30 min after the blackout. In three patients, the underlying cause of the blackouts was unclear.
The responses of symptoms to surgery are summarised and presented in Table 1 and Fig. 2. The symptom which improved, proportionately, most often was blackouts, with just over three-quarters (17/22) of patients reporting that this was resolved after surgery, and a further one in ten (2/22) reporting that the symptom lessened in frequency. Other symptoms showing significant improvement were Valsalva-related headaches, visual disturbances, dizziness/balance issues and sensory symptoms in the upper limbs (in all cases with p < 0.001).
No significant relationships were identified between age, gender and the degree of any symptom improvement.
Discussion
In our cohort of 129 cases, pressure dissociation headaches showed the most consistently positive response to craniovertebral decompression, in terms of total numbers. Three quarters of our patients with such headaches responded to surgery and almost two-fifths were considered as being cured at long-term follow-up. In another published, long-term follow-up of 38 patients operated for Chiari type 1 malformation without syringomyelia, headache improved in 87% of patients [2], a finding similar to our own. In another, 12-month follow-up of 29 patients with diagnosed Chiari type 1 malformation, without syringomyelia, 93% improved after surgery [3].
The second most common clinical feature in our patients consisted of visual disturbances. Overall, these symptoms or signs improved following craniovertebral decompression in a little over half of affected patients. Other publications have noted that between 82 and 100% of ocular symptoms may resolve after surgery, in patients with Chiari type 1 malformation, albeit cases with associated syringomyelia in some series [4]. Nystagmus and oscillopsia are particularly well-recognised features of Chiari type 1 malformation and are thought to be due to a combination of brainstem and cerebellar dysfunction, caused by the ectopic position of the cerebellum. Both can improve after successful suboccipital craniectomy [2]. The physiological basis of other, non-specific visual symptoms is not as clear but such features have also been described by other groups [4].
Dizziness and balance problems made up one of the largest groups of non-specific symptoms in our case series, affecting about a quarter of our patients. Interestingly, none of these patients had any demonstrable findings on clinical examination, i.e. no evidence of vestibular, cerebellar or gait disturbance, and not displaying any other neurological signs. What they described were subjective feelings of being unbalanced, using words such as giddy, dizzy, unsteady and wobbly, and so created a definable symptom group. Just over half of the patients in this group responded to craniovertebral decompression. It is possible that these patients had been affected by subtle, long-tract or vestibular connection dysfunction, which improved following dis-impaction of the cerebellar tonsils and decompression of the brainstem. In a prospective study of 10 patients with Chiari type 1 malformation, assessing in particular their neuro-opthamological/otological symptoms, 6 patients were noted to have presented with vertigo/dizziness and 4 improved after craniovertebral decompression [5].
Almost a quarter of our patients presented with abnormal sensory symptoms, mainly in the upper limbs. Of these, almost half showed a statistically significant response after surgery. Our patient cohort did not include patients with syringomyelia so we can reasonably infer that such somatic sensory disturbances result from subtle compression of the ascending tracts, or sensory relay nuclei at the cervico-medullary junction.
Interestingly, in our series, the symptom which showed, proportionally, the greatest response to decompression was that of blackouts. Almost 9 out of 10 of our patients who had been affected improved significantly after decompression. Blackouts are usually regarded as a rare primary presentation of Chiari type 1. They are, however, a not uncommon component of the overall symptom profile, certainly in our patient cohort. The mechanism underlying such episodic losses of consciousness, with full recovery, is not clear. Tests for epilepsy or cardiac arrhythmias usually yield normal results. Intermittent medullary compression, caused by the herniated cerebellar tonsils, seems an unlikely mechanism, given that full recovery usually follows each blackout. Vertebral arterial compression is also unlikely to occur given that, during surgical decompressions for Chiari type 1, these vessels are not usually seen to be compromised. Transient impairment of the ascending reticular activating system has been proposed as a mechanism [6]. Interruption of the central sympathetic pathways, leading to postural hypotension, is another possibility. Blackouts in Chiari type 1 patients have also been attributed to postural orthostatic tachycardia syndrome [7, 8], and these symptoms have been reported to resolve after decompressive surgery [8]. We therefore consider that neurological examination should be a part of the routine clinical assessment of patients who present with orthostatic syncope.
Surgery for Chiari type 1 is seldom mandatory but it may be considered advisable if a patient reports having suffered repeated blackouts, which are clearly precipitated by Valsalva-like manoeuvres. Other blackouts, which are not clearly related to CSF pressure dissociation at the craniovertebral junction, are more likely to have a benign basis. They may, nevertheless, cause considerable distress to the affected patient, and noting our high rate of improvement after decompression surgery, we feel that such symptoms may reasonably tip the balance in favour of surgical intervention, in an individual case.
Limitations
This is a retrospective review of operated patients and, as such, may be subject to observation bias, recall and selection bias. No formal and validated scoring system to assess each individual symptom was used as these do not exist. Instead, parts of the CCOS were used as this is a validated system in patients with Chiari I malformation. Development and validation of more nuanced scoring systems would be useful. Prospective studies with validated scoring systems, possibly by the use of local or national patient registries, would help patient and clinician in determining which symptoms may or may not improve after surgery.
Conclusion
When patients with Chiari type 1 hindbrain hernia undergo an anatomically adequate craniovertebral decompression, which successfully establishes satisfactory CSF movement across the craniovertebral junction, their presenting Valsalva-induced, pressure-dissociation headaches will resolve in most cases. Blackouts, when part of the overall clinical profile, will also cease in the majority of cases. Visual disturbance and subjective dizziness or balance problems, as well as somatic sensory symptoms, stand about an even chance of improving. Other symptoms do not respond as well, even to an anatomically satisfactory decompression. Overall, it would appear that symptoms with an identifiable underlying pathophysiological mechanism, such as pressure-dissociation headaches caused by restricted CSF flow, or oscillopsia resulting from compression of brainstem structures, will be improved by an adequate decompression. We can be less certain as to how well other symptoms may respond.
Abbreviations
- CSF:
-
Cerebrospinal fluid
- CCOS:
-
Chicago Chiari Outcome Scale
References
Aliaga L, Hekman KE, Yassari R, Straus D, Luther G, Chen J, Sampat A, Frim D (2012) A novel scoring system for assessing Chiari malformation type I treatment outcomes. Neurosurgery 70(3):656–664 discussion 664-665
Giammattei L, Messerer M, Daniel RT, Aghakhani N, Parker F (2017) Long term outcome of surgical treatment of Chiari malformation without syringomyelia. J Neurosurg Sci. doi: 10.23736/S0390-5616.17.04063-2
Beretta E, Vetrano IG, Curone M, Chiapparini L, Furlanetto M, Bussone G, Valentini LG (2017) Chiari malformation-related headache: outcome after surgical treatment. Neurol Sci 38(Suppl 1):95–98
Rowlands A, Sgouros S, Williams B (2000) Ocular manifestations of hindbrain-related syringomyelia and outcome following craniovertebral decompression. Eye (Lond) 14(Pt 6):884–888
Goldschagg N, Feil K, Ihl F, Krafczyk S, Kunz M, Tonn JC, Strupp M, Peraud A (2017) Decompression in Chiari malformation: clinical, ocular motor, cerebellar, and vestibular outcome. Front Neurol 8:292
Wieshmann U, Meierkord H (1995) Cough syncope with hypertension-caused by brainstem compression? Eur J Neurol 2(5):498–500
Nogués M, Delorme R, Saadia D, Heidel K, Benarroch E (2001) Postural tachycardia syndrome in syringomyelia: response to fludrocortisone and beta-blockers. Clin Auton Res 11(4):265–267
Prilipko O, Dehdashti AR, Zaim S, Seeck M (2005) Orthostatic intolerance and syncope associated with Chiari type I malformation. J Neurol Neurosurg Psychiatry 76(7):1034–1036
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Joshua Pepper and Ahmed Elhabal. The first draft of the manuscript was written by Joshua Pepper and all authors commented on or revised previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
For this type of study (retrospective study), formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on CSF Circulation
Rights and permissions
About this article
Cite this article
Pepper, J., Elhabal, A., Tsermoulas, G. et al. Symptom outcome after craniovertebral decompression for Chiari type 1 malformation without syringomyelia. Acta Neurochir 163, 239–244 (2021). https://doi.org/10.1007/s00701-020-04631-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-020-04631-z