Abstract
Aim
To systematically review microwave ablation (MWA) protocols, safety, and clinical efficacy for treating bone tumors.
Materials and methods
A systematic literature search was conducted using PubMed, the Cochrane Library, EMBASE, and Web of Science database. Data concerning patient demographics, tumor characteristics, procedure, complications, and clinical outcomes were extracted and analyzed.
Results
Seven non-comparative studies (6 retrospective, 1 prospective) were included accounting for 249 patients and 306 tumors (244/306 [79.7%] metastases; 25/306 [8.2%] myelomas, and 37/306 [12.1%] osteoid osteomas [OO]). In malignant tumors, MWA power was 30–70 W (except in one spinal tumors series where a mean power of 13.3 W was used) with pooled mean ablation time of 308.3 s. With OO, MWA power was 30–60 W with mean ablation time of 90–102 s. Protective measures were very sporadically used in 5 studies. Additional osteoplasty was performed in 199/269 (74.0%) malignant tumors. Clinically significant complications were noted in 10/249 (4.0%) patients. For malignant tumors, estimated pain reduction on the numerical rating scale was 5.3/10 (95% confidence intervals [95%CI] 4.6–6.1) at 1 month; and 5.3/10 (95% CI 4.3–6.3) at the last recorded follow-up (range 20–24 weeks in 4/5 studies). For OO, at 1-month follow-up, effective pain relief was noted in 92.3–100% of patients.
Conclusion
MWA is effective in achieving pain relief at short- (1 month) and mid-term (4–6 months) for painful OO and malignant bone tumors, respectively. Although MWA seems safe, further prospective studies are warranted to further assess this aspect, and to standardize MWA protocols.
Key Points
• Large heterogeneity exists across literature about ablation protocols used with microwave ablation applied for the treatment of benign and malignant bone tumors.
• Although microwave ablation of bone tumors appears safe, further studies are needed to assess this aspect, as current literature does not allow definitive conclusions.
• Nevertheless, microwave ablation is effective in achieving pain relief at short- (1 month) and mid-term (4–6 months) for painful osteoid osteomas and malignant bone tumors, respectively.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Bone is the third most frequent site of metastasis, preceded by lung and liver [1]. These commonly originate from breast, prostate, thyroid, and lung cancers [2]. Skeletal metastases are often painful, requiring palliative treatments [3, 4]. On the other hand, osteoid osteoma (OO) is the most common primary benign painful bone tumor [5].
Percutaneous thermal ablation is a well-established treatment for OO and skeletal metastases, with the largest experience currently being available with radiofrequency ablation (RFA) and cryoablation (CA) [6,7,8,9,10,11,12,13]. More recently, microwave ablation (MWA) has integrated into the armamentarium of percutaneous ablation techniques. MWA relies on an electromagnetic field (915 MHz or 2.45 GHz) applied to the target tumor through antenna(e). The electromagnetic field forces the dipole to continuously realign with its main direction, thus producing frictional energy that is converted into heat, which finally results into a coagulative necrosis. Theoretically, MWA is relatively insensitive to tissue characteristics (e.g., impedance and perfusion) [14], and the MWA energy can therefore radiate through all biological tissues, rendering this source of energy particularly powerful in creating large ablation zones within few minutes. Accordingly, MWA has been extensively applied for the treatment of liver tumors [15,16,17,18] that require large ablation areas to optimize local tumor control. However, validated evidence regarding the applications of MWA in the field of bone tumors is still limited to few case series [19,20,21,22,23,24,25], and it remains unclear whether such a powerful tool may be safely and effectively applied to bone tumors that are prone to many thermal-mediated complications including secondary fractures and neuro-cutaneous damages [26, 27]. Accordingly, we conducted this systematic literature review to evaluate MWA protocols, safety, and clinical efficacy in treating bone tumors.
Materials and methods
This systematic review was conducted as per the “Preferred Reporting Items for Systematic Reviews” and Meta-Analyses (PRISMA) guidelines (http://www.prisma-statement.org).
Search strategy
Using PubMed, the Cochrane Library, EMBASE, and Web of Science databases, we conducted a search for published studies between January 2005 and April 2020. The keywords researched were “microwave ablation” and “bone tumors.”
Abstracts were reviewed for relevance, and all the articles with a relevant abstract were reviewed for consideration of inclusion. Moreover, the reference lists of all relevant articles were manually searched for relevant publications. Duplicate results were removed. Following this, articles were included in the final analysis when all the following inclusion criteria were met:
-
Reporting on percutaneous imaging-guided MWA of benign/malignant bone tumors with or without subsequent bone consolidation;
-
Reporting at least one clinical outcome (i.e., local tumor control; pain management; functional improvement) and complications following bone tumor MWA;
-
Clear indication of the retrospective or prospective study design;
-
Inclusion of a cohort of at least 10 patients;
-
English literature.
Articles were not included if one or more of the following criteria were noted:
-
Animal and experimental laboratory studies;
-
Narrative or systematic reviews and meta-analyses;
-
Surgical series performing open rather than percutaneous MWA.
The research and inclusion/exclusion process were performed in consensus by two investigators (R.L.C. and G.D.R. with 6 and 2 years of experience, respectively, in interventional bone oncology), who assessed the titles and abstracts for eligibility. The full texts of the potentially eligible studies were further reviewed in consensus by the same two investigators, to verify the inclusion and exclusion criteria and collect data useful for the current analysis.
Study quality assessment
The quality of the studies included in the final analysis was appraised in consensus by the aforementioned two investigators. Quality assessment was conducted according to the Methodological Index for Non-Randomized Studies (MINORS) criteria [28]. This scale evaluates studies according to 8 different items for non-comparative studies including a clearly stated aim, enrollment of consecutive patients, prospective data collection, endpoints appropriate to the aim of the study, unbiased assessment of the study endpoint, follow-up period appropriate to the aim of the study, loss to follow-up < 5%, and prospective calculation of the study sample size. Four additional items (i.e., adequate control group, contemporary groups, baseline equivalence of groups, adequate statistical analyses) are additionally evaluated in case of comparative studies. Each item is allocated a score of 0, 1, or 2 points when the investigated item is not reported, inadequately, or adequately reported, respectively. Therefore, the ideal scores are 16 and 24 for non-comparative and comparative studies, respectively. We considered non-comparative studies scoring 0–4 as of very low quality; those scoring 5–8 of low quality; those scoring 9–12 of moderate quality; and those scoring 13–16 of high-quality. Similarly, in case of comparative studies, scores between 0 and 6, 7 and 12, 13 and 18, and 19 and 24 indicated very low-, low-, moderate-, and high-quality studies, respectively.
Data extraction and analysis
Included articles were analyzed according to the benign or malignant nature of the treated tumors. Data concerning patient demographics, tumor characteristics, procedural variables, complications, and clinical outcomes were extracted and further analyzed.
For studies reporting pain changes following MWA of malignant bone tumors, we calculated such change according to a 0–10 numerical rating scale (NRS) for all the included studies. The I2 test was performed to assess homogeneity among papers. Pain relief was analyzed at 1-month follow-up, and whenever possible at the last recorded follow-up. All the other results (i.e., demographics, tumor characteristics, procedure-related variables, complications, pain reduction in benign tumors, and local tumor control in malignant bone tumors) were reported descriptively due to heterogeneous data reporting across studies, which hindered further analyses.
Categorical variables were provided as absolute numbers and percentages with 95% confidence intervals (CI). Continuous variables were provided as means and medians. Statistical analysis was performed with MedCalc 15.0 software (MedCalc).
Results
Eligible studies and quality assessment
A flowchart summarizing study selection is shown in Fig. 1. We identified 91 manuscripts in the initial screening, and after evaluating abstracts and full texts, 22 were selected for full-text assessment. Eventually, 7 studies (6 retrospective, 1 prospective) [19,20,21,22,23,24,25] published between 2014 and 2019 were included according to inclusion/exclusion criteria.
All studies were non-comparative; 5 studies were of low quality (scoring 7 or 8), and two of moderate quality (both scoring 10). Baseline characteristics of included studies are summarized in Table 1. Five studies reported exclusively on malignant bone tumors [19, 21, 23,24,25], and two exclusively on OO [20, 22].
Study population
Two hundred forty-nine patients (139 males, 110 females; mean age ranging between 56.0 and 69.4 years in patients with malignant tumors, and between 13.3 and 20.7 years in patients with OO) were included.
Overall, 306 tumors (with mean size ranging between 2.6 and 4.0 cm in malignant tumors, and between 0.5 and 0.8 cm in OO) were included. Among included tumors, there were 244/306 (79.7%; 95% CI 74.8–84.1%) bone metastases, 25/306 (8.2%; 95% CI 5.4–11.8) myelomas, and 37/306 (12.1%; 95% CI 8.7–16.3) OO. Tumors were located in the spine (135/306 [44.1%]; 95% CI 38.5–49.9), pelvis (105/306 [34.3%]; 95% CI 29.0–39.9), long bones (54/306 [17.7%]; 95% CI 13.5–0.2), and other bone sites (12/306 [3.9%]; 95% CI 2.0–6.7). Three studies [21, 23, 24] reported the radiographic appearance of 159 (159/306 [52.0%]; 95% CI 46.2–57.7) tumors: 117/159 (73.6%; 95% CI 66.0–80.3) were lytic, 18/159 (11.3%; 95% CI 6.8–17.3) sclerotic, and 24/159 (15.1%; 95% CI 9.9–21.6) mixed.
Procedure-related results
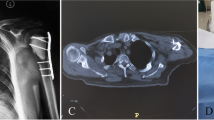
In five studies, computed tomography (CT) was used to guide MWA [19, 22,23,24,25]; Pusceddu et al [21] used combined CT/fluoroscopy; and Rinzler et al [20] cone beam CT. General anesthesia was used in 136 (136/249 [54.6%]; 95% CI 48.2–60.9) patients from 4 studies [20, 22, 23, 25], and treatment was provided on an in-patient basis to 135 (135/249 [54.2%]; 95% CI 47.8–60.5) patients from 4 studies [21, 23,24,25]. Intraprocedural biopsy of the target tumor was reported in 3 studies [22, 23, 25].
Data regarding MWA power and time of each study are summarized in Table 2. MWA power for malignant tumors was 30–70 W (except in one spinal tumors series where a mean power of 13.3 W was used). In terms of the ablation time, the mean pooled value for malignant tumors was 308.3 s. For OO, MWA power was 30–60 W with mean ablation time of 90–102 s.
A double-antenna approach was reported in 22/306 tumors (7.2%%; 95% CI 4.6–10.7) [19,20,21, 25], and overlapping ablations achieved with antenna repositioning were used by Wei et al [19] and Kastler et al [24] when tumor size exceeded 3.5 cm and 4.0 cm, respectively. On the other hand, Khan et al [23] reported an overlapping approach when tumors encompassed 2/3 of the vertebral body.
Additional thermoprotective measures were used very sporadically across studies. Thermocouples and clinical intraprocedural somatosensory lower limb monitoring was reported by Kastler et al [24]; sporadic hydrodissection by Prud’homme et al, Khan et al, and Rinzler et al [20, 22, 23]; and sporadic motor evoked potentials by Deib et al [25].
Osteoplasty was performed in 199/269 (74.0%; 95% CI 68.3–79.1) malignant tumors across the 5 studies reporting on this subject [19, 21, 23,24,25].
Technical success was 100% in 5 studies (Table 1) providing benchmark definitions and results of such outcome according to variable definitions and standards [19, 21, 23,24,25].
Complications
Complications were experienced in 16 patients (16/249 [6.4%]; 95% CI 3.7–10.2) across 4 studies [19, 20, 22, 23], which did not take into account intra- or peri-procedural pain that was reported in one study [19] and mentioned in another [22].
When subtracting the 6 asymptomatic cement leakages reported by Wei et al [19], the overall complication rate was 4.0% (10/249 patients; 95% CI 1.9–7.3). Nerve lesions, skin burns, and local infections were the most common events (Table 3).
Clinical outcomes
All the included studies [19,20,21,22,23,24,25] measured pain relief following MWA. Our analysis showed that I2 values for pain relief varied throughout intervals of all the studies (I2 = 88.0% at 1-month follow-up; I2 = 95.2% at the last recorded follow-up), suggesting vastly heterogeneous datasets. Therefore, the random-effect model was used to further describe the data, and despite heterogeneity, the p value was < 0.01, indicating statistical significance.
In studies reporting on malignant bone tumors [19, 21, 23,24,25] (Table 4; Fig. 2), the estimated pain reduction on the 0–10 NRS was 5.3/10 (95% CI 4.6–6.1) at 1 month. The same analysis at the last recorded follow-up (range 20–24 weeks in 4 studies and 48 weeks in one study) confirmed similar pain reduction (5.3/10; 95% CI 4.3–6.3).
For benign bone tumors, Prud’homme et al [22] used the NRS to assess pain relief at 1 month (NRS decrease of 6 points); in their study, the definition of clinical success (i.e., total pain relief and OO nidus necrosis on magnetic resonance imaging [MRI]) was provided and achieved in 12/13 (92.3%) patients. On the other hand, Rinzler et al [20] assessed 1 month pain relief in patients with OO as the percentage of subjects reporting complete pain relief without need for medications, and found it in 24/24 (100%) patients.
Khan et al and Deib et al [23, 25] also reported changes in the Oswestry Disability Index (ODI) scale, respectively, for 44/69 (63.8%; 95% CI 51.3–75.0) and 52/65 (80.0%; 95% CI 68.2–88.9) patients. In Khan et al [23], the mean ODI changed from 48.5 at baseline to 25.8 at 20–24 weeks follow-up, which was similar to Deib et al [25] (42.4 at baseline vs 25.3 at 20–24 weeks follow-up). Pusceddu et al [21] qualitatively evaluated patients’ walking ability at different intervals and noted an improvement in 100% (35/35 survivors), 98.0% (34/35 survivors), and 100% (25/25 survivors) patients at 1-, 6- and 12-month follow-up, respectively.
Local tumor control in malignant bone tumors was reported in only two studies [23, 25], accounting for 87/249 patients (34.9%; 95% CI 29.0–41.2; 65 patients from Deib et al and 22 oligometastatic patients from Khan et al). Khan et al [23] assessed complete tumor destruction with different imaging modalities (CT, MRI, positron emission tomography [PET-CT]), and Deib et al used PET-CT. Overall, at 20–24 weeks follow-up, 64/87 (73.6%; 95% CI 63.0–82.4) patients reported stable disease, and 23/87 (26.4%; 95% CI 17.6–37.0) disease progression.
Discussion
The quality of the studies included in the present analysis was predominantly low and sporadically moderate, mainly due to absence of a prospective study design (6/7 studies), unbiased assessment of the study endpoints (7/7 studies), and prospective calculation of the sample size (7/7 studies). Moreover, if one looks at the included population, there were only two studies (with a very limited number of subjects) applying MWA for the treatment of benign bone tumors [20, 22], and two studies on malignant bone tumors originating from one single institution were at the origin of more than 60% of the total number of malignant tumors included in the present study [23, 25]. Consequently, these data substantially highlight the very limited experience available in literature with bone tumors MWA.
Nevertheless, with the majority of studies clearly investigating pain relief, MWA did not fail to prove its effectiveness at follow-up intervals that largely varied across the malignant (4–6 months) and benign bone tumor (1 month) studies. This is concordant with series analyzing the same outcome following bone tumor RFA or CA. In particular, Goetz et al [9] reported a significant reduction (from 7.9/10 at the baseline to 1.4/10 at 24 weeks) of the mean worst pain after RFA of painful bone metastases. Rosenthal et al [29] reported clinical success of 91% after RFA of OO, and in a recently published prospective study including 21 OO treated with RFA, the mean pain score dropped from 7.1/10 at baseline to 0.2/10 at 3-month follow-up [7]. Similarly, Callstrom et al [11] reported a mean score for worst pain in the 24-h period dropping from 7.1/10 at baseline to 1.4/10 at 24 weeks following CA of painful bone metastases. In the end, Santiago et al noted that pain dropped from median 8/10 to 0/10 at 6–40 months after CA of 21 OO [12]. Given the concordance of results achieved by treating painful bone tumors with MWA, RFA, and CA, one may speculate that pain palliation primarily relies on thermal tumor destruction regardless of the type of applied energy [30].
Other clinical outcomes such as patient disability and local tumor control were only sporadically reported in MWA studies and with variable criteria, and although results were encouraging, a definitive appraisal and direct comparison with RFA and CA literature is restricted due to paucity/inhomogeneity of data.
In terms of ablation protocols, there was a large variability of practice, even when similar tumors were treated. For instance, Khan et al [23] used a very low power (mean 13 W) with a mean ablation time of 286 s for spinal tumors, which roughly corresponds to an amount of delivered energy of 3.9 KJ. On the other side, Kastler et al [24] applied a higher power (mean 60 W) with a mean 264 s, which approximately correspond to 15.8 KJ, in the same clinical setting. Similarly with OO, Prud’homme et al [22] used a single antenna at 50–60 W for mean 90 s, which approximately corresponds to 4.5–5.4 KJ, while Rinzler et al [20] applied at least 3 ablation cycles with 1–2 antennas; in their experience, they used 30 W (target temperature 90 °C with 30 s of cooling between heating cycles) for mean ablation time of 102 s, which approximately corresponds at least to 3 KJ when a single antenna was applied. These amounts of energies seem somehow excessive for OO ablation. In fact, we know from experiences on OO undergoing laser ablation that an effective and complete destruction of a nidus sized < 10 mm is achieved with no more than 1.2 KJ [31], which stresses the idea that practices with bone tumors MWA are still not homogenous and standardized.
Moreover, it was somehow surprising that despite the relatively low experience available with MWA, and the high propensity of bone tumor ablation to induce neuro-cutaneous damages [26, 27], protective measures were applied so sporadically, which is not the case in large RFA and CA series applying thermal monitoring and hydro-/carbo-displacement in at least 50% of treated tumors [26, 27]. This may justify the reason why most of the complications reported after MWA effectively involved these anatomical structures. Coming more into the details of safety of bone tumor MWA, with an overall 4.0% rate of clinically significant complications, MWA of bone tumors may be deemed safe. And when interrogating two recently published large series investigating RFA and CA safety in the setting of bone tumors [26, 27], one may speculate that MWA may be even safer than these two more established ablation modalities, respectively reporting an overall complication rate of 30.0% (2.3% major; 27.7% minor with postoperative pain accounting for 18.0% of all complications) and 9.1% (2.5% major; 6.6% minor). However, such comparison has some caveats including the calculation of complications per tumor in RFA/CA literature [26, 27], rather than per patient as done in MWA studies and, consequently, in our analysis. Moreover, in RFA series [27], a high number of treated tumors (18.0%) reported immediate postoperative pain, which was the main factor accounting for the overall high rate for all complications (30.0%). Such event has never been considered as a complication in any of the MWA studies, and only Wei et al [19] reported that some patients in their series experienced moderate/severe pain, which was considered an “adverse event” and did not account for complications. Consequently, the impact of post-procedural pain, which may have practical implications including prolonged hospital stay [32], has been probably largely underestimated in MWA series. Moreover, Prud’homme et al [22] reported that pain severely interfered with the normal course of MWA performed under local anesthesia, thus requiring an amendment to their prospective study protocol (i.e., switching from local to epidural/general anesthesia) after the first 5 patients.
Concerning major complications, with only one secondary fracture reported, it seems that MWA performs better than RFA and CA, for which secondary fractures represent the most common major complication occurring in 1.8% and 1.2% of treated bone tumors at mean 127.5 and 71.5 days, respectively [26, 27]. There is no clear rationale to explain why bone heating with MWA would cause less fragility to the bone compared to RFA. Possible rationalizations include (a) the high rate of osteoplasty (73.9%) performed after MWA of malignant tumors included in the present analysis; (b) the relatively short follow-up intervals reported in the included studies (especially those dealing with OO), which may have potentially resulted in an underestimation of such event in such population; (c) the relatively non-aggressive MWA applied in many index tumors included in the present study such as malignant tumors mainly undergoing treatments for pain relief, thus not compellingly needing large necrosis (predisposing to secondary fractures) to achieve the desired clinical outcome. In fact, MWA protocols were probably adapted to significantly reduce ablation power/time such as in Khan et al [23], who have ablated spinal metastases with a mean power of 13 W, and Kastler et al [24] have applied multiple very short (30–90 s) ablation cycles to treat painful spinal metastases. Moreover, several studies, and notably those with the largest sample for malignant tumors (i.e., Deib et al and Khan et al accounting for 134/212 [63.2%] patients with 179/269 [66.5%] malignant tumors) and OO (i.e. ,Rinzler et al accounting for 24/37 [68.9%] patients with 24/37 [68.9%] OO) [20, 23, 25], clearly avoided treatment of tumors being close to nerve roots or joints that are those clearly being prone to post-treatment complications.
There are some limitations to our study. First of all, the results we present were mostly derived from low-/moderate-quality single-arm retrospective studies without comparative groups. Secondly, primary benign/malignant and metastatic tumors were included; nevertheless, we have tried to present main results separately for these two entities. Thirdly, it was not possible from our analysis to assess on a large-scale clinical outcome other than pain relief, and to validate the safety profile of MWA. This latter aspect mainly occurred due to the relatively short follow-up reported in MWA series (especially those reporting on OO), the large variability of MWA protocols which were probably somehow “braked” at least in malignant cases, and treatment avoidance of high-risk tumors in many large series. Moreover, to allow extraction of homogenous data being comparable across studies, we have reported complications per patient rather than per tumor, which has prevented direct comparisons with other recently published series investigating the safety of bone tumor ablation achieved with more established techniques such as RFA and CA [26, 27]. In addition, reporting complications per patient may have somehow impacted the “quality” (minor/major complications) of reported complications, which mainly depends on the local anatomy (e.g., an ablation of a spinal tumor abutting the posterior vertebral wall is theoretically more challenging and more prone to complications compared to the ablation of a tumor in the anterior aspect of the iliac bone), and the real complication rate since one patient may receive ablation in multiple bone sites during the same interventional session. Lastly, data were collected in consensus without any assessment of inter-observer variability.
In conclusion, MWA is effective in achieving short- (1 month) and mid-term (4–6 months) pain relief after treating painful OO and malignant bone tumors. Nevertheless, clinical experience achieved so far is still limited (e.g., more than 60% included malignant tumors came from one single institution). Therefore, it seems crucial to achieve standardization of the ablation protocol through pre-clinical experiences, and to design prospective studies useful to investigate clinical outcomes other than pain relief (i.e., local tumor control and safety), as well as to compare MWA with more established techniques such as RFA and CA.
Abbreviations
- CA:
-
Cryoablation
- CI:
-
Confidence intervals
- CT:
-
Computed tomography
- MINORS:
-
Methodological Index for Non-Randomized Studies
- MRI:
-
Magnetic resonance imaging
- MWA:
-
Microwave ablation
- NRS:
-
Numerical rating scale
- ODI:
-
Oswestry Disability Index
- OO:
-
Osteoid osteomas
- PET-CT:
-
Positron emission tomography computed tomography
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RFA:
-
Radiofrequency ablation
References
Coleman RE (2001) Metastatic bone disease: clinical features, pathophysiology and treatment strategies. Cancer Treat Rev 27(3):165–176
Macedo F, Ladeira K, Pinho F et al (2017) Bone metastases: an overview. Oncol Rev 11(1):321
Cazzato RL, Arrigoni F, Boatta E et al (2019) Percutaneous management of bone metastases: state of the art, interventional strategies and joint position statement of the Italian College of MSK Radiology (ICoMSKR) and the Italian College of Interventional Radiology (ICIR). Radiol Med 124(1):34–49
Gangi A, Tsoumakidou G, Buy X, Quoix E (2010) Quality improvement guidelines for bone tumour management. Cardiovasc Intervent Radiol 33(4):706–713
Koch G, Cazzato RL, Gilkison A, Caudrelier J, Garnon J, Gangi A (2018) Percutaneous treatments of benign bone tumors. Semin Intervent Radiol 35(4):324–332
Rehnitz C, Sprengel SD, Lehner B et al (2012) CT-guided radiofrequency ablation of osteoid osteoma and osteoblastoma: clinical success and long-term follow up in 77 patients. Eur J Radiol 81(11):3426–3434
Miyazaki M, Arai Y, Myoui A et al (2016) Phase I/II multi-institutional study of percutaneous radiofrequency ablation for painful osteoid osteoma (JIVROSG-0704). Cardiovasc Intervent Radiol 39(10):1464–1470
Tanigawa N, Arai Y, Yamakado K et al (2018) Phase I/II study of radiofrequency ablation for painful bone metastases: Japan interventional radiology in oncology study group 0208. Cardiovasc Intervent Radiol 41(7):1043–1048
Goetz MP, Callstrom MR, Charboneau JW et al (2004) Percutaneous image-guided radiofrequency ablation of painful metastases involving bone: a multicenter study. J Clin Oncol 22(2):300–306
Cazzato RL, Garnon J, Caudrelier J, Rao PP, Koch G, Gangi A (2018) Percutaneous radiofrequency ablation of painful spinal metastasis: a systematic literature assessment of analgesia and safety. Int J Hyperthermia 34(8):1–10
Callstrom MR, Dupuy DE, Solomon SB et al (2013) Percutaneous image-guided cryoablation of painful metastases involving bone: multicenter trial. Cancer. 119(5):1033–1041
Santiago E, Pauly V, Brun G, Guenoun D, Champsaur P, Le Corroller T (2018) Percutaneous cryoablation for the treatment of osteoid osteoma in the adult population. Eur Radiol 28(6):2336–2344
Whitmore MJ, Hawkins CM, Prologo JD et al (2016) Cryoablation of osteoid osteoma in the pediatric and adolescent population. J Vasc Interv Radiol 27(2):232–237 quiz 238
Brace CL (2009) Microwave ablation technology: what every user should know. Curr Probl Diagn Radiol 38(2):61–67
Cazzato RL, De Marini P, Leclerc L et al (2020) Large nearly spherical ablation zones are achieved with simultaneous multi-antenna microwave ablation applied to treat liver tumours. Eur Radiol 30(2):971–975
Pusceddu C, Melis L, Ballicu N et al (2018) Percutaneous microwave ablation under CT guidance for hepatocellular carcinoma: a single institutional experience. J Gastrointest Cancer 49(3):295–301
Ma S, Ding M, Li J et al (2017) Ultrasound-guided percutaneous microwave ablation for hepatocellular carcinoma: clinical outcomes and prognostic factors. J Cancer Res Clin Oncol 43(1):131–142
Alexander ES, Wolf FJ, Machan JT et al (2015) Microwave ablation of focal hepatic malignancies regardless of size: a 9-year retrospective study of 64 patients. Eur J Radiol 84(6):1083–1090
Wei Z, Zhang K, Ye X et al (2015) Computed tomography-guided percutaneous microwave ablation combined with osteoplasty for palliative treatment of painful extraspinal bone metastases from lung cancer. Skeletal Radiol 44(10):1485–1490
Rinzler ES, Shivaram GM et al (2019) Microwave ablation of osteoid osteoma: initial experience and efficacy. Pediatr Radiol 49(4):566–570
Pusceddu C, Sotgia B, Fele RM, Ballicu N, Melis L (2016) Combined microwave ablation and cementoplasty in patients with painful bone metastases at high risk of fracture. Cardiovasc Intervent Radiol 39(1):74–80
Prud’homme C, Nueffer JP, Runge M, Dubut J, Kastler B, Aubry S (2017) Prospective pilot study of CT-guided microwave ablation in the treatment of osteoid osteomas. Skeletal Radiol 46(3):315–323
Khan MA, Deib G, Deldar B, Patel AM, Barr JS (2018) Efficacy and safety of percutaneous microwave ablation and cementoplasty in the treatment of painful spinal metastases and myeloma. AJNR Am J Neuroradiol 39(7):1376–1383
Kastler A, Alnassan H, Aubry S, Kastler B (2014) Microwave thermal ablation of spinal metastatic bone tumors. J Vasc Interv Radiol 25(9):1470–1475
Deib G, Deldar B, Hui F, Barr JS, Khan MA (2019) Percutaneous microwave ablation and cementoplasty: clinical utility in the treatment of painful extraspinal osseous metastatic disease and myeloma. AJR Am J Roentgenol. https://doi.org/10.2214/AJR.18.20386
Auloge P, Cazzato RL, Rousseau C et al (2019) Complications of percutaneous bone tumor cryoablation: a 10-year experience. Radiology. 291(2):521–528
Cazzato RL, Palussière J, Auloge P et al (2020) Complications following percutaneous image-guided radiofrequency ablation of bone tumors: a 10-year dual-center experience. Radiology. 296(1):227–235
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73(9):712–716
Rosenthal DI, Hornicek FJ, Torriani M, Gebhardt MC, Mankin HJ (2003) Osteoid osteoma: percutaneous treatment with radiofrequency energy. Radiology. 229(1):171–175
Gennaro N, Sconfienza LM, Ambrogi F, Boveri S, Lanza E (2019) Thermal ablation to relieve pain from metastatic bone disease: a systematic review. Skeletal Radiol 48(8):1161–1169
Tsoumakidou G, Thénint MA, Garnon J, Buy X, Steib JP, Gangi A (2016) Percutaneous image-guided laser photocoagulation of spinal osteoid osteoma: a single-institution series. Radiology. 278(3):936–943
Thacker PG, Callstrom MR, Curry TB et al (2011) Palliation of painful metastatic disease involving bone with imaging-guided treatment: comparison of patients’ immediate response to radiofrequency ablation and cryoablation. AJR Am J Roentgenol 197(2):510–515
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Pr Afshin GANGI.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was not required because this study is a systematic review of literature.
Ethical approval
Institutional Review Board approval was not required because this study is a systematic review of literature.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in the seven included studies used for the final analysis.
Methodology
• Systematic review of the literature
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cazzato, R.L., de Rubeis, G., de Marini, P. et al. Percutaneous microwave ablation of bone tumors: a systematic review. Eur Radiol 31, 3530–3541 (2021). https://doi.org/10.1007/s00330-020-07382-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07382-8