Abstract
Objectives
To evaluate the incidence and diagnostic performance of reverse attenuation gradient (RAG) sign in patients with coronary stent occlusion.
Methods
We retrospectively included patients with suspected restenosis who underwent both coronary computed tomography angiography (CCTA) and invasive coronary angiography (ICA) within 2 weeks. Stent occlusion at CCTA was defined as (1) complete contrast filling defect of large calibre stents (at least 3 mm), or (2) presence of RAG sign in patients with small calibre stents (less than 3 mm) or (3) presence of RAG sign in patients with non-diagnostic image quality of stents. The diagnostic performance of RAG sign was further assessed by comparison to ICA results.
Results
A total of 162 patients with 231 implanted stents were included. ICA confirmed stent occlusion in 59 patients (99 stents). RAG sign was present in 59.3 % (35/59) of all stent occlusions. As shown by patient-based analysis, the sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of our diagnostic criteria for detection of stent occlusion were 79.7 % (47/59), 100 % (103/103), 100 % (47/47) and 89.6 % (103/115) respectively. Superior diagnostic performance was confirmed by receiver operating characteristic (ROC) analysis with an area under the curve of 0.898.
Conclusions
RAG sign observed at CCTA in patients with coronary stenting represents reverse collateral flow distal to stents and is highly specific to indicate stent occlusion.
Key Points
• RAG sign in patients with previous stents represents retrograde collateral flow.
• RAG sign in patients with previous stents indicates stent occlusion.
• RAG sign improves detection of stent occlusion in small calibre stents.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary artery stenting is currently the predominant strategy of non-surgical revascularization in patients with obstructive coronary artery disease [1, 2]. Even with the wide application of drug-eluting stent (DES), in-stent restenosis (ISR) and stent occlusion remain the major complications of this procedure [3, 4].
Although coronary computed tomography angiography (CCTA) has a high sensitivity and specificity for diagnosis of ISR [5–7], the diagnostic performance is compromised in patients with small calibre stents [8]. Reverse attenuation gradient (RAG) sign is a recently revealed sign observed at CCTA in patients with chronic total occlusion and indicates retrograde collateral flow distal to the occlusive site [9]. In brief, RAG sign is defined as a reverse intraluminal opacification gradient of vessels distal to the occlusive lesions. Unlike the usual gradient pattern in normal coronary arteries, with a higher attenuation in proximal segment and gradually decreased attenuation along the vessel [10], the reverse gradient shows higher opacification in more distal sites. We hypothesized that RAG sign could also been seen in patients with stent occlusion and represent reverse filling from collaterals. Therefore, we aimed to evaluate the incidence and diagnostic performance of RAG sign in patients with stent occlusion.
Methods
Patient population
Institutional review board approval was obtained for this retrospective study, and informed consent was waived. We searched our database from January 2010 to December 2013 to identify patients with clinically suspected ISR who underwent both CCTA and invasive coronary angiography (ICA). In order to test the diagnostic performance of RAG sign in patients with small calibre stents, we retrospectively included all cases with various stent diameters. The inclusion criterion was an interval between CCTA and ICA of less than 2 weeks. The exclusion criterion was an interval between CCTA and ICA longer than 2 weeks.
Imaging protocol of CCTA
A 128-slice multidetector CT (Definition AS, Siemens Medical Solutions, Forchheim, Germany) was employed for imaging. Beta blocker (25–75 mg) was administrated orally 1 h prior to the examination in patients with a heart rate above 65 bpm. Nitroglycerin was given sublingually in all patients. A bolus of contrast medium (Iopamidol, 370 mg iodine/ml, Schering AG, Berlin, German) was injected into the antecubital vein at a rate of 4.5–5 ml/s, followed by a 20- to 40-ml saline flush by using a dual-barrel power injector (Tyco, Cincinnati, USA). The amount of contrast medium was determined according to the patient’s body weight and imaging time. A test bolus was first injected and the region of interest was placed within the ascending aorta to determine the required delay time, which was defined as 4 s plus the peak time of the ascending aorta. Retrospective ECG-gated CTA was performed in patients with a final heart rate of at least 70 bpm, with collimation, 128 × 0.6 mm; reconstructed slice thickness, 0.6 mm; reconstructed slice interval, 0.5 mm; rotation time, 300 ms; pitch and current were ECG modified; the effective current was set as 200 mA (ECG-dependent dose modulation technique was applied, full dose during the R–R interval of 40–70 %) and tube voltage, 120 kVp. Prospective ECG-triggered CTA was performed in patients with a final heart rate of less than 70 bpm, with the centre of the triggering window set at 70 % of the R–R interval. The rest of the parameters of the prospective acquisition were the same as for the retrospective acquisition.
Image reconstruction and analysis
For better delineation of both vessel wall and stent lumen [8], two sets of axial images were reconstructed with different kernels: smooth kernel (B26f smooth ASA) and sharp kernel (B46f sharp heartview ASA) with a slice thickness of 0.625 mm. Data was transferred to an offline workstation (SyngoTM, Siemens) for further analysis. Curved planar reformation (CPR) and short axis view of the stents with sharp kernel reconstruction were used for evaluation of ISR.
Image quality of stent was assessed by using a 3-point semi-quantitative scale: 3, excellent (absence of artefact); 2, acceptable (presence of less artefact, but still diagnostic); 1, poor (presence of severe artefact, non-diagnostic). Lesions with non-diagnostic image quality were considered as presence of ISR for further analysis.
Attenuation gradient distal to the stents was measured as follows: cross-sectional images perpendicular to the vessel centreline were reconstructed for each vessel segment distal to an occlusive lesion. The region of interest (ROI) was manually drawn to include the entire vessel lumen on cross-sectional images with exclusion of wall calcification using the unenhanced images for calcium scoring for comparison. The luminal radiological attenuation (Hounsfield units, HU) was measured at 10-mm intervals, from the distal end of the stents to the level of the artery where the lumen area fell below 2 mm2. Attenuation gradient was determined from the change in HU per 10-mm length of coronary artery and defined as the linear regression coefficient between intraluminal attenuation (in HU) and length from the distal end of the stents (in millimetres), as previously introduced by Choi et al. [10]. The RAG sign was considered present when attenuation gradient was greater than 0. Stent occlusion was defined as (1) complete contrast filling defect at CCTA in patients with large calibre stents (at least 3 mm), or (2) presence of RAG sign in patients with small calibre stents (less than 3 mm) or (3) presence of RAG sign in patients with non-diagnostic image quality of stents. Stents with visible contrast filling or absence of RAG sign were considered as non-occluded.
Binary ISR is considered as an in-stent neointimal proliferation with a stenosis diameter of at least 50 %. The angiographic patterns of binary ISR were further classified by CCTA into four types according to the Mehran classification [11].
Total lesion length was measured on CPR images and defined as the length from the proximal to distal shoulder of the in-stent neointimal proliferation. ISR involving two or more overlapping stents was considered as one lesion.
All images were evaluated independently by two radiologists who were blinded to the number, location, diameter, and type of stents and to the clinical history of the patients. Disagreements between the two readers for any image set were resolved by consensus, and the consensus findings were used in all assessments of diagnostic performance.
ICA procedure and analysis
The ICA was performed with standard techniques, and at least two different views were obtained for each main vessel. All segments were evaluated by two skilled observers who were blinded to the results of CCTA. Disagreements between the two readers were resolved by consensus. The angiographic patterns of ISR were classified into four types according to Mehran classification and stent occlusion was defined as absence of antegrade contrast filling with a thrombolysis in myocardial infarction (TIMI) flow grade of 0 [11].
Statistical analysis
Statistical analysis was performed using commercially available statistical software (SSPS, V13.0, SPSS Inc., Chicago, USA). The diagnostic accuracy was evaluated by sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV). Interobserver agreement was expressed in Cohen’s kappa value (κ) for categorical variables. We used a Fisher exact test to compare proportions. Receiver operating characteristic (ROC) curve analysis was performed to test the diagnostic accuracy of CCTA for the detection of stent occlusion.
Results
Clinical characteristics
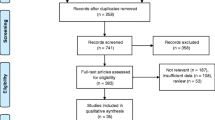
A total of 197 patients with prior percutaneous coronary intervention (PCI) and follow-up CCTA/ICA were initially included by a retrospective search. Of these, 35 patients were excluded owing to the interval between CCTA and ICA being longer than 2 weeks. Therefore, 162 patients (114 males and 48 females; mean age, 67.4 ± 11.5; range, 36–85 years) with 231 implanted stents were finally included in our study. The radiation dose of CCTA was 6.4 ± 1.5 mSv (range, 3.8–10.1 mSv) in the total population, 7.2 ± 1 mSv (range, 4.9–10.1 mSv, 113 patients) for the retrospective acquisition group and 4.5 ± 0.3 mSv (range, 3.8–4.9 mSv, 49 patients) for the prospective acquisition group. ICA was performed in all patients with an interval of 5 ± 3.1 days (range, 1–14 days). The radiation dose of ICA was 4.7 ± 1.1 mSv (range, 2.5–7.1 mSv). Detailed demographic data and stent characterization are shown in Tables 1 and 2.
CCTA and ICA characteristics
The image quality of CCTA was rated as excellent (score 3) in 91 patients and acceptable (score 2) in 57 patients. Fourteen patients had poor image quality (score 1) due to rhythm irregularity-related artefact (5 cases) and heart rate-related artefact (9 cases). Among all 231 implanted stents, ICA revealed the presence of total occlusion in 99 stents (59 lesions), non-occlusive ISR in 105 stents (96 lesions) and patency in 27 stents (25 lesions). Comparison to ICA, CCTA showed great discrepancy for detection of ISR in large (at least 3 mm) and small (less than 3 mm) calibre stents (Table 3). Reverse collateral flow was observed at ICA in all but 8 stent occlusions (86.4 %, 51/59). In terms of the calibre of 99 occluded stents, 57 stents (33 lesions) had a nominal diameter of at least 3 mm whereas another 42 stents (26 lesions) had a nominal diameter of less than 3 mm. Compared to ICA findings, most of the large calibre stents were assessable at CCTA and complete contrast filling defect was clearly detected. However, a large proportion of small calibre stents were considered as non-assessable at CCTA and failed to exclude stent occlusions in those patients when the traditional diagnosing criterion (detection of complete contrast filling defect) was applied (Table 4).
Incidence and diagnostic performance of RAG sign in patients with stent occlusion
According to CCTA findings, distal filling of vessels with occluded stents was evident in 89.8 % cases (53/59). Excellent interobserver agreement for determining the presence of RAG sign was observed (κ = 0.93, p < 0.001). Regardless of stent diameters, RAG sign was present similarly in both large calibre group (57.6 %, 19/33) and small calibre group (61.5 %, 16/26), with an overall incidence rate of 59.3 % (35/59) as shown by patient-based analysis. Compared to 51 cases with ICA-revealed reverse collaterals, RAG sign was observed in 64.7 % of patients (33/51) (Figs. 1, 2), with a mean attenuation gradient (of vessels distal to the stents) of 10 ± 4.5 HU/10 mm (range, 2–18 HU/10 mm). All vessels with presence of RAG sign were consistent with retrograde collateral flow, as confirmed by ICA findings. Additionally, RAG sign was present in two cases without ICA-confirmed retrograde distal filling.
Stent occlusion with the presence of RAG sign observed at CCTA. a CPR image of LAD showed severe strut artefact of proximal and middle LAD stents, which led to a non-assessable stent image. The attenuation gradient of distal LAD vessel was revealed to have the presence of RAG sign, indicating retrograde filling pattern. b ICA of left coronary artery confirmed the diagnosis of total stent occlusion (black arrow). c ICA of right coronary artery showed reverse collateral flow (black arrowhead) from PDA to LAD segment which was distal to the stent (black arrow). d Attenuation gradient of the vessel distal to the stents in this patient was 8.35 HU/10 mm, indicating the presence of RAG sign. CCTA coronary computed tomography angiography, CPR curved planar reformation, ICA invasive coronary angiography, LAD left anterior descending, PDA posterior descending artery, RAG reverse attenuation gradient
Stent occlusion with the presence of RAG sign observed at CCTA. a CPR image of LAD showed severe strut artefact of proximal LAD stents, which led to a non-assessable stent image. The attenuation gradient of middle and distal LAD vessel was revealed to have the presence of RAG sign, indicating retrograde filling pattern. b ICA of left coronary artery confirmed the diagnosis of total stent occlusion (black arrow). c ICA of right coronary artery showed reverse collateral flow (black arrowhead) from septal branches to LAD segment which was distal to the stent (black arrow). d Attenuation gradient of the vessel distal to the stents in this patient was 5.63 HU/10 mm, indicating the presence of RAG sign. CCTA coronary computed tomography angiography, CPR curved planar reformation, ICA invasive coronary angiography, LAD left anterior descending, RAG reverse attenuation gradient
CCTA was able to correctly identify stent occlusions in only 54.2 % (32/59) of total occluded lesions when detection of complete contrast filling defect was used as the sole diagnosing criterion. Since distal vessel opacification was usually present in case of stent occlusion, correct diagnosis in those non-assessable stents was not possible owing to severe strut artefact (45.8 %, 27/59), especially in the small calibre group. Notably, an additional 15 lesions were diagnosed as stent occlusions when taking RAG sign into consideration. Superior diagnostic performance was confirmed by ROC analysis if a combination of the traditional diagnosing criterion and RAG sign was employed (Fig. 3). As shown by patient-based analysis, the sensitivity, specificity, PPV and NPV for diagnosis of stent occlusion were 79.7 % (47/59), 100 % (103/103), 100 % (47/47) and 89.6 % (103/115) respectively.
Discussion
This study revealed two main findings: (1) RAG sign observed at CCTA in patients with coronary stenting represents reverse collateral flow distal to the stents; (2) RAG sign is a highly specific sign indicating stent occlusion.
The use of DES has remarkably reduced the rates of restenosis and target lesion revascularization (TLR) compared with bare-metal stents (BMS) [12]. However, a low rate of ISR after DES still exists, and its prevalence is not negligible because the population treated with DES is large. Although the majority leads to recurrent symptoms, some cases of ISR are clinically silent and late myocardial infarction (MI) can be caused by highly stenotic ISR or stent occlusion [13–15]. Early detection of stent occlusion is of clinical significance to prevent secondary MI and therefore improve long-term prognosis. However, small calibre stents (diameter less than 3 mm) dramatically reduce the visibility of stent lumen and subsequently lead to a large proportion of unassessable stents [8]. Thus, stent occlusion could potentially be overlooked at CCTA in patients with small calibre stents when reverse collateral filling is well developed.
Stent occlusion is defined as the obstruction of the stented coronary artery with no luminal continuity and interruption of antegrade blood flow [11]. Initial studies of normal coronary arteries imaged by CCTA showed a small but consistent decrease in contrast opacification from the proximal to distal coronary artery [10, 16]. However, since the collateral flow fills the distal lumen reversely in patients with stent occlusion, it is conceivable that the attenuation gradient of the downstream vessel is in the opposite sense. Similar to our previous report [9], all the cases showing RAG sign in this study were proved to be correlated with stent occlusion and represent reverse collateral flow. In terms of clinical significance, this highly specific sign is especially helpful for the diagnosis of stent occlusion in patients with small calibre stents or non-diagnostic stent image quality caused by various artefacts. As the RAG sign is able to reveal the flow direction distal to an occlusive lesion, it can help to differentiate stent occlusion from non-occlusive stents, which indeed have antegrade blood flow.
Other than its high specificity and positive predictive value, RAG was found to have non-comparable sensitivity and NPV as RAG sign was absent in several cases in which reverse collaterals were evident at ICA. The attenuation gradient pattern of those false negative lesions, as revealed by our study, was similar to that expected in non-occluded coronary arteries. This phenomenon could be caused by the relative late phase of acquisition, in which all segments distal to the occlusion have been filled by retrograde flow. Thus, the absence of RAG sign at CCTA could not exclude the diagnosis of stent occlusion. In addition, non-occluded ISR has the antegrade flow and does not show the presence of RAG sign. Therefore, RAG sign is not helpful for the diagnosis of non-occluded ISR types.
The major limitation of this study is the use of 128-slice multidetector computed tomography (MDCT), in which simultaneous acquisition of the whole heart is not possible. The measured gradient will be highly dependent on the timing of the examination relative to contrast injection. Thus the RAG will be less apparent if the examination is performed late in the contrast injection. However, RAG can be more frequently expected in patients with stent occlusion if wider detector MDCT or DSCT systems are employed, as the difference of filling time between proximal and distal collaterals will be more markedly revealed in a single-beat whole heart image.
In conclusion, RAG sign observed at CCTA in patients with previous coronary stenting represents the reverse collateral flow distal to stents and indicates stent occlusion.
Abbreviations
- CCTA:
-
Coronary computed tomography angiography
- CPR:
-
Curved planar reformation
- DES:
-
Drug-eluting stent
- ICA:
-
Invasive coronary angiography
- ISR:
-
In-stent restenosis
- IVUS:
-
Intravascular ultrasound
- PCI:
-
Percutaneous coronary intervention
- TIMI:
-
Thrombolysis in myocardial infarction
- TLR:
-
Target-lesion revascularization
References
Sousa JE, Serruys PW, Costa MA (2003) New frontiers in cardiology: drug-eluting stents: Part I. Circulation 107:2274–2279
Sousa JE, Serruys PW, Costa MA (2003) New frontiers in cardiology: drug-eluting stents: Part II. Circulation 107:2283–2289
Moses JW, Leon MB, Popma JJ, SIRIUS Investigators et al (2003) Sirolimus-eluting stents versus standard stents in patients with stenosis in a native coronary artery. N Engl J Med 349:1315–1323
Stone GW, Ellis SG, Cox DA, TAXUS-IV Investigators et al (2004) A polymer-based, paclitaxel-eluting stent in patients with coronary artery disease. N Engl J Med 350:221–231
Pan J, Lu Z, Zhang J et al (2013) Angiographic patterns of in-stent restenosis classified by computed tomography in patients with drug-eluting stents: correlation with invasive coronary angiography. Eur Radiol 23:101–107
Cademartiri F, Schuijf JD, Pugliese F et al (2007) Usefulness of 64-slice multislice computed tomography coronary angiography to assess in-stent restenosis. J Am Coll Cardiol 49:2204–2210
Oncel D, Oncel G, Karaca M (2007) Coronary stent patency and in-stent restenosis: determination with 64-section multidetector CT coronary angiography-initial experience. Radiology 242:403–408
Zhang J, Li M, Lu Z et al (2012) In vivo evaluation of stent patency by 64-slice multidetector CT coronary angiography: shall we do it or not? Int J Cardiovasc Imaging 28:651–658
Li M, Zhang J, Pan J et al (2013) Obstructive coronary artery disease: reverse attenuation gradient sign at CT indicates distal retrograde flow–a useful sign for differentiating chronic total occlusion from subtotal occlusion. Radiology 266:766–772
Choi JH, Min JK, Labounty TM et al (2011) Intracoronary transluminal attenuation gradient in coronary CT angiography for determining coronary artery stenosis. JACC Cardiovasc Imaging 4:1149–1157
Mehran R, Dangas G, Abizaid AS et al (1999) Angiographic patterns of in-stent restenosis: classification and implications for long-term outcome. Circulation 100:1872–1878
Stettler C, Wandel S, Allemann S et al (2007) Outcomes associated with drug-eluting and bare-metal stents: a collaborative network meta-analysis. Lancet 370:937–948
Rathore S, Kinoshita Y, Terashima M et al (2010) A comparison of clinical presentations, angiographic patterns and outcomes of in-stent restenosis between bare metal stents and drug eluting stents. EuroIntervention 5:841–846
Chen MS, John JM, Chew DP et al (2006) Bare metal stent restenosis is not a benign clinical entity. Am Heart J 151:1260–1264
Bossi I, Klersy C, Black AJ et al (2000) In-stent restenosis: long-term outcome and predictors of subsequent target lesion revascularization after repeat balloon angioplasty. J Am Coll Cardiol 35:1569–1576
Steigner ML, Mitsouras D, Whitmore AG et al (2010) Iodinated contrast opacification gradients in normal coronary arteries imaged with prospectively ECG-gated single heart beat 320-detector row computed tomography. Circ Cardiovasc Imaging 3:179–186
Acknowledgements
The scientific guarantor of this publication is Dr. Jiayin Zhang. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. This study has received funding by National Natural Science Foundation of China (Grant No.: 81301219) and Shanghai Committee of Science and Technology, China (Grant No.: 13ZR1431500). No complex statistical methods were necessary for this paper. Institutional review board approval was obtained. Written informed consent was waived by the institutional review board. Methodology: retrospective, diagnostic or prognostic study, performed at one institution.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Li, M., Zhang, J., Zhang, Q. et al. Coronary stent occlusion: reverse attenuation gradient sign observed at computed tomography angiography improves diagnostic performance. Eur Radiol 25, 568–574 (2015). https://doi.org/10.1007/s00330-014-3429-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3429-x