Abstract
Besides the assessment of carotid artery stenosis, evaluation of the vascular anatomy and lesions within both the extra- and intracranial arteries is crucial for proper clinical evaluation, treatment choice and planning. The purpose of our study was to evaluate the potential of dual-source CTA and 3T-MRA. In 16 symptomatic CAS patients, contrast-enhanced DSCT and 3T-MRA examinations were performed. For DSCT a dual-energy protocol with a 64 × 0.6-mm collimation was applied. In 3T-MRA intracranial high-resolution unenhanced TOF and extracranial contrast-enhanced MRA were performed. All examinations were analyzed for relevant morphologic and pathologic features or anomalies, and a total of 624 vessel segments were scored. All examinations were of diagnostic image quality with good to excellent vessel visibility. Almost all intracranial arteries were significantly better visualized by MRA compared to CTA (five of six vessels, p < 0.05). DSCT however allowed for further morphological carotid stenosis description, especially with respect to calcification. Although MRA proved to be superior in visualization of smaller intracranial arteries, all pre-interventionally relevant information could be perceived from DSCT. DSCT and MRA may both be regarded as a reliable, fast, pre-interventional imaging investigation in patients with carotid artery stenosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Atherosclerosis of the carotid arteries is a major cause of stroke and transient ischemic attack [1, 2]. Stroke is fatal in about 40% of cases, and surviving individuals often suffer from severe disabilities that require costly clinical care [2, 3]. Often atherothromboembolism from a focal atherosclerotic plaque at the carotid bifurcation is the cause of stroke and carotid stenosis and is present in about 25% of all strokes [4, 5].
Imaging investigations for diagnosis of significant carotid artery stenosis include digital subtraction angiography (DSA), MR angiography (MRA), Doppler ultrasonography (US) and also multi-detector row CT angiography (CTA) [6–16]. DSA is still considered the gold standard for evaluation of carotid artery stenosis, but the risk of neurological complications is estimated to be between 0.05 to 0.5% [17, 18]. Ultrasound is not capable of imaging all vessels that are relevant for the brain’s blood supply. Therefore, in clinical practice non-invasive imaging techniques such as MRA or CTA are used for diagnosis and pre-therapeutical planning [7, 19–23]. With the advent of higher field strengths (3 T), MRA has evolved as a powerful tool for imaging of the extracranial and intracranial vessels [19–25]. However, contrast-enhanced MRA still suffers with problems of movement and susceptibility artifact around the aortic arch, which can only party be avoided by right-sided contrast injections. With improved spatial and temporal resolution in CT and the introduction of dual-source CT (DSCT), CTA also has evolved considerably over the last years to become an accurate and reliable tool to assess the degree of carotid artery stenosis [26–33]. Clinical studies have shown that the degree of stenosis, the clinical presentation of the patient and how quickly the patient is imaged are the most important determining factors whether or not a conservative management or an invasive treatment is necessary. Concerning invasive treatments, there is a constant debate as to whether percutaneous balloon angioplasty with subsequent stent placement or surgical endarterectomy is the method of choice. Irrespective of this discussion, before each therapeutic approach, detailed knowledge of the anatomy, possible variations and the vessel pathology of all major cerebral arteries is important and may become even more crucial in the future [34, 35]. Moreover, in depth evaluation of the stenotic vessel with respect to its configuration and the plaque composition may help to improve patient outcome [36]. Still, most previously published studies focused mainly on the evaluation of the carotid vessel itself.
The aim of the present study was to compare 3T-MRA and dual-source CT (DSCT) angiography in preoperative evaluation of intra- and extracranial vessel anatomy and pathology in patients with symptomatic carotid artery stenosis before surgical carotid endartherectomy with respect to the visualization of both the diseased vessel segment and also the other vessels that may play a role in the treatment decision.
Material and methods
Patient population
Sixteen clinically symptomatic patients (2 female, 14 male, mean age 67.2 ± 12.3) with regular kidney function and suspected stenosis of the carotid artery and lumen reduction of at least 50% on duplex were prospectively enrolled in this study [37]. Ethical approval was given by the local ethics committee, and all patients gave informed consent for all procedures. Within a timeframe of 3 days both DSCT and 3T-MRA were successfully completed in all patients.
DSCT was performed using a SOMATOM Definition CT system (Siemens Medical Solutions, Forchheim, Germany). A dual-energy protocol with tube settings of 140 kV/55 mAs for tube A and 80 kV/230 mAs for tube B was applied. A collimation of 2 × 2 × 32 × 0.6 mm with z-sharp technology, a pitch of 0.65 and a rotation time of 0.33 s were used. For optimal bolus timing the test bolus technique with 20 ml of iodine-containing contrast media (Ultravist 300, Bayer-Schering, Berlin, Germany) injected into a right-sided cubital vein at a flow rate of 6.1 ml/s followed by a 40-ml saline chaser was performed before the actual CT data acquisition. The optimal delay was then individually determined from the time enhancement curve. For the main CT data acquisition, 123 ml of contrast medium was applied through an intravenous 18-gauge i.v. line followed by a saline chaser of 40 ml, both injected with the identical flow rate of 6.1 ml/s. CT data were acquired in a caudo-cranial direction from the aortic arch to the top of the skull. Images were reconstructed with 0.6-mm slice thickness and an increment of 0.4 mm applying a smooth convolution kernel. In addition, coronal and sagittal multiplanar reformations and maximum intensity projections were reconstructed.
MRA angiography
All MR examinations were performed at a 3T- MR scanner (Achieva, Philips Medical Systems, Best, The Netherlands). Patients were examined in a supine position using an eight-channel head-neck coil. Followed by a survey, anatomical FLAIR and the following non-enhanced image sequences were acquired: fluid-attenuated inversion recovery (FLAIR) sequences (TR/TE/FA/TI: 11,000/125/90/2,800) covering the whole head with 5-mm sections; diffusion-weighted sequences (DWI) (TR/TE/FA: 1,920,877/55/90) and unenhanced time-of-flight angiographies (TR/TE/FA) (25/3.45/20). The latter was performed with a matrix of 1,024 × 1,024 and a FOV of 200 × 200 mm2. Slice thickness was 1 mm resulting in an voxel size of 0.2 × 0.2 × 0.2.
Contrast-enhanced (CE) MRA was performed using a bolus tracking method using 20 ml of gadolinium (Multihance, Bracco) injected at 3 ml/s. Parameters for the CE sequence were as follows: TR 4.1 ms; TE 1.15 ms, flip angle 40 matrix 352 × 351, slice thickness 60 mm and voxel size 0.57/0.57/0.80 mm3. Images were rendered as MIPs in 16 projections separately for both carotid arteries.
Image analysis
Before the study two board-certified radiologists set up a comprehensive scoring sheet for evaluation of vessel anatomy and disease within all major cerebral extra- and intracranial arteries that might potentially influence further diagnostic workup of the patient, but also the choice of treatment (Table 1). Tortuosity or elongation of a vessel was defined as a deviance from a straight vessel course with at least two curves with an angulation of less than 135° (given 180° as a straight course and 90° as a rectangular kink).
Atherosclerotic plaques were visually classified into soft, calcified or mixed plaques. All CTA and MRA examinations were independently analyzed by these two radiologists, and inter-observer agreement between all scoring values was determined. The same radiologists also performed the consensus reading of all CT and MRI examinations. Evaluation was performed on a dedicated workstation with certified monitors and lightning. In order to exclude a recall bias a time delay of 2 months was ensured between the readings of the two investigations in each patient. Vessel visibility was evaluated using a 4-point scale with respect to the anatomic depiction, vessel edges and occurrence of artifacts (Table 2).
Statistical analysis
The characteristics of the anatomy and disease demonstrated were compared descriptively. Vessel visibility scores were analyzed applying paired samples t-tests between the two imaging investigations. P-values <0.05 were considered as statistically significant. All statistics were performed using MedCalc version 8.1.1.0 (MedCalc Software™, Mariakerke, Belgium).
Results
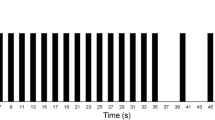
The CT and MRA examinations were successfully completed in all patients without the occurrence of any complications. All examinations were rated diagnostic, and there was no compromising venous overlay in CTA or MRA. The average duration for DSCT data acquisition was 10.4 ± 1.6 s (bolus timing excluded) with an average CTDIvol of 10.2 ± 0.8 mGy, whereas the time for MRA data acquisition was approximately 20 min.
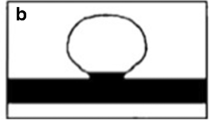
Concerning the degree of stenosis, of a total of 32 carotid arteries, 27 were consistently evaluated with both imaging investigations showing a lumen narrowing ≥70%. The remaining five carotid arteries did not show any significant stenosis in either imaging investigation. Stenosis geometry (eccentric, concentric or occluded) was consistently rated in 21 of these 27 arteries with 16 eccentric stenoses, 4 concentric stenoses and 1 occlusion). In six lesions stenosis geometry differed with respect to being eccentric or concentric with CTA calling two of these lesions eccentric, while MRA revealed eccentric lesions in the other four vessels. Concerning plaque characterization, MRA using the employed routine techniques did not reveal additional information, whereas CTA was capable of rating the 27 lesions as being soft (n = 3), calcified (n = 5) or of a mixed type (n = 19) (Fig. 1); a wall adherent thrombus was not detected by either investigation.
When evaluating the elongation of the common carotid artery, there was a 100% consensus between CTA and MRA, with 2 CCAs being rated as elongated and 30 being rated as non-elongated. In seven vessels a small poststenotic caliber of the vessel was consistently noted, one artery was occluded, and the remaining 24 vessels were of normal size. Relevant stenosis of the proximal vertebral artery was consistently detected in eight vessels; seven were uniformly rated as patent. In eight additional vessels, however, MRA showed signs of significant stenosis, whereas CTA showed suspicious lesions in yet two other vessels. In two MRA examinations and in one CTA scan, however, the image quality at the origin of the supraaortic vessels was rated non-diagnostic (see evaluation of vessel visibility below).
Consistently both imaging investigations detected a total of three additional intracranial stenoses (>70% lumen narrowing) in two patients in the carotid syphon (two lesions) and in the basilary artery (one lesion).
Several anomalies were also concordantly diagnosed by both investigations: one bicarotid trunk, one direct origin of the left vertebral artery from the aortic arch, one ophthalmic collateral and one doubled middle cerebral artery (Fig. 2). MRA in addition detected one very rare case of a fenestrated basilar artery that initially was not detected by CTA (Fig. 3). No lusoric artery was noted in any of our patients.
With respect to vessel visibility, the vessels listed in Table 1 were evaluated. A total of 624 vessels or vessel segments were scored by both investigations; the results are given in Table 3. CTA and MRA did not reveal any statistically significant difference with respect to visibility of extracranial arteries. MRA, however, revealed better vessel visibility for almost all intracranial arteries; especially small arteries like the posterior communicating artery were much more visible and more frequently detected by MRA (Fig. 4).
Discussion
Different imaging investigations such as ultrasound, CT, MR and conventional invasive digital subtraction angiography are established for assessment of the extra- and intracranial arteries. Several clinical conditions require detailed information on the arterial vessel course and blood supply to allow for a correct diagnosis and choice of appropriate therapeutic procedure. US has emerged as the first-line imaging investigation, especially in the case of suspected stenotic disease of the internal carotid artery at the extracranial bifurcation. MRA, especially with introduction of high-field and parallel imaging, became the substitute for DSA in most cases for definite diagnosis and preoperative or pre-interventional planning. CTA has been shown to be also capable of correctly measuring the degree of carotid stenosis [28, 30].
Little attention, however, has been paid to the capability of CTA and MRA in imaging arterial vessel disease and vascular abnormalities aside from the carotid artery; moreover, no previous study compared the vessel visibility of all major extra- and intracranial arteries using 3T-MRA and DSCT in patients with suspected stenotic carotid disease. This information, however, has clinical relevance in a variety of case scenarios: elongation of CCA, which is difficult to access using stents; “isolated ICA” (without a contralateral first segment of the anterior cerebral artery, or anterior communicating artery and missing posterior communicating artery) with a potentially more devastating clinical course when major vessel occlusion occurs; anatomical variations important for surgical or endovascular access (height of bifurcation, etc.), associated tandem stenoses that may very well be accessible for endovascular procedures but not for surgical ones or intracranial stenoses that may lead to a change in the choice of treatment. In almost every patient additional information with respect to vessel course, carotid stenosis morphology, additional carotid stenoses and presence or absence of intracranial collaterals was acquired in our study. Intracranial variations were better depicted by MRA—however, those who remained undetected by CTA were of no clinical relevance (such as non-fusions of the basilar artery or very small anterior or posterior communicating arteries) and had no further impact on choices for treatment planning.
With respect to carotid stenosis morphology and plaque composition, DSCT proved to be superior to MRA in our study. This is not surprising, however, as CT is also capable of visualizing the vessel wall and especially of showing calcifications within the atherosclerotic plaque. As the latter is important information for planning the intervention or surgery, a substantial amount of calcification will hamper the diagnostic accuracy of CTA because of the well-known blooming effect of these dense lesions. Plaque imaging with MRI will be helpful in the future, but at present is still experimental and very time consuming. For a rapid treatment decision as to whether a densely calcified eccentric high-grade stenosis is present, CTA appears to be the better alternative. Although sophisticated CTA software tools for calcium removal have not yet proved to be very efficient [38], the full information from dual-energy CTA may overcome this limitation and help even further to discriminate other plaque components, as has just been recently shown [39]. With dedicated MRI sequences applied, further analysis of plaque morphology also is possible [7, 11, 40, 41]. As we did not want to increase the overall imaging time beyond a degree that is practicable in an everyday clinical setting, these specially focused MRI sequences were not applied in our study.
While analyzing the CT- and MRI examinations, it again becomes obvious that a combination of several post-processing techniques is the key to efficient and comprehensive image interpretation. In CTA the focus was placed on axial images paired with sagittal and coronal multiplanar reformations. In MRA maximum intensity projections were most frequently the initial set of images that was reviewed followed by the source coronal or axial extra- or intracephalic angiography images. Most striking was the observed difference between CTA and MRA in image quality and vessel visibility of the intracranial vessels. Scores for vessel visibility were significantly better for almost all intracranial vessels, and smaller arteries like the posterior communicating artery were only reliably detected by MRA. Interestingly, intracranially the unenhanced time-of-flight MR sequence appeared superior to the contrast-enhanced gradient-echo sequence; this sequence comparison, however, was not thoroughly studied here and reflects a personal opinion of the authors. Although MRA revealed better intracranial image quality and (small) vessel detection, all clinically relevant information could also be perceived from the CTA images.
Our study has several limitations. The number of patients included is not very high. However, for vessel visibility numerous, mostly bilateral vessels, often divided into subsegments, were separately analyzed, which resulted in a total number of 624 vessel segments that were compared between the two imaging investigations. Moreover, the degree of stenosis of the carotid arteries was not analyzed and measured. This part, however, was left out as the still acknowledged gold standard DSA was not performed in all study participants. As mentioned above, previous studies already proved the potential of both CTA and MRA to reliably determine the degree of carotid stenosis. No inter- or intra-observer comparison was made; therefore, a consensus reading between two board certified radiologists with long-standing experience in cranial vessel analysis was performed. A future prospective study with a larger patient collective, inclusion of DSA data, high field MRI plaque imaging and dual-energy CT data is desirable and our focus.
Our results indicate that both DSCT and 3T-MRA are comparable at imaging both the extra- and intra-cranial arterial vessels and are helpful in diagnosis finding and pre-interventional planning. Although MRA proved to be superior in assessment of especially small intracranial arteries, all clinically relevant information needed for pre-interventional planning could be perceived from the DSCT examinations. Moreover, DSCT also allowed for dedicated depiction of carotid plaque calcifications. The two main CTA downsides are the radiation exposure and the administration of iodine-containing contrast media; these minor risks need to be balanced before DSCT can be recommended as an alternative to MRA in the pre-interventional assessment of carotid artery stenosis.
References
Seeger JM, Barratt E, Lawson GA, Klingman N (1995) The relationship between carotid plaque composition, plaque morphology, and neurologic symptoms. J Surg Res 58:330–336
Rosamond W, Flegal K, Furie K et al (2008) Heart disease and stroke statistics-2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 117:e25–e146
Feigin VL, Lawes CM, Bennett DA, Anderson CS (2003) Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case fatality in the late 20th century. Lancet Neurol 2:43–53
Bots ML, Hoes AW, Hofman A, Witteman JC, Grobbee DE (1999) Cross-sectionally assessed carotid intima-media thickness relates to long-term risk of stroke, coronary heart disease and death as estimated by available risk functions. J Intern Med 245:269–276
Hademenos GJ, Massoud TF (1997) Biophysical mechanisms of stroke. Stroke 28:2067–2077
Hankey GJ, Warlow CP, Sellar RJ (1990) Cerebral angiographic risk in mild cerebrovascular disease. Stroke 21:209–222
Essig M, Nikolaou K, Meaney JF (2007) Magnetic resonance angiography of the head and neck vessels. Eur Radiol 17(Suppl 2):B30–B37
Modaresi KB, Cox TC, Summers PE et al (1999) Comparison of intra-arterial digital subtraction angiography, magnetic resonance angiography and duplex ultrasonography for measuring carotid artery stenosis. Br J Surg 86:1422–1426
Patel MR, Kuntz KM, Klufas RA et al (1995) Preoperative assessment of the carotid bifurcation. Can magnetic resonance angiography and duplex ultrasonography replace contrast arteriography? Stroke 26:1753–1758
Scarabino T, Carriero A, Magarelli N et al (1998) MR angiography in carotid stenosis: a comparison of three techniques. Eur J Radiol 28:117–125
Thurnher SA (2005) MRA of the carotid arteries. Eur Radiol 15(Suppl 5):E11–E16
Clevert DA, Johnson T, Jung EM, Clevert DA, Flach PM, Strautz TI, Ritter G, Gallegos MT, Kubale R, Becker C, Reiser M (2007) Color Doppler, power Doppler and B-flow ultrasound in the assessment of ICA stenosis: Comparison with 64-MD-CT angiography. Eur Radiol 17:2149–2159
Derdeyn CP, Powers WJ, Moran CJ, Cross DT 3rd, Allen BT (1995) Role of Doppler US in screening for carotid atherosclerotic disease. Radiology 197:635–643
Nieman K, van der Lugt A, Pattynama PM, de Feyter PJ (2003) Noninvasive visualization of atherosclerotic plaque with electron beam and multislice spiral computed tomography. J Interv Cardiol 16:123–128
Baum U, Anders K, Steinbichler G et al (2004) Improvement of image quality of multislice spiral CT scans of the head and neck region using a raw data-based multidimensional adaptive filtering (MAF) technique. Eur Radiol 14:1873–1881
Kramer H, Morana G (2007) Whole-body magnetic resonance angiography with blood-pool agents. Eur Radiol 17(Suppl 2):B24–B29
Willinsky RA, Taylor SM, TerBrugge K, Farb RI, Tomlinson G, Montanera W (2003) Neurologic complications of cerebral angiography: prospective analysis of 2,899 procedures and review of the literature. Radiology 227:522–528
Dawkins AA, Evans AL, Wattam J et al (2007) Complications of cerebral angiography: a prospective analysis of 2,924 consecutive procedures. Neuroradiology 49:753–759
Lohan DG, Barkhordarian F, Saleh R et al (2007) MR angiography at 3 T for assessment of the external carotid artery system. AJR Am J Roentgenol 189:1088–1094
DeMarco JK, Huston J 3rd, Nash AK (2006) Extracranial carotid MR imaging at 3T. Magn Reson Imaging Clin N Am 14:109–121
Harloff A, Zech T, Frydrychowicz A, Schumacher M, Schöllhorn J, Hennig J, Weiller C, Markl M (2009) Carotid intima-media thickness and distensibility measured by MRI at 3 T versus high-resolution ultrasound. Eur Radiol 19(6):1470–1479
Borisch I, Horn M, Butz B et al (2003) Preoperative evaluation of carotid artery stenosis: comparison of contrast-enhanced MR angiography and duplex sonography with digital subtraction angiography. Am J Neuroradiol 24:1117–1122
Nederkoorn PJ, van der Graaf Y, Hunink MG (2003) Duplex ultrasound and magnetic resonance angiography compared with digital subtraction angiography in carotid artery stenosis - a systematic review. Stroke 34:1324–1332
Barth A, Arnold M, Mattle HP, Schroth G, Remonda L (2006) Contrast-enhanced 3-D MRA in decision making for carotid endarterectomy: a 6-year experience. Cerebrovasc Dis 21:393–400
Korteweg MA, Kerkhoff H, Bakker J, Elgersma OE (2008) Efficacy of patient selection strategies for carotid endarterectomy by contrast-enhanced MRA on a 1 T machine and duplex ultrasound in a regional hospital. Clin Radiol 63:174–183
Saba L, Sanfilippo R, Pirisi R, Pascalis L, Montisci R, Mallarini G (2007) Multidetector-row CT angiography in the study of atherosclerotic carotid arteries. Neuroradiology 49:623–637
Yoon DY, You SY, Choi CS et al (2006) Multi-detector row CT of the head and neck: comparison of different volumes of contrast material with and without a saline chaser. Neuroradiology 48:935–942
Bartlett ES, Walters TD, Symons SP, Fox AJ (2007) Carotid stenosis index revisited with direct CT angiography measurement of carotid arteries to quantify carotid stenosis. Stroke 38:286–291
Borisch I, Boehme T, Butz B, Hamer OW, Feuerbach S, Zorger N (2007) Screening for carotid injury in trauma patients: image quality of 16-detector-row computed tomography angiography. Acta Radiol 48:798–805
de Monye C, de Weert TT, Zaalberg W et al (2006) Optimization of CT angiography of the carotid artery with a 16-MDCT scanner: craniocaudal scan direction reduces contrast material-related perivenous artifacts. AJR Am J Roentgenol 186:1737–1745
Bartlett ES, Walters TD, Symons SP, Fox AJ (2006) Quantification of carotid stenosis on CT angiography. AJNR Am J Neuroradiol 27:13–19
Achenbach S, Ropers D, Kuettner A et al (2006) Contrast-enhanced coronary artery visualization by dual-source computed tomography–initial experience. Eur J Radiol 57:331–335
Flohr TG, McCollough CH, Bruder H et al (2006) First performance evaluation of a dual-source CT (DSCT) system. Eur Radiol 16:256–268
Barnett HJ, Taylor DW, Eliasziw M et al (1998) Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 339:1415–1425
Gurm HS, Yadav JS, Fayad P et al (2008) Long-term results of carotid stenting versus endarterectomy in high-risk patients. N Engl J Med 358:1572–1579
Haraguchi K, Houkin K, Koyanagi I, Nonaka T, Baba T (2008) Evaluation of carotid plaque composition by computed tomographic angiography and black blood magnetic resonance images. Minim Invasive Neurosurg 51:91–94
Grant EG, Benson CB, Moneta GL et al (2003) Carotid artery stenosis: gray-scale and Doppler US diagnosis–Society of Radiologists in Ultrasound Consensus Conference. Radiology 229:340–346
Simeone A, Carriero A, Armillotta M et al (1997) Spiral CT angiography in the study of the carotid stenoses. J Neuroradiol 24:18–22
Uotani K, Watanabe Y, Higashi M, Nakazawa T, Kono AK, Hori Y, Fukuda T, Kanzaki S, Yamada N, Itoh T, Sugimura K, Naito H (2009) Dual-energy CT head bone and hard plaque removal for quantification of calcified carotid stenosis: utility and comparison with digital subtraction angiography. Eur Radiol 19(8):2060–2065
Hatsukami TS, Ferguson MS, Beach KW et al (1997) Carotid plaque morphology and clinical events. Stroke 28:95–100
Alvarez-Linera J, Benito-Leon J, Escribano J, Campollo J, Gesto R (2003) Prospective evaluation of carotid artery stenosis: elliptic centric contrast-enhanced MR angiography and spiral CT angiography compared with digital subtraction angiography. AJNR Am J Neuroradiol 24:1012–1019
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mühlenbruch, G., Das, M., Mommertz, G. et al. Comparison of dual-source CT angiography and MR angiography in preoperative evaluation of intra- and extracranial vessels: a pilot study. Eur Radiol 20, 469–476 (2010). https://doi.org/10.1007/s00330-009-1547-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-009-1547-7