Abstract
The purpose was to evaluate the potential of the multidimensional adaptive filtering (MAF) technique by investigating its effects on image noise and image quality in multislice spiral CT (MSCT) examinations of the head and neck region. Fifty patients with head and neck tumors were examined using MSCT with a high resolution protocol. Reconstructions were performed using dedicated reconstruction software with a standard algorithm both without and with MAF using different modification. In all reconstructions, we measured the noise in seven different anatomical structures. The image quality and image noise were rated on a five-point scale. There was a significant (P<0.05) reduction in mean pixel noise in the reconstructions using MAF in comparison to the standard reconstructions, but there was no significant difference between the different modification fractions. With MAF the mean reduction in noise level was 60%, depending upon body shape and anatomical region. Independently from the used modification fraction, MAF led to a significant (P<0.05) improvement of image quality. In direct comparison of the different filter strength, the optimal image quality was achieved in the investigations with 15% MAF. The use of MAF facilitates the distinction of anatomical and pathological structures from artifacts in the supraclavicular fossae and the upper mediastinum, whereas the image quality of the upper portions of the neck remained unchanged. MAF improved image quality by reducing the noise level and removing noise structures without loss of image sharpness. This technique offers new perspectives to reduce the patient dose.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Technical developments in CT, with increasingly shorter scan times, shorter rotation times and thinner slices leading to higher image quality, led to a sharp increase in the number of CT examinations during the 1990s [1]. As a result of this development, the radiation exposure associated with CT increased as well. The effective dose exposure of a typical CT examination is now between 0.5 and 10 mSv depending on the scan length and scan region, thus in the same range as natural radiation exposure of about 2.4 mSv per calendar year [2, 3]. While CT accounts for only 3–5% of all radiological examinations, it is responsible for about 35–45% of the collective effective dose exposure in diagnostic radiology [1, 4]. The implementation of multislice technology not only increased the performance of CT scanning, but also patient dose exposure [5]. An important aim of the CT development is to reduce the dose required [4–6], but low contrast resolution depends crucially on the tube current. Halving the tube current and thus dose exposure increases the pixel noise by a factor of the square root of two [3, 7], if all other parameters (e.g., rotation time, tube voltage, slice width, etc.) are kept constant.
Apart from the tube current, the reconstruction algorithm and the reconstruction parameters also affect pixel noise and thus delineation of low contrast structures. Pixel noise can be reduced by using a smoothing reconstruction kernel, adequate windows and an appropriate spiral interpolation algorithm (e.g., 360°LI) [8, 9]. Additionally, advanced sliding thin slab viewing techniques reduce image noise in the viewing plane, while decreasing spatial resolution perpendicular thereto. Using these techniques some loss of image sharpness and spatial resolution is probably unavoidable [10]. A further possibility for the reduction of non-directional and directional noise is to use filters in image reconstruction. There are reports in the literature of the application of linear, median and adaptive filters [11–15]. Some of these filters operate in the raw data domain, others try to improve the image quality in the spatial domain. Operating in the spatial domain is a postprocessing technique, which cannot make use of the measured attenuation values and the photon statistics. Better results are obtained when filtering is performed in the raw data domain. Differences also exist with regard to the nature of the methods and the extent to which neighboring detectors are used. The problem with any smoothing is the loss of image sharpness. This problem can be minimized by restriction of the filter to a small region of data. Kachelrieß et al. reported on a multidimensional adaptive filtering (MAF), which uses the information from the raw data in all spatial planes, thus both in the detector plane, the projection plane and along the long axis of the patient. This increases its ability to suppress noise and, at the same time, minimizes the possible loss in image sharpness [16].
In regions of the body with high eccentricity (e.g., the shoulder or the pelvis), the noise from a small number of projections with high attenuation is dominant, and in the case of the thoracic inlet this is usually the lateral projection. MAF is particularly suitable for such images, because image sharpness, and thus spatial discrimination, requires that only a small proportion of the raw data points is changed through smoothing. In phantom examinations and in the first patient examinations, the MAF yielded promising results with noise reduction of up to 60%, especially in the shoulder region, with no detectable loss of image sharpness [16]. This suggests the need to apply this method to a larger number of patient raw data sets in the region of the thoracic inlet.
The purpose of this study was to evaluate the clinical value of this new MAF technique in a large patient group and its effect on pixel noise, image quality and clinical findings at the level of the thoracic inlet.
Materials and methods
Fifty patients with head and neck tumors and no contraindications to contrast-enhanced CT were examined in the course of tumor staging. The patients comprised 39 men and 11 women, with an age range of 40 to 80 years. The unequal distribution between the sexes is explained by the higher incidence of these tumors in men.
The examinations were performed using a multislice spiral CT (SOMATOM Volume Zoom, Siemens Medical Solutions, Erlangen, Germany) with a rotation time of 0.5 s, tube voltage of 120 kV and tube current-time product of 160 mA s. The slice collimation was 4×1 mm, with table feed of 4 mm per rotation (Pitch 1). The scan region included the region from the base of the skull to the aortic arch. For all examinations, 120-ml non-ionic iodinated contrast medium (Ultravist 300, Schering AG, Berlin) was administered intravenously at a flow rate of 2.5 ml/s and a start delay of 80 s.
The raw data sets were reconstructed on a separate workstation using dedicated reconstruction software (Syngo Explorer, VAMP GmbH, Möhrendorf, Germany) with the multidimensional standard reconstruction (180°MFI, multislice filtered interpolation) without and in combination with the multidimensional adaptive filter (180°MFI + MAF, which we briefly denote as 180°MAF). The “strength” of the multidimensional adaptive filter was varied by varying the modification fraction f. The modification fraction f is a measure of the maximum proportion of data points modified by the filter. Reconstructions of the data sets were performed using f=0%, f=5%, f=10%, f=15% and f=20%. These are designated below as 0%MAF (=180°MFI), 5%MAF, 10%MAF, 15%MAF and 20%MAF. The reconstructed slice width was 1.25 mm and the reconstruction increment 0.5 mm.
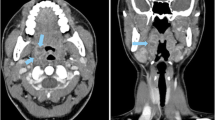
To quantify the pixel noise, the standard deviation of the attenuation (given in HU) of the pixels in a homogeneous region of interest (ROI) was determined. Using axial reconstructions with 180°MFI, we determined visually the transverse plane with the greatest noise artifacts (in all cases at the level of the head of the humerus) and the plane at the level of the carotid bifurcation as a reference for the fewest noise artifacts. Since 180°MAF modifies only image regions with high attenuation, we used four ROIs in visually homogeneous structures that are strongly affected by pixel noise (at the level of the head of the humerus, similar to Kachelrieß et al. [16]). These were the subscapularis muscle, the deltoid muscle, the supraclavicular fat tissue and the spinal canal. The carotid artery and the thyroid gland cannot be delineated at this level in some of the data sets. Both were measured because they are anatomically and clinically very relevant structures in themselves. As a reference point, we used the dorsal fat tissue, which should not be significantly modified by 180°MAF because of its location. The locations of the measurement points are shown in Fig. 1a. At the level of the carotid bifurcation, as shown in Fig. 1b, the chosen ROIs were in the carotid artery and the levator scapulae muscle. The measurements in the five reconstructions (without and with the four different modification fractions) were performed in identical positions with identical ROIs. In addition, the transverse and sagittal patient diameters were measured at both slice levels. The reduction in pixel noise was the difference in pixel noise with 180°MFI and with 180°MAF.
Measurement points a on transverse image at the level of humeral heads (1= subscapular muscle, 2= deltoid muscle, 3= supraclavicular fat tissue, 4= spinal canal, 5= carotid, 6= thyroid gland and 7= dorsal fat tissue). b On transverse image at the level of the carotid bifurcation (1= carotid, 2= levator scapulae muscle)
Image quality was evaluated by consensus between three radiologists. The images were evaluated with constant windowing with a center of 50 HU and a window of 400 HU on the monitor. Using interactive multiplanar reconstructions (iMPR) with a slice width of 1.25 mm in the axial, coronal and sagittal planes, the image quality of various anatomic structures (muscle, fat, vessels, thyroid and spinal canal) was evaluated, the critical evaluation being that of the worst region. In addition, the overall image quality was evaluated with regard to clinical aims (lymph node detection, detection of small lesions, stenosis evaluation and demonstration of plaque morphology). If pathological changes were found, they were compared in the different reconstructions with regard to detection and delineation.
The separate evaluation of the reconstructions with 0%MAF, 5%MAF, 10%MAF, 15%MAF and 20%MAF was performed at intervals of 1 week. The quality of the five anatomical structures and the overall image impression in the axial slices as well as the MPR (coronal and sagittal) of a reconstruction was rated during a single session using a five-point scale: 1= not evaluable, 2= inadequate, 3= adequate, 4= good/little artifact and 5= very good/artifact free. Overall image impression was evaluated using a three-point scale (−1= worse, 0= same and 1= better) once more independently in the axial planes and in the coronal and sagittal MPR. At least the images were compared directly.
Statistical analysis was performed using the software SPSS 11.0. The results were tested for normal distribution using the chi-square test. The standard deviations of the mean of a ROI and the image quality were compared using the one-way analysis of variance (ANOVA).
Results
Dependence of pixel noise on patient diameter (standard reconstruction)
With increasing transverse diameter, there was a significant increase in pixel noise in the two muscles, in the supraclavicular fat and in the spinal canal. For the carotid artery, the thyroid gland and the dorsal fat tissue, there was no association between transverse diameter and pixel noise.
To simplify further considerations, the mean values of the pixel noise were calculated in the structures principally affected, the two muscles and the supraclavicular fat. Figure 2 shows the increase in pixel noise with increasing transverse diameter. There was a similar relation considering the surface product that is simplified as the product of the transverse diameter and the sagittal diameter. No association was found between the pixel noise and the ratio of transverse to sagittal diameter for any measurement point.
Dependence of pixel noise. Mean value of pixel noise of supraclavicular fat tissue, deltoid muscle and subscapular muscle, measured as mean deviation of the pixel values of a ROI of an image reconstructed at the level of the humeral heads in dependence on a transverse diameter; b area product; c quotient of transverse to sagittal diameter
For both ROIs at the level of the carotid bifurcation in the carotid artery and the levator scapulae muscle, there was no association between pixel noise and transverse diameter or the ratio of transverse to sagittal diameter.
Reduction in pixel noise with various modification fractions
Table 1 summarizes the medium pixel noise of respective measurement points and the different filter strength at predefined slice positions at the thoracic inlet (Table 1) and the carotid bifurcation (Table 1). At the level of the thoracic inlet, there was a significant (P<0.05) reduction in the mean pixel noise in the reconstructions with MAF in comparison to the standard reconstructions (Fig. 3), but there was no significant difference between the different modification fractions from 5 to 20%. In the slices with least noise in the mid-neck, use of the MAF led to no significant change (P>0.05) either for the carotid artery or the levator scapulae muscle.
Figure 4 shows an example of the effect of filtering with 15% MAF depending upon the transverse diameter of the patient. The values for both curves were obtained from the mean values of the measurements of pixel noise in the subscapularis muscle, deltoid muscle and supraclavicular fat with 0%MAF and using 15%MAF. Pixel noise remains below 40 using 15%MAF, whereas noise increases above this level in the standard reconstructions with 180°MFI in 43 out of 50 patients. Noise increases to higher values than 40 HU with 15%MAF occur only in very broad patients .
Effect of filtering on image quality
Independently from the used modification fraction, MAF led to a significant (P<0.05) improvement of image quality of the muscles, the thyroid gland, the vessels and the fat tissue on axial images and on MPR, whereas the image quality of the spinal canal and the measurement points at the level of the carotid bifurcation was not significantly (P<0.05) influenced by MAF.
The image quality of the thyroid gland and the vessels could not be further improved by higher (10%, 15%, 20%) modification fractions. Image quality of the muscles and the fat tissue was significantly better (P<0.05) by using higher modification fractions, but there was no significant difference of image quality between the reconstructions with modification fractions of 10%, 15% and 20%. The results for the individual anatomical structures are summarized in Table 2(axial, MPR).
The distribution of evaluations for all 50 patients is exemplified by the overall image quality before and after filtering with 15%MAF. While the image quality with 180°MFI was good or very good (rating 4 or 5) in only 1/2 (axial/MPR) patients, this rating was obtained in 34/40 (axial/MPR) patients with 15%MAF; in 29/31 (axial/MPR) patients, image quality in the standard reconstruction with 180°MFI was not evaluable or inadequate (evaluation 1 or 2), while these ratings were given with 15%MAF for only 3/1 (axial/MPR) data sets, respectively (Fig. 5). Similar distributions were found for muscles, fat, and vessels. The effects of 15%MAF on image quality in the thyroid gland were, as expected, much less pronounced because of its eccentric location.
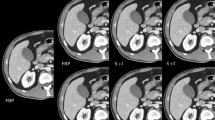
Figure 6 shows typical examples of MSCT scans in the axial and coronal planes at the level of the head of the humerus with 180°MFI (Fig. 6a,c,e,) and with 15%MAF (Fig. 6b,d,f,). The images of the patient in Fig. 6 were of poor quality in the reconstruction with 0%MAF (Figs. 6a,c,e), and MAF led to an improvement (Fig. 6b,d,f); by contrast, the image quality of another patient’s data set improved only slightly. The image quality in the upper and mid neck was similar for all modification fractions.
In direct comparison of the reconstructions with different modification fractions, the best attainable image quality was achieved with 5%MAF in 3 patients, with 10%MAF in 32 patients, with 15%MAF in 46 patients and with 20%MAF in 44 patients. In none of the patients was there further improvement in image quality with 20%MAF, but loss of definition of the musculature, vessels, fat lamellae and the bone margins was observed in five patients with 20%MAF.
The reconstructions using high modification fractions showed artifacts in the bone margins that were already present in the reconstructions without adaptive filtering, but initially (with 0%MAF) were hardly noticeable in the reconstructions because of superimposed noise structures.
Effect of filtering on detection of abnormalities
Pathological findings were detected in a total of 20 patients at the level of the thoracic inlet or the supraclavicular fossae (lymph nodes in 17 patients, thyroid changes in 3 patients and plaque in the left carotid artery in 1 patient). The detection of the lesions was easier and less time consuming in the filtered reconstructions, particularly for lymph nodes, but only in two patients lymph nodes that were not detected in the standard reconstructions were seen in the filtered images. The transversal diameter of the additionally detected lymph nodes was less than 1 cm.
Discussion
Pixel noise is largely determined by projections with high attenuation. In most non-cylindrical regions of the human body this is typically the lateral projection [3, 14]. In the region of the thoracic inlet, the attenuation due to lateral projection is particularly high if the upper arm is in the scan region as is the case with computer tomographic examinations of the head and neck region. Pixel noise is not homogeneously distributed throughout the image, but is highest in the field between the humeral heads [16].
Various attempts to reduce artifacts using filter techniques have been described in the literature [10–15]. In contrast to these techniques, the MAF technique uses a three-dimensional approach. This permits directional noise suppression proportional to the third power of the filter width and allows improvements in image quality to be achieved without impairing spatial resolution. This has two benefits: first, in regions of high radiation absorption the image quality can be improved while holding dose exposure constant, and second, the dose exposure can be reduced in slim patients without loss of image quality.
In agreement with the data published in the literature, there was an exponential relationship in our study between image noise and the transverse diameter of the object being examined [17]. In examinations of the head and neck region, this means increased noise particularly in the supraclavicular region and the musculature of the shoulder girdle. Depending upon the anatomical situation, the carotid artery and especially the thyroid gland may lie partly in a region of high lateral attenuation only, and pixel noise is thus less dependent upon patient diameter and more on the individual anatomy. The dorsal subcutaneous fat tissue is usually located outside the zone with high attenuation, and there is thus no correlation here between pixel noise and physical dimensions. In the mid-neck region, the attenuation distribution is relatively symmetric and less than at the thoracic inlet so that no directional noise occurs. Correspondingly, the multidimensional filter does not affect pixel noise in this region. The ratio of transverse diameter to sagittal diameter has no effect on pixel noise per se, since it affects eccentricity, but does not affect attenuation itself. The transverse diameter and the area product have similar correlations to pixel noise. The best correlation was found with measurement of attenuation in the lateral projection.
In evaluation of image quality, the dominant structures in the image impression and contrast were fat and muscle tissue, and a large reduction in pixel noise in these regions was extremely advantageous for detecting pathological changes. The clear correlation between the initial pixel noise and the maximum reduction achieved was most marked in these structures, and shows that applying MAF takes effect only when a certain amount of noise is present in the unfiltered image. This implies that the dose should be reduced in patients in whom the pixel noise is low with the use of 160 mA s in the standard reconstruction. The summary of measurement results and evaluation of the image quality shows that, on the one hand, in order to maintain diagnostic image quality using standard reconstruction algorithms at the thoracic inlet, the majority of patients would have required a dose above 160 mA s, but on the other hand that the tube current can be reduced for slim patients when MAF is used. Additional dose reduction in the head and neck region by new techniques, e.g., attenuation-based tube current modulation [19–26] or automatic exposure control [3] should also be pursued. The additive effect of MAF may allow for further dose reduction [3, 27].
In general, before exploiting more sophisticated ways to reduce dose exposure, first of all scan dose should be adapted to the individual patient constitution—which means a dose reduction in slim patients and an augmentation of scan dose in obese individuals. Yet, so far, trials concerning a patient-based optimization of scan dose in the head-and-neck region are missing; these topics should be addressed in future studies. In addition, CT scanners generally should be equipped with tube current modulation or, even better, automatic exposure control). Adaptive filtering within the scope of image reconstruction, as shown in this trial, can contribute to additional dose optimization and savings.
Image quality at the level of the thoracic inlet, particularly in the MPR, was significantly improved. This is due to the fact that the structures in the neck region (musculature, vessels) are shown better over their entire course in the coronal and sagittal MPR so that the reduction in pixel noise is more impressive. Streak artifacts caused by directional noise make evaluation of the supraclavicular fossa particularly difficult [15, 30]. Coronal views (MPR) are of particular value in lymph node detection in advanced head and neck tumors [31]. Coronal MPRs of the supraclavicular region often contain massive artifacts when a standard algorithm is used. The 180°MAF technique largely minimizes these artifacts and allows clear morphological evaluation of the supra-aortic vessels and lymph nodes. This allows better delineation and particularly detection of pathological structures in the MAF reconstructed images.
Even though overall image quality showed sustained improvement at the thoracic inlet, tumor staging and therapeutic strategies remained unchanged within our patient group. The additionally detected lymphatic nodules within the supraclavicular fossa in two of our patients were classified as non-pathologic and thus had no impact on tumor staging. If and to what extent the amelioration of image quality might influence tumor staging in patients with lymph node metastases, as for example in breast cancer or malignant melanoma, with lymphoma or pancoast tumor, has to be demonstrated in additional studies.
As expected, there was a significant decrease in pixel noise with increasing filter strength. At the same time, in the blind image quality evaluation, the optimal image noise and image sharpness were obtained using reconstructions with 15%MAF in 46/50 examinations. On direct comparison, a lower modification fraction gave comparable image quality in only a small proportion of patients (12%), and in 16% of cases, there was some loss of sharpness and definition of the structures with 20%MAF. Thus, for the thoracic inlet, reconstructions with 15%MAF gives excellent image quality with low pixel noise, and this can be used routinely even although stronger filtering may enable an improvement in image quality in patients with a large transverse diameter. Baum et al. reported comparable results for multislice spiral CT scans of the pelvis in patients with rectal carcinoma [32].
In conclusion, in contrast to other filter techniques, the MAF technique does not cause any loss in detailed information or resolution with modification fractions up to 15%. For further dose reduction, the procedure can be combined with tube current modulation or automatic exposure control [3, 25]. A particularly interesting application is the possibility of avoiding pinioning of the arm in a “whole body scan” in polytrauma patients. Since the MAF algorithm is conceived as a data pre-processing step, corresponding improvements should be seen with other scanners, such as the new 16-slice spiral CT scanners and their reconstruction algorithms.
References
Kaul A, Bauer B, Bernhardt J, Nosske D, Veit R (1997) Effective doses to members of the public from the diagnostic application of ionizing radiation in Germany. Eur Radiol 7:1127–1132
Kalender WA (1999) Basics and techniques of spiral CT. Radiologe 39:809–819
Kalender WA (2000) Computed tomography. MCD, München, p 137
Bauer B, Corbett R, Moores BM, Schibilla H, Teunen D (eds) (1998) Reference doses and quality in medical imaging. Radiat Prot Dosimetry 80:1–3
Brix G, Nagel HD, Stamm G, Veit R, Lechel U, Griebel J, Galanski M (2003) Radiation exposure in multi-slice versus single-slice spiral CT: results of a nations wide survey. Eur Radiol 13:1979–1991
Cohnen M, Fischer H, Hamacher J, Lins E, Kotter R, Modder U (2000) CT of the head by use of reduced current and kilovoltage: relationship between image quality and dose reduction. Am J Neuroradiol 21:1654–1660
European Commission’s Study Group (eds) (1998) Quality criteria for computed tomography. EUR 16262, 1998
Huda W, Scalzetti EM, Roskopf M (2000) Effective doses to patients undergoing thoracic CT examinations. Med Phys 27:838–844
Husstedt H, Prokop M, Becker H (1998) Window width as a dosage-relevant factor in high-contrast structures in CT. Fortschr Rontgenstr 168:139–143
Prokop M (2002) Radiation dose and image quality in computed tomography. Fortschr Rontgenstr 174:631–636
Westin CF, Richolt J, Moharir V, Kikinis R (2000) Affine adaptive filtering of CT data. Med Image Anal 4:161–177
Hu H (1999) Multi-slice helical CT: scan and reconstruction. Med Phys 26:5–18
Hu H, Shen Y (1998) Helical CT reconstruction with longitudinal filtration. Med Phys 26:2130–2138
Harpen MD (1999) A computer simulation of wavelet noise reduction in computed tomography. Med Phys 26:1600–1606
Hsieh J (1998) Adaptive streak artifact reduction in computed tomography resulting from excessive x-ray photon noise. Med Phys 25:2139–2147
Keselbrener L, Shimoni Y, Akselrod S. Nonlinear filters applied on computerized axial tomography: theory and phantom images. Med Phys 19:1057–1064
Kachelrieß M, Watzke O, Kalender WA (2001) Generalized multi-dimensional adaptive filtering for conventional and spiral single-slice, multi-slice and cone-beam CT. Med Phys 28:475–490
Haaga JR, Miraldi F, MacIntyre W, LiPuma P, Bryan PJ, Wiesen E (1981) The effect of mAs variation upon computed tomography image quality as evaluated by in vivo and in vitro studies. Radiology 138:449–454
Gies M, Kalender WA, Wolf H, Suess C (1999) Dose reduction in CT by anatomically adapted tube current modulation. I. Simulation studies. Med Phys 26:2235–2247
Giacomuzzi SM, Erckert B, Freund M, Schöpf T, Dessl A, Jaschke W (1996) Dose reduction in computerized tomography with a new scan procedure. Aktuelle Radiol 6:110–113
Giacomuzzi SM, Erckert B, Schöpf T, Freund M, Springer P, Dessl A (1996) The smart-scan procedure of spiral computed tomography. A new method for dose reduction. Fortschr Rontgenstr 163:10–16
Greess H, Wolf H, Baum U, Kalender WA, Bautz WA (1999) Dosage reduction in computed tomography by anatomy-oriented attenuation-based tube-current modulation: the first clinical results. Fortschr Rontgenstr 170:246–250
Greess H, Wolf H, Baum U, Lell M, Pirkl M, Kalender WA, Bautz W (2000) Dose reduction in CT by attenuation-based on-line modulation of tube current: evaluation of six anatomical regions. Eur Radiol 10:391–394
Kalender WA, Wolf H, Suess C, Gies M, Greess H, Bautz WA (1999) Dose reduction in CT by on-line current control: principles and validation on phantoms and cadavers. Eur Radiol 9:323–328
Kopka L, Funke M, Breiter N, Hermann K-P, Vosshenrich R, Grabbe E (1995) An anatomically adapted variation of the tube current in CT. Studies on radiation dosage reduction and image quality. Fortschr Rontgenstr 163:383–387
Greess H, Nömayr A, Wolf H, Baum U, Lell M, Böwing B, Kalender W, Bautz WA (2002) Dose reduction in CT examination of children by an attenuation-based on-line modulation of tube current (CARE Dose). Eur Radiol 12:1571–1576
Kachelrieß M, Leidecker C, Kalender WA. Patient dose reduction by combining automatic exposure control (AEC) with multidimensional adaptive filtering (MAF) for spiral CT. Eur Radiol 12(Suppl 1):196
Tack D, De Maertelaer V, Gevenois PA (2003) Am J Roentgenol 181:331–334
Vock P (2002) CT Exposition beim Kind: Geht das Erwachen der Amerikaner uns Europäer an? Radiologe 42:679–702
Tarver RD, Conces D, Godwin D (1988) Motion artifacts on CT simulate bronchiectasis. Am J Radiol 151:1117–1119
Lell M, Baum U, Koester M, Noemayr A, Greess H, Lenz M, Bautz W (1999) The morphological and functional diagnosis of the head–neck area with multiplanar spiral CT. Radiologe 39:932–938
Baum U, Noemayr A, Reissig A, Lell M, Cavallaro A, Kachelriess M, Riedel T, Kalender WA, Bautz W (2003) Improvement of the image quality of MSCT of the pelvis with a raw-data-based, multidimensional filter. Fortschr Rontgenstr 175:1572–1576
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baum, U., Anders, K., Steinbichler, G. et al. Improvement of image quality of multislice spiral CT scans of the head and neck region using a raw data-based multidimensional adaptive filtering (MAF) technique. Eur Radiol 14, 1873–1881 (2004). https://doi.org/10.1007/s00330-004-2403-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-004-2403-4