Abstract
Purpose
To investigate the radiation exposure in non-vascular fluoroscopy guided interventions and to search strategies for dose reduction.
Materials and Methods
Dose area product (DAP) of 638 consecutive non-vascular interventional procedures of one year were analyzed with respect to different types of interventions; gastrointestinal tract, biliary interventions, embolizations of tumors and hemorrhage. Data was analyzed with special focus on the fluoroscopy doses and frame doses. The third quartiles (Q3) of fluoroscopy dose values were defined in order to set a reference value for our in-hospital practice.
Results
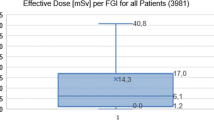
Mean fluoroscopy times of gastrostomy, jejunostomy, right and left sided percutaneous biliary drainage, chemoembolization of the liver and embolization due to various hemorrhages were 5.9, 8.6, 13.5, 16.6, 17.4 and 25.2 min, respectively. The respective Q3 total DAP were 52.9, 73.3, 155.1, 308.4, 428.6 and 529.3 Gy*cm2. Overall, around 66% of the total DAP originated from the radiographic frames with only 34% of the total DAP applied by fluoroscopy (P < 0.001). The investigators experience had no significant impact on the total DAP applied, most likely since there was no stratification to intervention-complexity.
Conclusion
To establish Diagnostic Reference Levels (DRLs), there is a need to establish a registry of radiation dose data for the most commonly performed procedures. Documentation of interventional procedures by fluoroscopy “grabbing” has the potential to considerably reduce radiation dose applied and should be used instead of radiographic frames whenever possible.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
During the last two decades, the field of interventional radiology (IR) has shown a constantly increasing number of procedures performed throughout the world as well as an impressive expansion of the spectrum of intervention types involving increasing complexity and radiation exposure [1–4]. Currently, as a general principle of IR, stepwise documentation of the procedural steps allows for comprehensive quality and safety management based on distinct and conclusive radiographic records, making the procedure transparent to all others, particularly the patients and the referring physician. Compared with formerly used sheet-film angiography, state-of-the-art angiography machines allow for high frame frequencies, nearly without limit to the total number of frames [5]. Those high-frequency frames might be necessary in vascular interventions with high-flow dynamics; however, if not specifically needed for these, their frequent use should be avoided because of high radiation doses.
Diagnostic reference levels (DRLs) are an important tool for quality assurance and improvement. Although they have been used in diagnostic radiology since the 1990 s, until to now no respective DRLs have been defined for most of the established interventional procedures [6–8]. In Germany, the Federal Office for Radiation Protection recently published a guideline dealing with radiation exposure in medicine [9]. However, due to lack of data, it only consists of reference data for some vascular procedures, such as coronary angiographies, percutaneous coronary angioplasty, and percutaneous angioplasty of the pelvic and upper-leg arteries. In this publication, clinical data from the majority of intervention sites from 2006 to 2009 were analyzed, and the third quartiles (Q3) of the pooled DAP were taken as suggested benchmarks for interventional procedures. Transarterial chemoembolization (TACE) of tumors or bleeds, percutaneous transhepatic bile duct interventions (PTCD), fluoroscopy-guided percutaneous gastrostomies (PRG), and percutaneous abscess drainages (PAD) are frequently performed procedures. However, especially in these nonvascular procedures, only a few DRLs have been published thus far [10–15]. Some of these procedures are performed repeatedly (e.g., TACE) in the same patient. In addition, basically all interventional procedures contribute not only to the radiation dose of the patient but also to the performing physician’s cumulative life dose. Therefore, the analysis of respective DAPs from daily interventional procedures is of basic interest for interventional radiologists. The purpose of this retrospective analysis was to analyze and define our in-house preliminary DRLs. The data include all fluoroscopy-guided nonvascular interventions during the period of 1 year in one of our three angiography suites.
Materials and Methods
Consecutive nonvascular interventions (n = 716) performed with an Integris V3000 angiography system (Philips, Eindhoven, the Netherlands) were included in this retrospective analysis. As part of the primary dosimetric quantity data, the DAP was registered by the integrated ionization chamber of the angiography unit (Diamentor 102 M1; PTW, Freiburg, Germany). The DAP meter was calibrated regularly using a calibrated external DAP meter (Diados; PTW). First calibration has been performed at initial certification of the angiography unit. Afterward, the correct calibration was checked twice a year by external technicians during the course of regular unit maintenance. Every fifth year, the official federal technical control board performed a detailed recertification of the entire unit, including renewal of the DAP-meter calibration. Subsequently, the intervention protocols, including the separate DAPs for fluoroscopy and frame acquisition as well as fluoroscopy times, were automatically archived and transferred to our institutional radiological information system (RIS). This was performed automatically by the angiography unit sending the information to the RIS-included DICOM-connector-MPPS-server (modality-performed procedure step) with a unique application entity title and port number using the standard DICOM interface. These protocols were analyzed with respect to fluoroscopy time and overall DAPs as well as fluoroscopy-DAPs and radiographic frame-DAPs. Similar interventional procedures were categorized and grouped, taking into account the number of patients for each procedure to achieve a sufficiently large sample size. In total, 79 rarely performed procedures could not be adequately grouped and were excluded from the analysis because the resulting patient numbers in each group were too small to reach statistical analysis. The number of interventions finally included into this analysis was 638.
The impact of the investigators experience on fluoroscopy time and DAP, frame-DAP, and total DAP was analyzed by building two groups of investigators: The first group included final-year residents and early board-certified radiologists, and the second group included senior radiologists with at least 5 years of experience in IR. We restricted our comparison of three different types of interventions (PTCD placement from the left and the right as well as liver TACE) because these interventions were the only ones performed by experienced and less experienced investigators in equal numbers. However, because of the retrospective nature of this analysis, there was no randomized allocation of clinical cases and physicians. Due to ethical issues, this also would have been not acceptable in a prospective study design. The present data, in fact, represent clinical routine, with technically complex cases being allocated to experienced senior interventional radiologists (IRs) and straightforward cases being allocated to intermediate IRs under the surveillance of senior IRs.
Statistical Analysis
Primary data were recorded using Excel 2007 by Microsoft (Richmond, WA). Calculation software was SPSS Statistics version 18 (SPSS, Chicago, IL). Fluoroscopy time, fluoroscopy-DAP, DAP of radiographic frames, and total DAP are described for each group by mean values (means), standard deviation (SD), medians, and Q3s. DAP is given in Gy*cm2. Fluoroscopy time is given in decimal fractions of minutes. Proportion of DAPs during fluoroscopy or by frame acquisition was compared for each group and for all interventions. Because the distribution of these samples was related but highly skewed and non-Gaussian, the respective DAPs were compared using Wilcoxon signed-rank test. The investigators’ experience was analyzed by comparing fluoroscopy time and fluoroscopy-DAP, frame-DAP, and total DAP of both investigator groups. Because the data were non-Gaussian and not related, the Mann–Whitney U test was applied. Statistical testing was performed by an independent statistician to avoid any review bias, and P < 0.05 was considered statistically significant.
Results
Nonvascular interventions were categorized into four groups (gastrointestinal interventions, embolizations, biliary interventions, and percutaneous abscess drainages) consisting of 11 subgroups. The number of patients varied between 7 and 165 patients/group (mean 58). Table 1 lists descriptive statistics of fluoroscopy time, mean number of frames, and total DAPs for each group of interventions. The last column shows Q3s of total DAPs to suggest preliminary in-house reference levels for the respective intervention types.
As expected, fluoroscopy time, number of frames, and total DAPs varied depending on the complexity of the procedures. Complexity might also cause respective differences within the same intervention group (e.g., PTCD control versus PTCD placement). Overall, the interventions can be divided into high- and low-dose procedures. Gastrointestinal interventions, such as PRG, PAD, and PTCD, might be categorized as low-dose procedures with relatively short fluoroscopy times and consecutively low radiation dose levels. Fluoroscopy times, number of frames, and DAPs of these procedures were 5.9 ± 5.3 min, 18 frames, 44.1 ± 49.4 Gy*cm2 (PRG); 5.4 ± 9 min, 20 frames, 54.6 ± 79.1 Gy*cm2 (abdominal PAD); 1.3 ± 2.7 min, 52 frames, 99.4 ± 72.8 Gy*cm2 (PTCD control); and 4.7 ± 7.1 min, 44 frames, 96.4 ± 77.9 Gy*cm2 (PTCD change). As noted previously, especially in these procedures, the SD in fluoroscopy time and DAP is great and could be twice as much as the mean value. These procedures were performed by all investigators, the less and the most experienced ones, demonstrating the potential for further dose decrease. However, percutaneous radiologic jejunostomies (PRJs) are intrinsically associated with greater fluoroscopy time and slightly greater DAP of 8.6 ± 8.9 min and 81.8 ± 72.9 Gy*cm2 because direct percutaneous puncture of the lumen of the jejunum might sometimes be a challenge for both, experts and beginners. A comparison of our DAPs with the data available in the literature is listed in Table 2.
The second group consisted of more complex interventions, which are associated with greater fluoroscopy times, frames’ and DAPs, such as biliary interventions with PTCD placements from left and right (16.6 ± 9.4 min, 14 frames, 213.4 ± 136.9 Gy*cm2 and 13.5 ± 9.7 min, 85 frames, 153.5 ± 161.5 Gy*cm2, respectively) or TACE of liver tumors or bleedings (17.4 ± 10.7 min, 124 frames, 395.3 ± 238.3 Gy*cm2 and 25.2 ± 11.9 min, 371 frames, 317.5 ± 184.9 Gy*cm2, respectively). As noted previously, particularly liver TACE might be associated with high cumulative DAPs for patients and IRs since usually it is performed repeatedly on a regular schedule. Because most of these patients are treated palliatively, the investigator should be aware of the radiation doses applied.
Analyzing all 638 interventions, taking into account the numbers of each procedure, 66.1% of total DAP administered was due to the acquisition of digital high-quality images, and only 33.9% were attributable to fluoroscopy (P < 0.001). Table 3 lists fluoroscopy-DAP and radiographic frame-DAP. In 5 of 11 subgroups (gastric banding–filling, TACE of liver tumors, embolization of hemorrhage, PTCD control, and PTCD change), frame acquisition of the intervention resulted in significantly greater DAPs compared with fluoroscopy phases. This means that documentation needed significantly more radiation than fluoroscopy-guided performance of the basic intervention itself. In PRG and PAD placements, the distribution between fluoroscopy-DAPs and frame-DAPs was nearly equal. In only 3 of 11 subgroups (PTCD placement from both sides as well as thoracic drainage), was fluoroscopy-DAP the leading source of total DAP (in two of them just slightly and in PTCD placement from the right side significantly).
Table 4 lists the impact of the investigators’ experience with DAP in PTCD and TACE. There were no statistically significant differences between final-year residents/early board-certified radiologists and senior radiologists. In fact, in most cases there was not even a trend toward greater DAPs in beginners. In left-sided PTCD, senior radiologists needed even greater DAPs than final-year residents/early board-certified radiologists. However, left-sided PTCD might be technically more challenging, and there was no randomized allocation of intervention and investigator.
Discussion
The present data demonstrated that fluoroscopy-induced DAPs were considerably lower compared with the DAPs applied through radiographic frame acquisition. Two thirds of total DAP originated from the acquisition of high-quality radiographic frames (34 vs. 66%, P < 0.001). The same had also been shown for invasive cardiology. Therefore, our data confirm this statement also for nonvascular radiologic interventions [16]. Apart from a few special clinical situations, high-resolution radiographic frames are only used for documentation purposes. Stepwise documentation of the entire intervention has been a good standard in IR for the last two decades. It makes the procedure more transparent for further quality-management issues and is necessary for complication and safety management. State-of-the-art angiography machines allow for “grabbing” fluoroscopy scenes with sufficient image quality [17]. We therefore suggest restricting the use of high-quality frames to documentation of the preinterventional and postinterventional status and to critical intraprocedural steps when fluoroscopy might not capture the image details or because of safety issues.
Fluoroscopy phases represent the critical phases of the intervention itself, and DAP might therefore not be arbitrarily further decreased. In contrast, high-quality frames are add-ons for documentation without additional effect on the procedure itself. Our suggestion to minimize frame acquisition is in accordance with the Cardiovascular and Interventional Radiological Society of Europe (CIRSE)/Society of Interventional Radiology guideline [18], which also recommends the use of fluoroscopy loops instead of frames for documentation based on the work of Stecker et al. [19]. In addition, our analysis has quantified the distribution of radiation between fluoroscopy and frame acquisition. It suggests Q3 in-house reference standards in fluoroscopy-guided nonvascular interventions and demonstrates the possible range of dose decreases. Moreover, the potential impact on the radiation dose for the staff is striking. Vano et al. reported that DAP of the staff might be eight times greater when using DSA frames instead of fluoroscopy scenes [20].
A comparison of our DAPs with the few existing data in the literature is barely possible. First, sufficient data are only available on liver TACE, PTCD placement, and PTCD control [10–15]. Second, the differing grouping of interventions, e.g., no side specified for PTCD, has the potential to completely alter the values. In addition, it further depends on the complexity levels of the procedures, which were not well defined and might have been different in distinct reports [21]. Compared with the data mentioned previously (Table 2), our fluoroscopy times are in the lower range for TACE (17.4 vs. 24.3, 22, and 16.8 min) and approximately one third lower than the average for PTCD placement (16.6 left side and 13.5 right side vs. 21.1 and 23.6 min, respectively). Comparing total DAP during TACE, we are in the upper range (395.3 vs. 121, 463, and 282 Gy*cm2). The same is found for PTCD placement (213.4 left side and 153.5 right side vs. 244, 71, and 150 Gy*cm2, respectively). Especially for left-hepatic PTCD placements, this is a major issue for the performing radiologist because the dose-decreasing lead shield cannot be used in many cases due to technical issues during the intervention [22]. During PTCD control, we applied approximately twice as much dose compared with Ruiz-Cruces et al. (99.4 vs. 43 Gy*cm2). The mean number of frames differs considerably in these studies and does not seem to correlate to total DAP applied with the exception of PTCD control, during which we probably acquired too many frames (52 vs. 3.8). Unfortunately, there are no reference data available giving separate dose values for fluoroscopy and frame acquisition. Therefore, our fluoroscopy DAPs reported herein might serve as preliminary internal DRLs for quality control of our in-house interventional procedures.
In the present study, the investigators experience had no significant impact on total DAPs applied. However, this retrospective analysis was not randomized. Therefore, all complex procedures were primarily performed by the experienced senior radiologists, leaving the less sophisticated ones for the beginners. In addition, residents or early board-certified colleagues were supervised and supported by an experienced senior radiologist who took over whenever necessary. Because clinical training in IR requires room for training beginners, immediate support and takeover by the senior radiologist are mandatory in cases of substantial trouble. To realistically investigate the impact of personal experience on radiation doses, the assignment of interventions to the radiologist would have to be randomized and stratified according to complexity [23]; however, this would be inacceptable according to ethical issues.
The International Commission on Radiological Protection (ICRP) recommends doses not to drop below a critical range in order to avoid inadequate image quality with consecutive loss of diagnostic information [8, 21, 24]. Therefore, IRs should be well trained, thus enabling them to decide when they can forego high-quality images without loss of diagnostic information. Restricting high-quality frames might allow for some more fluoroscopy time during the intervention for beginners. This should be helpful because the lack of routine and speed are the main reasons why other studies proved that less-experienced operators need to use more radiation during the same procedures [17, 25, 26]. Overall, a decrease of radiographic frames will be favorable for both, experienced investigators and beginners [16].
This study design was retrospective. Nonetheless, we believe that this was not disadvantageous because review bias was eliminated by not performing any preselection and instead just including all interventions and interventionalists from one angiography suite during a certain period of time. In fact, this design could be advantageous because at the point of intervention, the operators were not aware that their dose values would be analyzed afterwards. In fact, the collected data represent daily clinical routine, and the approach avoids any bias. In contrast, dose values from prospective study designs might be too low to realistically represent clinical routine because the investigators became aware of the projected radiation analysis, thus encouraging them to use less radiation [27]. Furthermore, radiation doses vary up to a factor of 6 depending on patient thickness [20]. Therefore, more exact data could have been obtained if patient body weight and thickness had been measured and registered as well. This was not performed in this study; however, there was no patient selection in our study, meaning that the respective data represent the present patient population of our hospital. Of course, variability even between formally identical procedures is great and depends on too many factors why the skewness in this study is that great. Therefore, reference levels can only serve as an orientation for investigators and patients rather than representing strict thresholds [6]. Nonetheless, particularly for frequently performed interventions, our fluoroscopy data will be used for internal quality assurance of our interventional procedures to benchmark fluoroscopy time and DAPs [28–30]. In our study, only DAP data (in Gy*cm2) were collected. A better predictor of the frequency of occurrence of deterministic skin effects is the peak skin dose (PSD) [15, 27, 31–34]. Because PSD is difficult to measure, measurement of cumulative dose (CD), in addition to DAP, is a good compromise, making it easier to compare the total amount of radiation applied in different procedures.
Altogether, the development of fluoroscopy- and frame-DRLs requires a registry of radiation doses that should not only rely on a sufficiently large patient collective but also differentiate between the complexity of different types of procedures to provide an informative basis for the miscellaneous radiation risks for specific interventions as well as various anatomic regions [10, 21, 35].
Conclusion
Two thirds of total DAP applied during nonvascular IR procedures were due to frame acquisition, and only one third was attributable to fluoroscopy. Therefore, the overall DAP can be considerably decreased by using fluoroscopy-image “grabbing” instead of radiographic frame acquisition for documentation whenever possible. To establish DRLs, there is a need to establish a registry of radiation dose data for the most commonly procedures performed from a sufficiently large number of different hospitals. Nonetheless, DRLs can always only serve as an orientation because DAP is influenced by a variety of factors. Preferably, separate DAPs for fluoroscopy and frame acquisition should be recorded to demask the fraction of radiation applied for documentation purposes only. Analyzing the impact of investigators’ experience on the DAP requires a prospective randomized trial with an additional complexity stratification, which would be inacceptable according to ethical issues.
References
Miller DL (2008) Overview of contemporary interventional fluoroscopy procedures. Health Phys 95(5):638–644
Valentin J (2000) Avoidance of radiation injuries from medical interventional procedures. Ann ICRP 30(2):7–67
Chida K, Kato M, Kagaya Y et al (2010) Radiation dose and radiation protection for patients and physicians during interventional procedure. J Radiat Res 51(2):97–105
Vano E, Sanchez R, Fernandez JM et al (2009) Patient dose reference levels for interventional radiology: a national approach. Cardiovasc Interv Radiol 32(1):19–24
Strahlenschutzkommission Cfrp (2008) Interventional radiology––recommendations for radiation protection. Bull Comm Radiat Prot 56:1–58
Wall BF, Shrimpton PC (1998) The historical development of reference doses in diagnostic radiology. Radiat Prot Dosim 80(1–3):15–20
International Commission on Radiological Protection (2001) Diagnostic reference levels in medical imaging: review and additional advice. Ann ICRP 31(4):33–52
ICRP (2007) Radiological protection in medicine. ICRP Publication 105. Ann ICRP 37(6):1–63
Nosske D (2010) Updated reference levels in diagnostic and interventional radiology. In: Federal Bulletin. Federal office for Radiation protection, Salzgitter, Germany
Vano E, Jarvinen H, Kosunen A et al (2008) Patient dose in interventional radiology: a European survey. Radiat Prot Dosim 129(1–3):39–45
Aroua A, Rickli H, Stauffer JC et al (2007) How to set up and apply reference levels in fluoroscopy at a national level. Eur Radiol 17(6):1621–1633
Miller DL, Balter S, Cole PE et al (2003) Radiation doses in interventional radiology procedures: the RAD-IR study. Part I: Overall measures of dose. J Vasc Interv Radiol 14(6):711–727
Ruiz Cruces R, Garcia-Granados J, Diaz Romero FJ, Hernandez Armas J (1998) Estimation of effective dose in some digital angiographic and interventional procedures. Br J Radiol 71(841):42–47
Zweers D, Geleijns J, Aarts NJ et al (1998) Patient and staff radiation dose in fluoroscopy-guided TIPS procedures and dose decrease using dedicated fluoroscopy exposure settings. Br J Radiol 71(846):672–676
Ruiz-Cruces R, Perez-Martinez M, Martin-Palanca A et al (1997) Patient dose in radiologically guided interventional vascular procedures: conventional versus digital systems. Radiology 205(2):385–393
Kuon E, Robinson DM, Empen K, Dahm JB (2005) Fluoroscopy time––an overestimated factor for patient radiation exposure in invasive cardiology. Fortschr Geb Rontgenstrahlen Neuen Bildgeb Verfahr Erganzungsbd 177(6):812–817
Mavrikou I, Kottou S, Tsapaki V, Neofotistou V (2008) High patient doses in interventional cardiology due to physicians′ negligence: How can they be prevented? Radiat Prot Dosim 129(1–3):67–70
Miller DL, Vano E, Bartal G et al (2009) Occupational radiation protection for interventionalists: a joint Guideline of the Cardiovascular and Interventional Radiology Society of Europe and the Society of Interventional Radiology. CIRSE SOP guideline, pp 1–18. http://www.cirse.org/index.php?pid=412
Stecker MS, Balter S, Towbin RB et al (2009) Guidelines for patient radiation dose management. J Vasc Interv Radiol 20(7):S263–S273
Vano E, Gonzalez L, Fernandez JM, Prieto C, Guibelalde E (2006) Influence of patient thickness and operation modes on occupational and patient radiation doses in interventional cardiology. Radiat Prot Dosim 118(3):325–330
Miller DL, Kwon D, Bonavia GH (2009) Reference levels for patient radiation doses in interventional radiology: proposed initial values for US practice. Radiology 253(3):753–764
d’Othee BJ, Lin PJ (2007) The influence of angiography table shields and height on patient and angiographer irradiation during interventional radiology procedures. Cardiovasc Intervent Radiol 30(3):448–454
Samara ET, Aroua A, De Palma R et al (2011) An audit of diagnostic reference levels in interventional cardiology and radiology: are there differences between academic and non-academic centres? Radiat Prot Dosim
Balter S (2008) Capturing patient doses from fluoroscopically based diagnostic and interventional systems. Health Phys 95(5):535–540
Verdun FR, Aroua A, Trueb PR, Vock P, Valley JF (2005) Diagnostic and interventional radiology: a strategy to introduce reference dose level taking into account the national practice. Radiat Prot Dosim 114(1–3):188–191
Bor D, Sancak T, Toklu T, Olgar T, Ener S (2008) Effects of radiologists’ skill and experience on patient doses in interventional examinations. Radiat Prot Dosim 129(1–3):32–35
Vehmas T (1997) Radiation exposure during standard and complex interventional procedures. Br J Radiol 70:296–298
Wall BF (2001) Diagnostic reference levels––the way forward. Br J Radiol 74(885):785–788
Vano E, Gonzalez L (2001) Approaches to establishing reference levels in interventional radiology. Radiat Prot Dosim 94(1–2):109–112
Board NRP (1990) Patient dose decrease in diagnostic radiology: Report by the Royal College of Radiologists and the National Radiological Protection Board. Doc NRPB 1(3):1–46
Castellano IA, McNeill JG, Thorp NC, Dance DR, Raphael MJ (1995) Assessment of organ radiation doses and associated risk for digital bifemoral arteriography. Br J Radiol 68(809):502–507
McParland BJ (1998) A study of patient radiation doses in interventional radiological procedures. Br J Radiol 71(842):175–185
Vano E, Gonzalez L, Ten JI, Fernandez JM, Guibelalde E, Macaya C (2001) Skin dose and dose-area product values for interventional cardiology procedures. Br J Radiol 74(877):48–55
van de Putte S, Verhaegen F, Taeymans Y, Thierens H (2000) Correlation of patient skin doses in cardiac interventional radiology with dose-area product. Br J Radiol 73(869):504–513
Marshall NW, Chapple CL, Kotre CJ (2000) Diagnostic reference levels in interventional radiology. Phys Med Biol 45(12):3833–3846
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kloeckner, R., Bersch, A., dos Santos, D.P. et al. Radiation Exposure in Nonvascular Fluoroscopy-Guided Interventional Procedures. Cardiovasc Intervent Radiol 35, 613–620 (2012). https://doi.org/10.1007/s00270-011-0206-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-011-0206-y