Abstract
Background
To evaluate FCH-PET/CT and parathyroid 4D-CT so as to guide surgery in patients with primary hyperparathyroidism (pHPT) and prior neck surgery.
Methods
Medical records of all patients referred for a FCH-PET/CT in our institution were systematically reviewed. Only patients with pHPT, a history of neck surgery (for pHPT or another reason) and an indication of reoperation were included. All patients had parathyroid ultrasound (US) and Tc-99m-sestaMIBI scintigraphy, and furthermore, some patients had 4D-CT. Gold standard was defined by pathological findings and/or US-guided fine-needle aspiration with PTH level measurement in the washing liquid.
Results
Twenty-nine patients were included in this retrospective study. FCH-PET/CT identified 34 abnormal foci including 19 ectopic localizations. 4D-CT, performed in 20 patients, detected 11 abnormal glands at first reading and 6 more under FCH-PET/CT guidance. US and Tc-99m-sestaMIBI found concordant foci in 8/29 patients. Gold standard was obtained for 32 abnormal FCH-PET/CT foci in 27 patients. On a per-lesion analysis, sensitivity, specificity, positive and negative predictive values were, respectively, 96%, 13%, 77% and 50% for FCH-PET/CT, 75%, 40%, 80% and 33% for 4D-CT. On a per-patient analysis, sensitivity was 85% for FCH-PET/CT and 63% for 4D-CT. FCH-PET/CT results made it possible to successfully remove an abnormal gland in 21 patients, including 12 with a negative or discordant US/Tc-99m-sestaMIBI scintigraphy result, with a global cure rate of 73%.
Conclusion
FCH-PET/CT is a promising tool in the challenging population of reoperative patients with pHPT. Parathyroid 4D-CT appears as a confirmatory imaging modality.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Primary hyperparathyroidism (pHPT) is a common endocrine disorder defined as an autonomous hypersecretion of parathyroid hormone (PTH) by the parathyroid gland(s) leading to an elevated serum calcium level. In most patients (80–85%) [1], pHPT is caused by a single adenoma for which surgery is the only curative treatment. Unfortunately, in less than 5% of cases with experienced teams, reoperative surgery may be required in patients who have persistent (ppHPT) or recurrent (rpHPT) primary hyperparathyroidism after surgery. The three main risk factors for persistent disease are the unknown ectopic localizations during the first surgery (found in 60% ppHPT) [2], an unrecognized multigland disease for >20% of the patients [3] and a negative preoperative imaging workup (26% of ppHPT instead of less than 2%) [4]. Reoperative neck surgery represents a technical challenge due to scar formation and distorted anatomy; this makes identification of an abnormal parathyroid gland more difficult, leads to a fivefold increase in the risk of recurrent laryngeal nerve injury and may be related to up to 20% of postoperative permanent hypoparathyroidism [5, 6]. The same challenge is encountered in patients with a history of significant neck surgery, in particular, total thyroidectomy. Therefore, in this challenging population, accurate localization by imaging is critical to achieve a safe and definitive cure.
Since overactive parathyroid glands were incidentally discovered on 18F-fluorocholine (FCH) positron emission tomography (PET)/computed tomography (CT) images performed for prostate cancer [7,8,9], several studies have investigated the performance of FCH-PET/CT in patients with pHPT [10,11,12,13,14,15,16]. Parathyroid four-dimensional computed tomography (4D-CT) scan is also emerging as an alternative imaging modality [17].
To our knowledge, these new imaging techniques have only been evaluated on small series of patients with pHPT, but never specifically in patients with previous neck surgery. The aim of this study was to investigate the performance of FCH-PET/CT and 4D-CT scan in reoperative patients with pHPT.
Patients and methods
Patients
We systematically reviewed the medical records of all patients with pHPT referred for a FCH-PET/CT in our institution. Patients were eligible for inclusion if they met the following criteria: 1—age ≥18 years old; 2—symptomatic pHPT with an indication for an iterative surgery; 3—pHPT associated with a history of neck surgery for pHPT or thyroid goiter.
The indication of pHPT surgery was assessed in a multidisciplinary consultation meeting and based on international guidelines [18]. The following parameters were recorded in all patients at the time of imaging: age, history and number of neck surgeries, histological report of previous neck surgeries, calcium and PTH serum levels, 24-h urinary calcium level and genetic testing. Long-term effects of hyperparathyroidism, such as osteopenia, osteoporosis, kidney stones and renal failure, were also systematically recorded.
pHPT was biologically defined by an elevated serum concentration of ionized calcium (>1.30 mmol/L) associated with an inappropriate serum concentration of PTH. ppHPT was defined by the persistence of these biochemical anomalies after an unsuccessful surgery, and rpHPT was defined by recurrent disease over 6 months after surgery.
Imaging
Neck ultrasonography (US)
A first high-resolution neck ultrasonography was performed with a real-time US scanner (Siemens Acuson Antarès Premium) using a 7.5–13 MHz bandwidth linear transducer by two experienced sonographers trained in parathyroid imaging (TD and AR). This first-line US was performed blinded from the 4D-CT and FCH-PET/CT results. Description of the localization of lesions was performed according to Robbins’classification [19].
Tc-99m-sestaMIBI scintigraphy
Tc-99m-sestaMIBI scintigraphy was performed on the same day as neck US by the same operator (TD or AR). Both imaging modalities were performed prior to FCH-PET/CT and 4D-CT scan (blind reading). Two different methods were performed on an Infinia GE Healthcare gamma camera (dual tracer/subtraction or single tracer/dual-phase washout (for protocol details, see additional data in: Electronic Supplementary material). When necessary, these acquisitions were completed by single-photon emission computed tomography (SPECT)/CT.
18F-FCH-PET/CT
FCH-PET/CT was used as a second-line imaging modality and performed after US and Tc-99m-sestaMIBI. Each patient was imaged with a 3D-TOF PET/CT imaging system (Siemens mCT flow 16-slice CT scanner). Image acquisitions were performed 60 min after the injection of 231 MBq ± 42 of FCH in a supine position, arms along the body (for additional protocol data, see Electronic supplementary material). Visual analysis of focal lesions detected with FCH-PET/CT was performed, combined with their semiquantitative estimation by SUVmax.
Parathyroid 4D-CT
An experienced radiologist (ME) performed parathyroid 4D-CT when prescribed by the specialist in charge of the patient. The protocol consisted of three imaging phases (Electronic Supplementary material). For 4D-CT images analysis, the operator was aware of clinical data and results of first-line imaging (US and Tc-99m-sestaMIBI). Results of FCH-PET/CT were not available at the time of first 4D-CT examination, and a second read was performed for patients with discordant results between 4D-CT and FCH-PET/CT.
Gold standard
Surgery
Results of US, Tc-99m-sestaMIBI, FCH-PET/CT and parathyroid 4D-CT scan were discussed in a multidisciplinary consultation meeting to plan and perform the intervention. Intraoperative PTH (IOPTH) measurements were performed for all patients. Patients were considered cured when IOPTH decreased >50% from baseline and achieved a level in the normal range, within 15 min after resection [20]. Furthermore, PTH serum concentration was measured at day one after surgery. Whenever possible, minimally invasive surgery was decided. Resection specimens were all sent for intraoperative frozen section and histopathological examinations. Gold standard was defined as positive when definitive histopathological findings confirmed pathological parathyroid tissue (adenoma or hyperplasia). A laryngoscopy was systematically performed before reoperation.
Postoperative complications were systematically recorded. Acute parathyroid insufficiency syndrome was defined by the need for calcium supplementation in the following days after surgery (calcium <2 mmol/l at day 1), while chronic parathyroid insufficiency syndrome was defined as permanent when calcium supplementation was still required 6 months after surgery with a serum PTH level <12 ng/l [21]. Recurrent laryngeal nerve injury was defined as permanent if vocal cord paralysis was confirmed by laryngoscopy 6 months after surgery.
US-guided FNA (fine-needle aspiration)
An US-guided FNA of the overactive parathyroid gland detected with FCH-PET/CT could be performed by an experienced radiologist using high-resolution US (SIEMENS, ACUSON Antares Premium, linear high-frequency probe 15–4 mHz) in order to confirm imaging findings before surgery when the lesion was accessible. PTH level in the needle washing liquid (PTH in situ) was systematically assayed. All samples were sent to the pathologist for a cytology analysis. Cytobiological gold standard was considered as positive (“positive FNA”) if PTH ratio (PTH in situ/PTH serum level) was greater than 2 [22]. All post-FNA complications were recorded.
Data analysis
On per-lesion analysis, imaging results were considered as true positive (TP), true negative (TN), false positive (FP) or false negative (FN) according to surgery and/or FNA findings as a gold standard.
On per-patient analysis, since the diagnosis is biologically confirmed for all patients, there were no false-positive or true-negative patients and therefore each patient was classified in only two different categories:
-
TP: patients with one or several hyperactive glands detected on imaging and confirmed by surgery or FNA findings.
-
FN: patients with negative imaging results or patients with positive imaging results subsequently confirmed as negative by surgery or FNA findings.
As a consequence of this classification, only sensitivity could be evaluated in this per-patient analysis. Exact 95% confidence intervals were obtained by the Clopper and Pearson procedure [23].
US first-line imaging performance is given for blinded first-look US and not for the second parathyroid US performed in order to guide FNA after FCH-PET/CT and 4D-CT.
FCH-PET/CT and 4D-CT results are given in an open reading.
The data for this study were extracted from the local database of PET examinations, with approval from the French authority for the protection of privacy and personal data in clinical research (CNIL, Approval No. 2111722). This study was performed according to the principles of the Declaration of Helsinki.
Results
Characteristics of patients
From January 2016 to December 2017, FCH-PET/CT was performed in 41 patients in our center. Eight patients were not included in the present study: Five patients had pHPT with no previous history of neck surgery, one patient had tertiary hyperparathyroidism, one patient had a parathyroid carcinoma and in one another patient pHPT was not confirmed. Of the remaining 33 patients, four patients were excluded (Fig. 1) and the characteristics of the remaining 29 patients included in the study are detailed in Table 1. Among them, 23 (79%) had a previous surgery for pHPT with a predominance of bilateral neck exploration, 6 (21%) had a previous neck surgery for thyroid goiter only (total thyroidectomy in 4 patients and lobectomy in 2) and 27% had both parathyroid and thyroid surgery. One case of multiple endocrine neoplasia type 1 (MEN 1) was reported in a woman with rpHPP.
All patients had an operative indication confirmed in a multidisciplinary consultation meeting, according to international guidelines [18].
Imaging data
Combining all imaging methods, 39 abnormal foci were detected including 48.7% (19/39) ectopic locations (including 2 intrathyroid lesions) (Table 2). Median size (larger diameter, mm) of the lesions detected with the different imaging methods was, respectively, 8 mm [4.8–25 mm] for FCH-PET/CT, 10 mm [6–27 mm] for 4D-CT, 8 mm [6–19 mm] for first-line US and 8 mm [5–39 mm] for Tc-99m-sestaMIBI.
FCH-PET/CT identified 34 abnormal foci (0–3 per patient), and only one patient had a negative result on all imaging modalities. The mean SUVmax at 60 min was 8.6 ± 5.1.
In addition to FCH-PET/CT, parathyroid 4D-CT was performed in 20 (69%) patients and showed 11 typical abnormal parathyroid glands at first reading. Six additional parathyroid lesions were found retrospectively after comparison to FCH-PET/CT findings.
All patients had both first-line US and Tc-99m-sestaMIBI of 11.7 (± 13.5) months before FCH-PET/CT. Twenty-two were performed with single tracer/dual phase and five with dual tracer/subtraction; for two patients explored in another institution, Tc-99m-sestaMIBI protocol is unknown. US and Tc-99m-sestaMIBI findings were both negative and discordant in 21/29 (72%) patients (Figs. 2, 3). SPECT/CT was performed (when possible) in 48% (14/29) of the patients (including 8/18 patients with negative Tc-99m-sestaMIBI results).
Patient #3 with persistent primary hyperparathyroidism after bilateral neck exploration and a total thyroidectomy for multinodular goiter, negative first-line US and Tc-99m-sestaMIBI scintigraphy (with SPECT/CT): Right cervical and paratracheal abnormal gland detected with FCH-PET/CT and 4D-CT scan and confirmed by histology. (a, b, e Coronal, sagittal and axial fused FCH-PET/CT images, c, d Tc-99m-sestaMIBI scintigraphy at 5 and 90 min postinjection showing only bilateral thyroid remnant (confirmed by SPECT/CT), f axial 4D-CT scan images, 45 s after iodine injection, g FCH-PET/CT-guided positive US enabling to perform FNA)
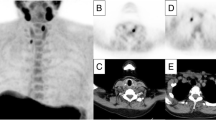
Patient #4 with persistent primary hyperparathyroidism after bilateral neck exploration and a lobectomy for thyroid nodule, negative first-line US and Tc-99m-sestaMIBI scintigraphy: abnormal parathyroid gland detected with FCH-PET/CT and 4D-CT scan in the left IIa neck level and confirmed by histology. [a, b, c coronal, axial and sagittal fused FCH-PET/CT images, d axial 4D-CT scan images, 45 s after iodine injection, e, f Tc-99m-sestaMIBI scintigraphy at 5 min postinjection showing a left thyroid remnant lobe vanishing at 90 min (f)]
Imaging performance in patients with gold standard findings (Table 3)
The gold standard (GS) was obtained for 32/39 abnormal foci in 27/29 patients. Surgery was performed in 23 patients and FNA in 15 (Table 3). One abnormal parathyroid gland was macroscopically found but left in place by the surgeon to avoid postoperative hypoparathyroidism in a MEN1 context and was considered as a positive histologic gold standard (Patient #8). One patient with a positive FNA delayed the surgical procedure for personal reasons (Patient #16).
FCH-PET/CT obtained a per-lesion sensitivity of 95.8%, significantly higher than 4D-CT (75.0%; p = 0.0026), Tc-99m-sestaMIBI scintigraphy (50.0%; p = 0.0055) and first-line neck US examination (54.2%; p = 0.0094) (Table 4). At the patient level (Table 5), FCH-PET/CT sensitivity was significantly higher than Tc-99m-sestaMIBI scintigraphy and first-line neck US examination (p = 0.0026) but not in comparison with 4D-CT (p = 0.1336).
Tc-99m-sestaMIBI scintigraphy results and protocols (subtraction versus dual phase and SPECT/CT) in the 26 patients with a GS are detailed in Table 3, and performance is summarized in Tables 4 and 5. Subtraction Tc-99m-sestaMIBI was performed in only four patients (Table 3). Diagnostic performance according to scintigraphic modalities was not statistically different.
Surgical results
Twenty-three patients underwent surgery. The surgeon was guided and enabled by FCH-PET/CT to remove an abnormal parathyroid gland in 21 patients (91%), while neck US and Tc-99m-sestaMIBI scintigraphy were concordant with true-positive findings only in 9/21 of them (43%). The median weight of removed abnormal glands was 340 mg [100–1450 mg]; it was below 200 mg for 27% of the patients.
Postoperative biochemical follow-up was available for 21/23 patients who underwent surgery. Among them, 16/21 patients were considered cured (73%). pHPT was still persistent in two patients with a negative surgery (patients #1 and #10) and three patients (#6, #11 and #23) who seemed to have a ppHPT despite a positive surgery. No patient presented postoperative permanent recurrent laryngeal nerve injury, and only one patient presented chronic parathyroid insufficiency (patient #20).
Discussion
To our knowledge, this is the first study evaluating FCH-PET/CT and 4D-CT specifically in reoperative patients. Our results confirm the superiority of FCH-PET/CT and 4D-CT compared to first-line imaging (US and Tc-99m-sestaMIBI) in this specifically challenging population.
Due to the need for dissection of scarified tissues and the technical challenge, reoperation for patients suffering from pHPT should be carefully weighed, as the complication rate is higher than 50% and the risk of failure is high even for experienced teams [3, 6]. In our study, FCH-PET/CT enabled a successful surgery in 21 patients, with pHPT healing confirmed in 16 patients, leading to a global cure rate of 73%. Five of the six patients included because of previous thyroid surgery were successfully operated upon. It is important to note that among the 21 patients operated upon, 12 patients (57%) were considered in a therapeutic impasse (not recommended for reoperation) because of a negative or discordant first-line imaging result. 4D-CT results enabled to confirm the abnormal target and reassure the surgeon for 11 of these patients, including 3 in an open reading only. Previous reports showed that 4D-CT provided higher diagnostic performance than MIBI and first-line US for preoperative localization, even in the field of persistent disease [24,25,26,27]. A recent study showed an interesting added value of a coregistration of FCH-PET/CT and 4D-CT [28]. In our study, 4D-CT also showed a higher specificity than FCH-PET/CT but the sensitivity was lower. Moreover, 4D-CT was performed in three among the six patients with FP results; this improved the specificity in only one (Patient #17). To the best of our knowledge, there is no comparison of 4D-CT with FCH-PET/CT in reoperative patients in the literature, and the positioning of 4D-CT in this setting needs to be confirmed through further studies. Nevertheless, the utility of 4D-CT must be weighted against the added radiation exposure from multiple passes, with four phases of scanning through the same anatomic region with a range of radiation exposure estimated between 10 and 27 millisievert (mSv), while FCH-PET/CT rarely exceeds 10 mSv [29].
FCH-PET/CT has a poor specificity (12.5%) with a high rate of FP lesions. No difference was observed in the SUVmax of these FP lesions versus TP ones. Few studies describe FP results and especially in a reoperative population, and the specificity of FCH-PET/CT is not available to our knowledge [30]. This result should be tempered by the fact that among the eight FP lesions in six patients only one gold standard was obtained (FNA or histology) taking into account either US-guided FNA or surgery performance. Another explanation could be a high rate of thyroid disease in four patients among the six having had past thyroid surgery.
This study could shed light on the challenge of localizing abnormal glands in these reoperative patients. Indeed, while Tc-99m-sestaMIBI and parathyroid US are still the reference for preoperative imaging modalities in pHPT, their sensitivities were particularly low in this selected population. Actually, Tc-99m-sestaMIBI and parathyroid US were already negative or discordant prior the first operation for a majority of these patients. Despite limitations due to the retrospective design of the study with different Tc-99m-sestaMIBI protocols (a majority of dual-phase protocols, the absence of 123I/sestaMIBI dual-tracer protocol providing a higher sensitivity according to the literature, and the absence of systematic SPECT/CT [31]), the low sensitivity of Tc-99m-sestaMIBI in our study is consistent with the literature in this particular population of reoperative patients [32, 33]. Actually, the lesions detected by FCH-PET/CT and 4D-CT were small (median size of 8 mm) with a large number of ectopic abnormal parathyroid glands, consistent with the high rate (60%) of ectopic lesions described in the literature in this population [2, 34]. Another potential limitation is the unblinding during image interpretation of FCH-PET/CT, which may lead to an increased performance of this modality compared to US and Tc-99m-sestaMIBI. Thus, we showed that US performance was increased when performed after FCH-PET/CT and 4D-CT in an open reading, making it possible to perform US-guided FNA before surgery (Fig. 2). US should play an important role in preoperative strategy as it might enable FNA confirmation and preoperative tattooing for surgery guidance [35].
Patient # 10 had unusual ectopic location in the sternothyroid muscle that the surgeon failed to remove despite a positive FNA. One could suspect that this location is secondary to parathyroid dispersion during one of the three previous surgeries underwent by this patient. This case illustrates the limits of detecting small lesions in a patient with previous neck surgery, even with good localization and high-resolution imaging. Indeed, in this patient the lesion was very small (8.5 mm) and superficial and it is still detected on a US examination performed after surgical failure, leading to the assumption that carbon tracking could have helped and should be more widely used in the future.
Finally, despite a high success of surgical findings (91%) and an important cure rate of more than 70% in this difficult population with several previous surgery failures, it is important to underline that three patients (#6 and #11 and #23) are still not cured despite the successful removal of an abnormal parathyroid gland. While patients #6 and #11 had a unique lesion with consistent results between US and Tc-99m-sestaMIBI, patient # 23 had three lesions described on FCH-PET/CT with only one removed during surgery. This may demonstrate the high rate of infraclinical multiglandular disease in this population with previous parathyroid surgery and the importance of prospectively evaluating the cure rate in future studies.
In conclusion, we describe here the first study focusing on FCH-PET/CT and 4D-CT performance in reoperative patients with pHPT. These first promising results need to be confirmed in a large prospective study. They may lead to promoting the use of FCH-PET/CT in reoperative patients, particularly in the event of discordant first-line imaging findings. 4D-CT parathyroid scan appears as a good confirmatory imaging modality.
References
Fraser WD (2009) Hyperparathyroidism. Lancet 374:145–158
Gough I (2006) Reoperative parathyroid surgery: the importance of ectopic location and multigland disease. ANZ J Surg 76:1048–1050
Jaskowiak N, Norton JA, Alexander HR et al (1996) A prospective trial evaluating a standard approach to reoperation for missed parathyroid adenoma. Ann Surg 224:308–320 (discussion 320–301)
Bergenfelz AO, Wallin G, Jansson S et al (2011) Results of surgery for sporadic primary hyperparathyroidism in patients with preoperatively negative sestamibi scintigraphy and ultrasound. Langenbeck’s Arch Surg/Deutsche Gesellschaft fur Chirurgie 396:83–90
Parikh PP, Farra JC, Allan BJ et al (2015) Long-term effectiveness of localization studies and intraoperative parathormone monitoring in patients undergoing reoperative parathyroidectomy for persistent or recurrent hyperparathyroidism. Am J Surg 210:117–122
Karakas E, Muller HH, Schlosshauer T et al (2013) Reoperations for primary hyperparathyroidism—improvement of outcome over two decades. Langenbeck’s Arch Surg/Deutsche Gesellschaft fur Chirurgie 398:99–106
Hodolic M, Huchet V, Balogova S et al (2014) Incidental uptake of (18)F-fluorocholine (FCH) in the head or in the neck of patients with prostate cancer. Radiol Oncol 48:228–234
Mapelli P, Busnardo E, Magnani P et al (2012) Incidental finding of parathyroid adenoma with 11C-choline PET/CT. Clin Nucl Med 37:593–595
Quak E, Lheureux S, Reznik Y et al (2013) F18-choline, a novel PET tracer for parathyroid adenoma? J Clin Endocrinol Metab 98:3111–3112
Kluijfhout WP, Pasternak JD, Gosnell JE et al (2017) 18F fluorocholine PET/MR imaging in patients with primary hyperparathyroidism and inconclusive conventional imaging: a prospective pilot study. Radiology 284:460–467
Kluijfhout WP, Vorselaars WM, Vriens MR et al (2015) Enabling minimal invasive parathyroidectomy for patients with primary hyperparathyroidism using Tc-99m-sestamibi SPECT-CT, ultrasound and first results of (18)F-fluorocholine PET-CT. Eur J Radiol 84:1745–1751
Lezaic L, Rep S, Sever MJ et al (2014) (1)(8)F-fluorocholine PET/CT for localization of hyperfunctioning parathyroid tissue in primary hyperparathyroidism: a pilot study. Eur J Nucl Med Mol Imaging 41:2083–2089
Michaud L, Balogova S, Burgess A et al (2015) A pilot comparison of 18F-fluorocholine PET/CT, ultrasonography and 123I/99mTc-sestaMIBI dual-phase dual-isotope scintigraphy in the preoperative localization of hyperfunctioning parathyroid glands in primary or secondary hyperparathyroidism: influence of thyroid anomalies. Medicine (Baltimore) 94:e1701
Michaud L, Burgess A, Huchet V et al (2014) Is 18F-fluorocholine-positron emission tomography/computerized tomography a new imaging tool for detecting hyperfunctioning parathyroid glands in primary or secondary hyperparathyroidism? J Clin Endocrinol Metab 99:4531–4536
Quak E, Blanchard D, Houdu B et al (2018) F18-choline PET/CT guided surgery in primary hyperparathyroidism when ultrasound and MIBI SPECT/CT are negative or inconclusive: the APACH1 study. Eur J Nucl Med Mol Imaging 45:658–666
van Raalte DH, Vlot MC, Zwijnenburg A et al (2015) F18-choline PET/CT: a novel tool to localize parathyroid adenoma? Clin Endocrinol (Oxf) 82:910–912
Hoang JK, Sung WK, Bahl M et al (2014) How to perform parathyroid 4D CT: tips and traps for technique and interpretation. Radiology 270:15–24
Bilezikian JP, Brandi ML, Eastell R et al (2014) Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the fourth international workshop. J Clin Endocrinol Metab 99:3561–3569
Robbins KT, Clayman G, Levine PA et al (2002) Neck dissection classification update: revisions proposed by the American Head and Neck Society and the American Academy of Otolaryngology-Head and Neck Surgery. Arch Otolaryngol Head Neck Surg 128:751–758
Fraker DL, Harsono H, Lewis R (2009) Minimally invasive parathyroidectomy: benefits and requirements of localization, diagnosis, and intraoperative PTH monitoring. Long-term results. World J Surg 33:2256–2265. https://doi.org/10.1007/s00268-009-0166-4
Stack BC Jr, Bimston DN, Bodenner DL et al (2015) American Association of Clinical Endocrinologists and American College of Endocrinology Disease State Clinical Review: postoperative hypoparathyroidism-definitions and management. Endocr Pract 21:674–685
Trimboli P, D’Aurizio F, Tozzoli R et al (2017) Measurement of thyroglobulin, calcitonin, and PTH in FNA washout fluids. Clin Chem Lab Med 55:914–925
Clopper C, Pearson E (1934) The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika 26:404–4113
Day KM, Elsayed M, Beland MD et al (2015) The utility of 4-dimensional computed tomography for preoperative localization of primary hyperparathyroidism in patients not localized by sestamibi or ultrasonography. Surgery 157:534–539
Hinson AM, Lee DR, Hobbs BA et al (2015) Preoperative 4D CT localization of nonlocalizing parathyroid adenomas by ultrasound and SPECT-CT. Otolaryngol Head Neck Surg 153:775–778
Suh YJ, Choi JY, Kim SJ et al (2015) Comparison of 4D CT, ultrasonography, and 99mTc sestamibi SPECT/CT in localizing single-gland primary hyperparathyroidism. Otolaryngol Head Neck Surg 152:438–443
Hamidi M, Sullivan M, Hunter G et al (2018) 4D-CT is superior to ultrasound and sestamibi for localizing recurrent parathyroid disease. Ann Surg Oncol 25:1403–1409
Piccardo A, Trimboli P, Rutigliani M et al. (2018) Additional value of integrated (18)F-choline PET/4D contrast-enhanced CT in the localization of hyperfunctioning parathyroid glands and correlation with molecular profile. Eur J Nucl Med Mol Imaging. https://doi.org/10.1007/s00259-018-4147-4
Campbell MJ, Sicuro P, Alseidi A et al (2015) Two-phase (low-dose) computed tomography is as effective as 4D-CT for identifying enlarged parathyroid glands. Int J Surg 14:80–84
Treglia G, Piccardo A, Imperiale A et al. (2018) Diagnostic performance of choline PET for detection of hyperfunctioning parathyroid glands in hyperparathyroidism: a systematic review and meta-analysis. Eur J Nucl Med Mol Imaging. https://doi.org/10.1007/s00259-018-4123-z
Hindie E, Zanotti-Fregonara P, Tabarin A et al (2015) The role of radionuclide imaging in the surgical management of primary hyperparathyroidism. J Nucl Med Off Publ Soc Nucl Med 56:737–744
Schalin-Jantti C, Ryhanen E, Heiskanen I et al (2013) Planar scintigraphy with 123I/99mTc-sestamibi, 99mTc-sestamibi SPECT/CT, 11C-methionine PET/CT, or selective venous sampling before reoperation of primary hyperparathyroidism? J Nucl Med Off Publ Soc Nucl Med 54:739–747
Witteveen JE, Kievit J, Stokkel MP et al (2011) Limitations of Tc99m-MIBI-SPECT imaging scans in persistent primary hyperparathyroidism. World J Surg 35:128–139. https://doi.org/10.1007/s00268-010-0818-4
Yen TW, Wang TS, Doffek KM et al (2008) Reoperative parathyroidectomy: an algorithm for imaging and monitoring of intraoperative parathyroid hormone levels that results in a successful focused approach. Surgery 144:611–619 (discussion 619–621)
Chami L, Hartl D, Leboulleux S et al (2015) Preoperative localization of neck recurrences from thyroid cancer: charcoal tattooing under ultrasound guidance. Thyroid 25:341–346
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This study has been submitted as an abstract of less than 400 words at the annual congress of the European Association of Nuclear Medicine in October 2018.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Amadou, C., Bera, G., Ezziane, M. et al. 18F-Fluorocholine PET/CT and Parathyroid 4D Computed Tomography for Primary Hyperparathyroidism: The Challenge of Reoperative Patients. World J Surg 43, 1232–1242 (2019). https://doi.org/10.1007/s00268-019-04910-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-04910-6