Abstract
Purpose
Primary hyperparathyroidism is a common endocrine disorder which is diagnosed biochemically and for which therapy is surgical. A prerequisite for minimally invasive surgery, which minimizes morbidity and cost, is accurate localization of the involved gland(s). The aim of this study was to evaluate the usefulness of 18F-fluorocholine PET/CT for preoperative localization of hyperfunctioning parathyroid tissue.
Methods
18F-Fluorocholine PET/CT and conventional parathyroid scintigraphic imaging consisting of 99mTc-sestaMIBI SPECT/CT, 99mTc-sestaMIBI dual-phase imaging and 99mTc-sestaMIBI/pertechnetate subtraction imaging were performed in 24 patients. The diagnostic performance of the imaging methods was compared against histology as the gold standard and postoperative serum Ca2+ and iPTH values.
Results
The sensitivity and specificity of 18F-fluorocholine PET/CT were 92 % and 100 %, respectively, in contrast to 49 % and 100 %, 46 % and 100 %, and 44 % and 100 % for 99mTc-sestaMIBI SPECT/CT, 99mTc-sestaMIBI/pertechnetate subtraction imaging and 99mTc-sestaMIBI dual-phase imaging, respectively. Combined conventional scintigraphic imaging had a sensitivity and specificity of 64 % and 100 %, respectively. The performance of 18F-fluorocholine PET/CT was superior particularly in patients with multiple lesions or hyperplasia.
Conclusion
18F-Fluorocholine PET/CT appears to be a promising, effective imaging method for localization of hyperfunctioning parathyroid tissue.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Primary hyperparathyroidism is a common endocrine disorder which is diagnosed biochemically and for which therapy is surgical in the vast majority of patients. The previously used surgical approach of bilateral neck exploration is being replaced by minimally invasive procedures, which have the advantages of shorter duration of surgery and general anaesthesia, lower morbidity and fewer complications with comparable success rates [1]. A prerequisite for minimally invasive surgery is successful preoperative localization of the involved parathyroid tissue. The most commonly used imaging modality for this purpose is parathyroid scintigraphy with 99mTc-sestaMIBI, usually supplemented by ultrasonography of the neck [2]. Overall, parathyroid scintigraphy is a sensitive method for localization of hyperfunctioning parathyroid tissue; however, its diagnostic performance is significantly lower in patients with multiple parathyroid lesions [3].
In contrast to conventional nuclear medicine imaging approaches for localization of the involved parathyroid tissue, hybrid imaging (PET/CT and SPECT/CT) offers the possibility of attenuation correction and coregistration of functional and anatomical information [4]; an additional advantage of PET/CT over SPECT/CT is its superior spatial resolution. 18F-Fluorocholine is a PET tracer that is commonly used for prostate cancer imaging. In contrast to 18F-FDG, it is also taken up by well-differentiated neoplasms in which 18F-FDG uptake is unreliable [5]. We hypothesized that 18F-fluorocholine might be efficiently taken up by parathyroid adenomata and/or hyperplasia.
The aim of this study was to investigate the efficiency of localization of hyperfunctioning parathyroid tissue with 18F-fluorocholine PET/CT in patients with primary hyperparathyroidism and to compare its performance with that of conventional scintigraphic imaging methods for this purpose.
Materials and methods
A group of 24 consecutive patients (20 women, 4 men; age range 42 – 77 years) with biochemically proven primary hyperparathyroidism with serum Ca2+ 2.41 – 2.83 mmol/L (median 2.68 mmol/L) and iPTH 7.1 – 37.6 pmol/L (median 8.8 pmol/L; 67.4 – 357.0 pg/mL, median 83.5 pg/mL) were referred for preoperative scintigraphic imaging in addition to ultrasonography of the neck to localize the hyperfunctioning parathyroid tissue. No prior surgery for hyperparathyroidism or other cervical pathology had been performed. There was no medical history of neoplastic or inflammatory/infectious disease in the area of head and neck and no medical history of diseases of the thyroid or potential iodine overload. Ultrasonography of the neck was performed in all patients prior to surgery.
18F-Fluorocholine PET/CT imaging and interpretation
Patients were injected with 100 MBq of 18F-fluorocholine, and 5 min after injection, low-dose CT imaging of the neck and upper mediastinum (25 mAs, CARE Dose 4D, 120 kV) was performed, immediately followed by PET imaging of the same area (one bed position, 4 min per bed position; Siemens mCT 128-slice CT scanner). Images were reconstructed using proprietary Siemens HD PET software with the iterative TrueX + TOF OSEM method (two iterations, 21 subsets). PET/CT imaging of neck and upper mediastinum was repeated 60 min after injection. Regional 18F-fluorocholine uptake not associated with thyroid tissue was considered to represent hyperfunctioning parathyroid tissue.
Conventional scintigraphic imaging, image processing and interpretation
Patients were injected with 600 MBq of 99mTc-sestaMIBI, and after 10 min, a planar image of the neck and upper mediastinum was acquired (“early” sestaMIBI planar image: matrix 128 × 128, zoom level 2.5, 10 min; Siemens BASICAM planar gamma camera), immediately followed by SPECT/CT imaging of the same area (matrix 128 × 128, zoom level 1.78, 32 projections, 20 s/frame; Siemens Symbia T2 dual-head gamma camera; low-dose CT at 25 mAs and 130 kV). Images were reconstructed using Siemens Flash3D proprietary software with the iterative OSEM method (four iterations, 16 subsets), and attenuation and scatter correction. After SPECT/CT imaging, 99mTc-sestaMIBI planar imaging was repeated 90 min after injection using identical parameters (“delayed” 99mTc-sestaMIBI planar image). Immediately after acquisition of the second 99mTc-sestaMIBI planar image and without a change in position, patients were injected with 150 MBq of pertechnetate (TcO4 −), and 15 min after injection, planar imaging of the neck and upper mediastinum was again performed using identical parameters.
For SPECT/CT imaging, regional 99mTc-sestaMIBI uptake not associated with thyroid tissue was considered to represent hyperfunctioning parathyroid tissue. For subtraction imaging, the pertechnetate planar image was subtracted from the early 99mTc-sestaMIBI planar image after normalization; the regional uptake remaining after subtraction was considered to represent hyperfunctioning parathyroid tissue. For dual-phase imaging, early and delayed 99mTc-sestaMIBI planar images were compared; regional uptake of 99mTc-sestaMIBI with slower washout than from thyroid tissue was considered to represent hyperfunctioning parathyroid tissue.
Surgical procedure, intraoperative iPTH measurements and histological confirmation
A minimally invasive focused approach parathyroidectomy was performed in patients with a single identified lesion. In patients with multiple lesions, nonlocalization or discrepancy among imaging methods, a more extensive bilateral neck exploration was chosen with intraoperative iPTH measurements at induction of general anaesthesia and 10 min after removal of the last enlarged parathyroid gland; the procedure was deemed successful if there was a decrease in the serum iPTH value by 50 % or more from the baseline value 10 min after removal of the lesion. For determination of iPTH, blood samples were collected into K2-EDTA Vacutainer™ tubes (Becton-Dickinson, Plymouth, UK). After collection, tubes were immediately transported to the laboratory, centrifuged (2,500 g, 10 min, room temperature) and analysed using a commercially available kit (cobas PTH STAT) and analyser (cobas e 411; both Roche Diagnostics, Mannheim, Germany).
The removed parathyroid glands were submitted to histopathological analysis and served as the gold standard for comparison with the noninvasive imaging results. The pathology report included gland size, weight and predominant cell type (clear, chief or oxyphil cells), if present. In all patients serum Ca2+ and iPTH values were obtained on the morning 1 day after surgery, and normalization of both values was considered to represent successful surgery.
Image processing and analysis
Images were read in five sessions: (1) 18F-fluorocholine PET/CT imaging, (2) 99mTc-sestaMIBI SPECT/CT imaging, (3) 99mTc-sestaMIBI/pertechnetate subtraction imaging, (4) 99mTc-sestaMIBI dual-phase imaging, (5) combined assessment of above-mentioned conventional scintigraphic imaging methods. Studies were anonymized and the patient list was randomized using a random list generator for each occasion. Reading sessions were held approximately 14 days apart. In each patient, five locations were evaluated for the presence/absence of regional tracer uptake considered to represent hyperfunctioning parathyroid tissue: upper left, lower left, upper right, lower right and ectopic. Surgical/histological findings were classified using the same five-location scheme.
The imaging findings were classified as follows: true-positive location with regional tracer uptake with histological confirmation of parathyroid adenoma/hyperplasia; false-positive location with regional tracer uptake with histology findings other than parathyroid adenoma/hyperplasia; false-negative location without regional tracer uptake but with histology findings of parathyroid adenoma/hyperplasia; true-negative location without regional tracer uptake and histology findings of normal parathyroid tissue; and locations without regional tracer uptake and without histological confirmation in patients whose serum Ca2+ and PTH values were normal at follow-up (i.e. presumably no remnant hyperfunctioning parathyroid tissue). For conventional scintigraphic imaging methods, a combined assessment was derived with either method (or combination of methods) classifying a lesion as positive.
Reading sessions were performed separately by two experienced observers. On review and comparison of results, disparities were resolved by consensus.
Statistical analysis
Numerical values are reported as range (median). Sensitivity, specificity, accuracy, and positive and negative predictive values of the four imaging modalities were calculated using histology analysis as the gold standard. McNemar’s test was used to compare the sensitivity and specificity of the modalities with p < 0.05 indicating a significant difference in diagnostic performance. The Kolmogorov-Smirnov test was used to assess the normality of data distributions. The Wilcoxon rank-sum test was used for continuous data as appropriate. R software package (R Foundation for Statistical Computing, Vienna, Austria) was used for statistical analysis.
Ethical considerations
The study was approved by the National Committee for Medical Ethics (no. 77/11/12). Each participant gave a written informed consent upon entering the study.
Results
Surgery, histological confirmation and follow-up
Of 39 lesions removed at surgery, histology revealed 21 adenomata (17 solitary lesions and two patients with 2 lesions) and 18 lesions with parathyroid hyperplasia (two patients with 3 and three patients with 4 hyperplastic glands); none of the histology reports indicated significant cell-type predominance. The volumes and weights of removed hyperfunctioning glands are shown in Table 1; neither of the parameters was significantly different between adenomata and hyperplastic lesions (Wilcoxon rank-sum test). On follow-up, all patients had normal serum iPTH and Ca2+ levels.
Diagnostic performance of 18F-fluorocholine PET/CT
18F-Fluorocholine PET/CT correctly localized 36 lesions. All lesions were visible at both imaging times with visually better lesion-to-background and lesion-to-thyroid contrast on delayed imaging. One lower right adenoma on imaging was classified as upper right at surgery. The surgeon designated it as upper parathyroid gland adenoma because of its position posterior to the recurrent laryngeal nerve and not because of its position relative to the thyroid gland (posteriorly located upper gland adenomata are descended upper parathyroid glands located in the tracheooesophageal groove or in a retrooesophageal location which can lie very low in the neck). The volume and weight of the three nonlocalized glands did not differ significantly from those of the localized glands (Wilcoxon rank-sum test).
Diagnostic performance of conventional scintigraphic imaging
99mTc-SestaMIBI SPECT/CT correctly localized 19 lesions. The same lesion classified as lower right 18F-fluorocholine PET/CT was identically classified on 99mTc-sestaMIBI SPECT/CT, yet surgically classified as upper right adenoma. 99mTc-sestaMIBI/pertechnetate subtraction imaging correctly localized 18 lesions. Again, one lower right lesion was classified as upper right at surgery. The performance of 99mTc-sestaMIBI dual-phase imaging was inferior to that of other conventional scintigraphic imaging methods: 17 lesions were correctly localized. With conventional imaging methods combined (i.e. either one classifying the lesion as positive on combined reading) sensitivity was improved, with 25 lesions correctly localized while maintaining perfect specificity. The combination of conventional imaging methods was significantly more sensitive than either method alone.
The sensitivity of 18F-fluorocholine PET/CT was significantly higher than that of any of the conventional imaging methods separately or combined, with no difference in specificity. The volume and weight of the nonlocalized glands was not significantly different from those of the localized glands for all conventional imaging modalities (separately and combined; Wilcoxon rank-sum test). Discordant findings (i.e. true-positive on 18F-fluorocholine PET/CT and false-negative with conventional modalities) were then compared to true-positive findings with conventional imaging modalities. Differences in gland volume were significant comparing discordant findings for 99mTc-sestaMIBI SPECT/CT (p = 0.04) and borderline significant for 99mTc-sestaMIBI/pertechnetate subtraction imaging (p = 0.05). Details are shown in Table 2.
Diagnostic performance of imaging modalities in patients with solitary parathyroid adenoma, multiple parathyroid adenomata and parathyroid hyperplasia
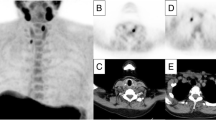
In 17 patients with solitary adenomata, 18F-fluorocholine PET/CT had a sensitivity of 94 % and specificity of 100 % for lesion localization. Again, one lesion surgically classified as upper right adenoma was placed in the lower right position on imaging. 99mTc-SestaMIBI SPECT/CT had a lower sensitivity (70 %), followed by 99mTc-sestaMIBI/pertechnetate subtraction imaging and 99mTc-sestaMIBI dual-phase imaging. Combined conventional imaging had a sensitivity of 82 % and specificity of 100 % for lesion localization. The diagnostic performance of PET was not significantly better than that of conventional imaging methods separately or combined in solitary adenomata, apart from a lower sensitivity of dual-phase imaging. An example of a solitary adenoma localized on 18F-fluorocholine PET/CT and with poor uptake on 99mTc-sestaMIBI SPECT/CT is shown in Fig. 1.
A solitary adenoma with slightly ectopic (upper right posterior paraoesophageal) localization. The lesion is well delineated on the axial 18F-fluorocholine PET image (a) and the axial PET/CT fusion image (c), while only very faint uptake is present on the axial 99mTc-sestaMIBI SPECT image (b) and the axial SPECT/CT fusion image (d)
In seven patients with multiple parathyroid lesions (two patients with two adenomata each, and two patients with three and three patients with four hyperplastic glands), by correctly localizing 20 out of 22 lesions, 18F-fluorocholine PET/CT had a sensitivity of 91 % and specificity of 100 %. Conventional nuclear medicine imaging modalities all performed identically by correctly localizing 7 of 22 lesions. Conventional imaging methods combined had a sensitivity of 50 % and specificity of 100 %. Again, the sensitivity of PET was significantly better than that of conventional imaging methods separately or combined, with no difference in specificity. An example of four-gland hyperplasia demonstrated on 18F-fluorocholine PET/CT with only one lesion visible on SPECT/CT is shown in Fig. 2.
Diagnostic performance of the imaging modalities is summarized in Table 3.
Discussion
To the best of our knowledge, this is the first study to evaluate the diagnostic performance of 18F-fluorocholine PET/CT for localization of parathyroid adenomata or hyperplasia in patients with primary hyperparathyroidism. In this small patient group 18F-fluorocholine PET/CT demonstrated very good diagnostic performance, equalling or surpassing those of other imaging modalities as reported in the literature. In particular, the diagnostic performance of 18F-fluorocholine was most impressive in patients with multiple parathyroid adenomata and hyperplasia, where other imaging modalities frequently fail to localize all hyperfunctioning lesions [3]. The failure of nuclear medicine imaging to localize multiple hyperfunctioning lesions is largely attributed to the decreased volume of individual glands [2], that is more common with parathyroid hyperplasia than with multiple adenomata. No significant differences in volume or size between adenomata and hyperplastic lesions were found in our small patient group, which can be partly attributed to several large hyperplastic lesions found. However, comparison of discordant and true-positive findings between 18F-fluorocholine PET/CT and conventional modalities, with smaller lesions being identified on PET/CT, suggests that lesion size is probably an important factor contributing the good diagnostic performance of PET/CT that can be attributed to its superior spatial resolution.
18F-Fluorocholine is mainly used for imaging prostate cancer. As a phospholipid analogue it is integrated into newly synthesized membranes of proliferating cells and its uptake in neoplastic cells is increased by upregulation of choline kinase [6]. In parathyroid adenomata, upregulation of phospholipid-dependent choline kinase has been shown to be related to PTH secretion [7]. It is plausible that both mechanisms may be responsible for uptake of 18F-fluorocholine in hyperfunctioning parathyroid tissue. PET is already used for localization of hyperfunctioning parathyroid tissue. However, none of the tested tracers have been used in clinical routine. 18F-FDG, the most common routinely used and widely available PET tracer, has been evaluated in patients with primary hyperparathyroidism with conflicting results: the sensitivity for parathyroid adenoma localization was found to be very high (94 % and 86 % [8, 9]) and disappointingly low (0 % and 22 % [10, 11]). Somewhat more consistent results have been obtained with 11C-methionine with overall sensitivities ranging from 50 % [12] to 92 % [13], and a recent review suggests the utility of 11C-methionine PET/CT in patients with nondiagnostic conventional scintigraphic imaging [4]. According to a single study, 18F-DOPA PET/CT does not have a role in parathyroid imaging [14].
Parathyroid scintigraphy is the most commonly used test to localize hyperfunctioning parathyroid tissue and 99mTc-sestaMIBI/pertechnetate subtraction imaging is the most commonly used and suggested technique among scintigraphic approaches due to its proven diagnostic accuracy [3]. Surprisingly, in our patient group we did not find the performance of subtraction scintigraphy to be comparable to that of 18F-fluorocholine PET/CT or to its performance reported in the literature. The probable reason was the extraordinarily high percentage of multiple parathyroid adenomata and hyperplasia in our patient cohort (seven patients, 22 lesions out of 39), significantly exceeding their usually reported prevalence of up to 15 % in patients with primary hyperparathyroidism [1]. In these patients, the sensitivity of conventional scintigraphic methods has been reported to be low (16 % to 35 %) [2]. In patients with solitary adenomata, the performance of subtraction scintigraphy was similar to that reported in concise reviews [3], but was again not significantly better than those of the other two conventional scintigraphic techniques.
Limitations
It must be noted that the protocol used was not optimal for subtraction imaging. Ideally, pertechnetate imaging is performed first and no patient movement is allowed between pertechnetate and 99mTc-sestaMIBI injection in order to optimize subtraction of the thyroid image from the combined parathyroid/thyroid image [15]. However, the used a “hybrid” protocol allows three recommended approaches (subtraction, dual-phase and SPECT or SPECT/CT) to be combined and compared; in particular, the approach is advised in areas where goitre is endemic [15]. In our analysis, the combined reading of conventional scintigraphic imaging methods outperformed either method alone and the sensitivity of combined reading in patients with solitary lesions was comparable that reported in the literature. A very similar imaging approach was used in a recent comprehensive retrospective single-centre analysis of the diagnostic performance of conventional scintigraphic imaging methods [16], with similar conclusions: the authors found that the combination of methods resulted in improved sensitivity of parathyroid lesion detection. Finally, the number of patients in this pilot study was small, which would probably have affected the performance of conventional scintigraphic diagnostic modalities and was also the most likely reason for the observed discrepancy in diagnostic performance between our study and the previously reported study. Confirmation of these results in a larger sample is needed.
Conclusion
This pilot study suggested that 18F-fluorocholine PET/CT is an accurate, efficient imaging modality for localization of hyperfunctioning parathyroid tissue, particularly in patients with multiple lesions or hyperplasia, in which the diagnostic performance of conventional scintigraphic imaging methods is often unsatisfactory.
References
Lew JI, Solorzano CC. Surgical management of primary hyperparathyroidism: state of the art. Surg Clin N Am. 2009;89:1205–25.
Johnson NA, Carty SE, Tublin ME. Parathyroid imaging. Radiol Clin N Am. 2011;49:489–509.
Taieb D, Hindie E, Grassetto G, Colletti PM, Rubello D. Parathyroid scintigraphy: when, how, and why? A concise systematic review. Clin Nucl Med. 2012;37(6):568–74.
Grassetto G, Alavi A, Rubello D. PET and parathyroid. PET Clin. 2008;2:385–93.
Treglia G, Giovannini E, Di Franco D, Calcagni ML, Rufini V, Picchio M, et al. The role of positron emission tomography using carbon-11 and fluorine-18 choline in tumors other than prostate cancer: a systematic review. Ann Nucl Med. 2012;26:451–61.
Jadvar H. Prostate cancer: PET with 18F-FDG, 18F- or 11C-acetate, and 18F- or 11C-choline. J Nucl Med. 2011;52:81–9.
Ishizuka T, Kajita K, Kamikubo K, Komaki T, Miura K, Nagao S, et al. Phospholipid/Ca2+-dependent protein kinase activity in human parathyroid adenoma. Endocrinol Jpn. 1987;34:965–8.
Neumann DR, Esselstyn Jr CB, MacIntyre WJ, Chen EQ, Go RT, Kohse LM, et al. Primary hyperparathyroidism: preoperative parathyroid imaging with regional body FDG PET. Radiology. 1994;192:509–12.
Neumann DR, Esselstyn CB, Maclntyre WJ, Go RT, Obuchowski NA, Chen EQ, et al. Comparison of FDG-PET and sestamibi-SPECT in primary hyperparathyroidism. J Nucl Med. 1996;37:1809–15.
Sisson JC, Thompson NW, Ackerman RJ, Wahl RL. Use of 2-[F-18]-fluoro-2-deoxy-D-glucose PET to locate parathyroid adenomas in primary hyperparathyroidism. Radiology. 1994;192:280.
Melon P, Luxen A, Hamoir E, Meurisse M. Fluorine-18-fluorodeoxyglucose positron emission tomography for preoperative parathyroid imaging in primary hyperparathyroidism. Eur J Nucl Med. 1995;22:556–8.
Herrmann K, Takei T, Kanegae K, Shiga T, Buck AK, Altomonte J, et al. Clinical value and limitations of [11C]-methionine PET for detection and localization of suspected parathyroid adenomas. Mol Imaging Biol. 2009;11:356–63.
Tang BN, Moreno-Reyes R, Blocklet D, Corvilain B, Cappello M, Delpierre I, et al. Accurate pre-operative localization of pathological parathyroid glands using 11C-methionine PET/CT. Contrast Media Mol Imaging. 2008;3:157–63.
Lange-Nolde A, Zajic T, Slawik M, Brink I, Reincke M, Moser E, et al. PET with 18F-DOPA in the imaging of parathyroid adenoma in patients with primary hyperparathyroidism. A pilot study. Nuklearmedizin. 2006;45:193–6.
Hindié E, Ugur O, Fuster D, O’Doherty M, Grassetto G, Ureña P, et al. 2009 EANM parathyroid guidelines. Eur J Nucl Med Mol Imaging. 2009;36:1201–16.
Nichols KJ, Tomas MB, Tronco GG, Rini JN, Kunjummen BD, Heller KS, et al. Preoperative parathyroid scintigraphic lesion localization: accuracy of various types of readings. Radiology. 2008;248:221–32.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lezaic, L., Rep, S., Sever, M.J. et al. 18F-Fluorocholine PET/CT for localization of hyperfunctioning parathyroid tissue in primary hyperparathyroidism: a pilot study. Eur J Nucl Med Mol Imaging 41, 2083–2089 (2014). https://doi.org/10.1007/s00259-014-2837-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-014-2837-0