Abstract
Purpose
To evaluate the added value of 18F-Fluorocholine (18F-FCH) PET/CT in presurgical imaging of patients with primary hyperparathyroidism (HPT) and challenging localization of the hyper-functioning parathyroid glands.
Methods
We included 27 consecutive patients with primary HPT (19 F; median age: 58 years), with either (i) non-conclusive pre-surgical localization with 99mTc-sestaMIBI scintigraphy and neck ultrasonography (US), (ii) recurrence of previously operated HPT, or (iii) familiar HPT with a suspicion of multiple gland disease. Histological findings and resolution of HPT were considered as the gold standard.
Results
18F-FCH PET/CT was positive in 24/27 patients. Twenty-one patients underwent surgery with 27 resected lesions (14 adenomas, 11 hyperplastic glands, two hyper-functioning histologically normal glands), with resolution of HPT in 19/21 patients (90%). 18F-FCH PET/CT localized 22 lesions in 17/21 patients (per patient: sensitivity 81%, positive predictive value (PPV) 94%; per gland: sensitivity 76%, PPV 85%, specificity 91%, negative predictive value (NPV) 86%). 18F-FCH PET/CT found eight lesions which were undetectable on both 99mTc-sestaMIBI scintigraphy and US. In patients with a familial HPT and/or a multiple gland disease, sensitivity was 100 and 79% on a per-patient and a per-gland analysis respectively, while NPV was 63%. In six patients with a persistence or recurrence of previously treated HPT, 18F-FCH PET/CT localized all lesions, both in sporadic and familiar disease.
Conclusions
18F-FCH PET/CT is a promising modality in challenging pre-surgical localization of hyper-functioning parathyroid glands, such as inconclusive standard imaging, recurrence after surgery, or suspected multiple gland disease.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Primary hyperparathyroidism (HPT) is due to parathyroid hormone (PTH) overproduction caused by a single parathyroid adenoma in more than 80% of cases and by multiple parathyroid hyperplasia or adenomas in the remaining cases [1]. In about 5–10% of patients, primary HPT occurs in the familial context of multiple endocrine neoplasia syndromes (MEN 1, 2a and 4) or in other rare syndromes [hyperparathyroidism-jaw tumor syndrome (HPT-JT), familial hypocalciuric hypercalcemia, familial isolated HPT, neonatal severe HPT or autosomal dominant moderate hyperparathyroidism] [2].
Surgery is the treatment of choice in many cases of primary HPT, in particular in symptomatic patients. A correct pre-surgical localization of the hyper-functioning parathyroid gland by imaging allows for a mini-invasive approach that results in a successful surgical resection in 95–98% of patients [3, 4]. When the pre-surgical localization is inconclusive, a surgical exploration of the four glands is mandatory, but the risk of unsuccessful intervention is increased [5].
The most commonly used pre-surgical imaging assessment is a combination of parathyroid scintigraphy with 99mTc-sestaMIBI (2-methoxyisobutylisonitrile) and neck ultrasonography (US) [6]. Different scintigraphic protocols are used, such as the single-tracer (99mTc-sestaMIBI) dual-phase protocol or the dual tracer (99mTc-sestaMIBI +99mTcO4− (pertechnetate) or 99mTc-sestaMIBI +123Iodine) subtraction protocol, sometimes in combination with a single photon emission tomography (SPECT) or SPECT/computed tomography (CT) acquisition [7, 8]. In a meta-analysis, a pooled sensitivity of 88% was reported for SPECT/CT both on a per-lesion basis and on a per-patient basis [9], compared to a previously reported pooled sensitivity of 58% for planar images alone [9,10,11]. Neck US has a sensitivity ranging from 48 to 96% [12]. The Doppler technique may increase US performance, parathyroid adenoma being highly vascularized, with a sensitivity exceeding 90% in some studies [13, 14].
Factors associated with lower performances of 99mTc-sestaMIBI scintigraphy and neck US are small increases of serum levels of PTH and ionized calcium, low parathyroid gland weight (small adenoma), the presence of multi-glandular disease, and concomitant thyroid disease. Neck US is highly operator-dependent and, in some cases, is not able to differentiate parathyroid adenomas from reactive cervical lymph nodes. Furthermore, ectopic parathyroid glands in the upper mediastinum are often inaccessible to neck US [7, 11].
In case of persistence or recurrence of HPT after a previous surgical treatment, the localization of the hyper-functioning gland is challenging for both 99mTc-sestaMIBI scintigraphy and US, because most recurrent HPT are due to multi-glandular disease or ectopic parathyroid glands, and because previous surgery creates anatomical variations in the neck [15, 16].
Since 2012, incidental findings of parathyroid adenomas have been reported in patients undergoing 11C-choline and 18F-Fluorocholine (18F-FCH) PET/CT for prostate cancer assessment [17,18,19,20]. Preliminary studies showed that 11C-choline and 18F-FCH PET/CT may localize hyper-functioning parathyroid glands both in primary and in secondary HPT, with higher sensitivity compared to 99mTc-sestaMIBI scintigraphy [21,22,23]. However, because of the high costs of the tracer, 18F-FCH PET/CT may be not cost-effective enough to substitute standard imaging techniques in all patients with primary HPT.
The aim of this study was to evaluate the added value of 18F-Fluorocholine-PET/CT in challenging localizations of hyper-functioning parathyroid glands in patients with primary HPT who were referred to two centers [Gustave Roussy (GR) and Bicetre Hospital (KB)] for surgery. Patients with sporadic primary HPT and non-conclusive pre-surgical localization on ultrasonography (US) and 99mTc-sestaMIBI scintigraphy, patients with suspicion of multiple gland disease, and patients with a persistence or recurrence of HPT after previous surgery were included in the study.
Patients and methods
Patients
Forty-six consecutive patients between September 2014 and December 2016 were prospectively evaluated by 18F-FCH PET/CT for pre-surgical evaluation of HPT.
For this analysis, we considered patients meeting the following criteria: 1) biochemical diagnosis of primary hyperparathyroidism, 2) indication for surgical treatment according to guidelines [3, 4], 3i) non-conclusive pre-surgical localization imaging on 99mTc-sestaMIBI scintigraphy and neck US, 3ii) suspicion of multiple gland disease (i.e., familiar forms of HPT), or 3iii) persistence/relapse of HPT after previous surgical treatment. A total of 27 patients met the inclusion criteria and were considered for analysis.
The remaining 19 patients were excluded from the present analysis because of diagnosis of secondary HPT (n = 1), absence of complete standard imaging with 99mTc-sestaMIBI scintigraphy and neck US (n = 7), positive and concordant 99mTc-sestaMIBI scinti graphy and neck US (n = 3), or absence of follow-up (n = 8).
99mTc-sestaMIBI scintigraphy
A dual-phase 99mTc-sestaMIBI protocol was performed in all 27 patients, with a median administered activity of 448 MBq (range: 390–728), by GE Discovery 690 at GR and Siemens Symbia T2 at KB gamma camera respectively [24] In all patients, a dynamic acquisition was obtained immediately after injection with subsequent planar images. Subsequent planar images of the neck were obtained 30 and at least 90 min after the tracer injection, using a pinhole collimator. Furthermore, a planar image at 90 min including the mediastinum was obtained with a parallel hole collimator searching for ectopic parathyroid glands. Three patients underwent a dual-isotope 99mTc-sestaMIBI/I123 subtraction protocol in addition to the dual-phase protocol described above in cases of known thyroid disease, after administration of a median administered activity of I123 of 11 MBq (range: 7–15). A supplementary SPECT/CT acquisition was performed in 17 patients (63%) with dubious findings at planar images.
Neck ultrasound
Ultrasonography (US) was performed by an expert US operator in both centers, using a linear high frequency transducer of 10 MHz. A real-time sonography combined with color-Doppler imaging was used to evaluate vascularity of the lesion and to aid differentiation of thyroid and lymph nodes from parathyroid lesions. Transverse and longitudinal views were recorded. A complete evaluation of the thyroid gland was performed in addition to the search for abnormal parathyroid glands.
18F-Fluorocholine PET/CT
All 27 patients underwent a 18F-FCH PET/CT. PET/CT imaging acquisitions were performed on a GE Discovery 690 PET/CT (General Electric Healthcare), 30 min after injection of a median 18F-FCH activity of 100 MBq (range 77–230) [25]. We administered an industrial preparation of fluoromethyl-(18F)-dimethyl-2-hydroxyethyl-ammonium, whose use is off-label in parathyroid imaging [21,22,23]. All patients gave their consent. The exam included a low-dose CT (120 kV; 210 mA, slice thickness 3.75 mm) and a PET acquisition of the head, neck, and mediastinum (3 min/bed position). All foci of uptake located behind the thyroid lobes or in the upper mediastinum were considered as positive findings for hyper-functioning parathyroid glands.
Statistics
Sensitivity and positive predictive values of 18F-Fluorocholine PET were calculated in a per-patient analysis. Sensitivity, specificity, and positive and negative predictive values were calculated in per-gland analysis.
The combination of histological findings and biochemical resolution of HPT after surgery was considered as the gold standard.
In the per-gland analysis, independently of the number of glands explored during the surgical procedure, we considered four parathyroid glands for patients with newly diagnosed HPT and the number of remaining parathyroid glands for patients already operated for HPT.
Parathyroid glands with abnormal 18F-FCH uptake, confirmed to be abnormal at histopathological examination (adenoma or hyperplasia), associated with a biochemical resolution of HPT after surgery, were classified as true positive findings. 18F-FCH uptake was considered a true positive also in case of resolution of HPT after resection of a single parathyroid gland with normal appearance at histopathological examination.
The absence of 18F-FCH uptake in a parathyroid gland confirmed to be normal at surgical exploration and/or histopathological examination was classified as a true negative finding. The absence of 18F-FCH uptake in parathyroid glands that were not explored during surgery was considered as a true negative finding in case of biochemical resolution of HPT after resection of another gland.
In case of persistent HPT after surgery, one of the not-removed glands without 18F-FCH uptake was classified as a false negative finding.
An 18F-FCH uptake in a parathyroid gland found to be normal at surgical exploration and histopathological examination was classified as a false positive finding.
Patients that did not undergo surgery were followed up and, in the absence of a gold standard, they were not considered for sensitivity, specificity, PPV analysis, and NPV analysis.
Results
Among 40 patients that underwent FCH PET/CT, a total of 27 patients (eight male, 19 female; median age: 58 years; range: 22–87 years) were considered for the analysis. Patient population characteristics are summarized in Table 1. In particular, 18 patients (67%) had 18F-FCH PET/CT for a newly diagnosed primary hyperparathyroidism, and nine (33%) for persistent or recurrent primary HPT after previous surgery. Seven cases (26%) of familial HPT were evaluated in the study, among whom five were operated.
In 23/27 patients (85%), the assessment by 99mTc-sestaMIBI scintigraphy and neck US was inconclusive: in five patients, both 99mTc-sestaMIBI scintigraphy and neck US were normal, in five 99mTc-sestaMIBI scintigraphy was normal and neck US was positive or dubious, in seven neck US was normal and 99mTc-sestaMIBI scintigraphy was positive or dubious, and in six patients 99mTc-sestaMIBI scintigraphy and neck US were both dubious or discordant.
18F-FCH PET/TC showed at least one abnormal uptake in 24/27 cases (89%) (single uptake in 17 patients and multiple uptakes in seven patients), including in the six patients who did not undergo surgery for patient refusal (n = 1), comorbidities (n = 2) or for stable calcium serum levels (n = 3). In the remaining three cases, 18F-FCH PET/CT was normal, but patients underwent surgery according to clinical indications.
Twenty-one patients underwent surgery (Table 1), with a minimally invasive approach in the case of single uptake on 18F-FCH PET/CT (n = 8), four-gland exploration in case of familial HPT and/or multiple uptakes at 18F-FCH PET/CT (n = 9), and total or partial thyroidectomy with parathyroid resection in case of concomitant thyroid disease (n = 4).
The histological examination revealed 14 adenomas, 11 hyperplastic glands and two hyper-functioning parathyroid glands with normal histological appearance. The hyper-function of these two histologically normal glands was confirmed by the resolution of HPT after their surgical removal.
One parathyroid gland was ectopic in the superior mediastinum, another one was an intrathyroidal hyperfunctioning gland. The other glands were retro-thyroidal: 11 left superior, seven left inferior, four right inferior, and three right superior.
Among the 21 operated patients, 19 (90%) had a biochemical resolution of HPT after surgery. At histology, 16 had a single abnormal gland (13 adenomas, one hyperplastic gland in a patient with a previously operated multiple gland disease, two parathyroid glands with normal histological appearance), and three had multiple abnormal glands (three hyperplastic glands in two patients, two hyperplastic glands and one adenoma in one patient).
The remaining two patients had persistent HPT after surgery. In one patient, in a context of a MEN type 1, 18F-FCH PET/CT found one abnormal uptake, while surgery found two hyperplastic glands and one normal gland that was re-implanted in the forearm. The fourth gland was not found during surgical exploration. In the second patient, in a context of sporadic HPT, 18F-FCH PET/CT found one abnormal uptake corresponding to the left inferior parathyroid gland that was resected and appeared to be normal at histological examination.
Per-patient analysis
Among the 21 patients who underwent surgery, 18F-FCH PET/CT correctly identified at least one parathyroid lesion in 17 patients. In the remaining four patients, PET was classified as a false negative: no abnormal uptake was visible in three cases (resection of two parathyroid adenomas and one normal parathyroid gland without 18F-FCH uptake, with postoperative resolution of HPT in all these patients), while in one case PET did not correctly identify the abnormal parathyroid gland, even in the presence of one abnormal uptake (uptake focus corresponding to a resected normal parathyroid gland, with persistent HPT after surgery).
Sensitivity and PPV of 18F-FCH PET/CT in operated patients were 81% and 94% respectively. Sensitivity and PPV in overall population and in different subgroups of patients are reported in Table 2.
18F-FCH -PET identified at least one lesion in all patients with familial or multi-glandular HPT and in all patients with persistent or recurrent HPT after surgery. Resolution of HPT after surgery was achieved in 5/6 patients (83%) with familial or multi-glandular HPT and in all patients (6/6) with persistent or recurrent HPT after surgery.
Age, sex, PTH and calcium serum levels in patients with a positive 18F-FCH PET/CT and patients with a normal 18F-FCH PET/CT are summarized in Table 3. In particular, median PTH serum levels was similar in patients with either a negative or a positive PET/CT.
Per-gland analysis
In the per-gland analysis, we considered a total of 74 analyzed parathyroid glands in the 21 operated patients (the four parathyroid glands for patients with newly diagnosed HPT and the remaining parathyroid glands for patients already operated for HPT). Based on histology results, we considered 29 lesions, the 27 resected parathyroid glands confirmed to be hyperfunctioning at histology and at follow-up after surgery, and the two hypothetic lesions that were not removed in the two patients with persistent HPT after surgery.
18F-FCH PET/CT correctly identified 22 out of 29 lesions. Four 18F-FCH uptakes were classified as false-positive: two faint uptakes were found to be normal parathyroid glands at surgery, a thyroid uptake due to a differentiated thyroid cancer and an undetermined thyroid uptake that was not explored, with post-operative normalization of HPT. There were seven false-negatives at 18F-FCH PET/CT: two hyperplastic glands in two patients with a multi-glandular parathyroid disease (MEN1 in both cases), one ectopic adenoma in the thyro-thymic ligament that was found at surgery, one right inferior sporadic single adenoma, one hyper-functioning parathyroid gland with a normal histologic appearance, and two lesions not found at surgery with persistent HPT after surgery (sporadic HPT in one case and familiar HPT in one case). Per-lesion sensitivity, specificity, PPV, and NPV were 76%, 91%, 85%, and 86% respectively. Sensitivity, specificity, PPV, and NPV in patients with single sporadic parathyroid adenoma, familiar or multi-glandular parathyroid disease, and relapse of HPT after previous surgery are reported in Table 4.
In 7/21 patients (33%), 18F-FCH PET/TC was able to detect eight lesions that were not detected on either 99mTc-sestaMIBI scintigraphy or neck US (four adenomas, four hyperplastic glands). Among these seven patients, three had a first diagnosis of sporadic parathyroid adenoma, one had a relapse of a previously treated sporadic adenoma, one had a familial multiple gland disease, and two had a relapse of a multiple parathyroid hyperplasia.
In patients with multi-glandular parathyroid disease, despite good values of sensitivity, specificity, and PPV, the NPV was 63% compared to 89% in patients with sporadic adenoma. In patients with a relapse of a previously treated HPT, 18F-FCH PET/CT properly localized all sites of recurrence in both patients with sporadic HPT (n = 3) and familiar forms of HPT (n = 3).
Median SUVmax was similar in case of true-positive uptakes and false-positive uptakes (4.5 (range 2.6–10.7) and 3.1 (range 1.9–5.0) respectively). Median size of true-positive lesions was 15 mm (range: 4–50) compared to 14 mm in false-negative lesions (range 9–24).
Discussion
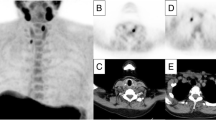
Our study demonstrates that 18F-FCH PET/CT could have an important role in patients in whom the pre-surgical detection of hyper-functioning parathyroid gland is challenging. On a per-patient analysis, sensitivity and PPV of 18F-FCH PET/CT were 81 and 94% respectively. On a per-gland analysis, sensitivity, and PPV of 18F-FCH PET/CT were 76 and 85% respectively. In one third of patients, 18F-FCH PET/TC correctly identified eight lesions that neither 99mTc-sestaMIBI scintigraphy nor neck US were able to detect (Fig. 1).
Patient with a recurrence of primary hyperparathyroidism after surgical resection of the right superior parathyroid gland, in the context of a familiar form of hyperparathyroidism (MEN1). Histopathological examination found three hyperplastic parathyroid glands. 99mTc-sestaMIBI scintigraphy correctly identified one hyperplastic parathyroid gland (white arrows; a planar images, b SPECT maximum intensity projection, c SPECT/CT axial images). 18F-FCH PET/CT correctly identified three hyperplastic parathyroid glands (white arrows, d PET maximum intensity projection, e–f PET/CT coronal images and axial images)
18F-FCH PET/CT made it possible to identify the hyper-functioning gland in two-thirds of patients with sporadic HPT and negative/inconclusive standard work-up. In patients with familial or multiple gland disease, sensitivity was 79% and 100% on a per-lesion and a per-patient basis respectively. In these patients, however, some abnormal glands could be missed, and NPV is lower in comparison to those with a sporadic single gland disease (NPV 57% and 90% respectively). This suggests the need for a complete exploration of the four parathyroid glands in case of clinically suspected multi-glandular disease (i.e., familial HPT, secondary HPT) and when two or more abnormal foci are found at imaging. Interestingly, in patients with a persistence or relapse of a surgically treated HPT, all lesions were correctly identified by 18F-FCH PET/CT, in both sporadic and familiar forms of HPT. In these patients, a correct localization of the hyper-functioning gland is essential to avoid complex and often invasive surgery in an already operated neck, with a higher rate of complications [26, 27].
Recently published studies suggest that 18F-FCH PET/CT is a promising tool in the localization of hyper-functioning gland(s) in patients with HPT, with higher sensitivity compared to 99mTc-sestaMIBI scintigraphy [21, 28]. In patients with a negative or inconclusive pre-surgical evaluation with 99mTc-sestaMIBI scintigraphy and/or US, a detection rate of hyper-functioning parathyroid gland by 18F-FCH PET/CT ranging between 77% and 94% was reported on a per-patient analysis and between 80% and 96% on a per-lesion analysis [22, 25, 29, 30]. Consistent with previous preliminary studies, our results suggest a high detection rate of hyper-functioning parathyroid glands in patients with primary HPT and negative or non-conclusive standard work-up. Nevertheless, several differences from the previous studies are relevant. In a recently published prospective study, among 24 subjects with primary HPT and negative or inconclusive standard imaging, 18F-FCH PET/CT was able to guide the surgical procedure in 22 cases, and 21/24 patients (88%) were cured after surgery [30]. Considering the APACH1 study, a higher sensitivity in a per-lesion analysis was found compared to our study (91.3% versus 76%). However, in the APACH1 study authors considered only the histopathological results as the gold standard in the per-lesion analysis, while we also took into account the resolution of HPT after surgery. Compared to other studies, in our study there was a high prevalence of patterns known to negatively influence the pre-surgical localisation imaging, such as the presence of familial multiple gland hyperplasia and the recurrence of HPT after previous surgery. Moreover, we did not include secondary HPT, surgery being of limited interest in these patients [22, 23]. Furthermore, in the present study, even when the pre-surgical localization imaging was negative, patients underwent surgery if there was formal indication, and the six patients who did not undergo surgery despite a positive 18F-FCH PET/CT were not considered for the analysis. Finally, in contrast to our criteria, in previous studies a histological gold standard was sometimes available only in a small proportion of cases and a negative localisation on 18F-FCH PET/CT was the main reason to avoid surgery, and therefore the diagnostic impact could not be evaluated [29].
A retrospective study including 151 subjects with primary HPT showed that 18F-FCH PET/CT allows minimally invasive targeted surgery in most patients with parathyroid adenoma, with a 96.8% cure rate [31]. Similarly, in our series the cure rate was high, reaching 90%. Nevertheless, the number of minimally invasive interventions was lower, due to a higher proportion of multiple gland disease and concomitant thyroid disease, requiring a four-gland exploration or a total/partial thyroidectomy.
Even if 18F-FCH PET/CT localization performances are quite good, false-positive or false-negative findings may occur. In our series, we observed four false-positive findings related to thyroid gland uptakes in two patients (one corresponding to a differentiated thyroid carcinoma) or to a faint uptake in normal parathyroid glands in two patients. Similarly, false-positive results have been reported in previous studies in cases of thyroid nodules (including differentiated thyroid carcinoma and oncocytic thyroid adenoma) and normal lymph nodes [18, 22, 23, 31]. Interestingly, 18F-FCH uptakes were also described in parathyroid carcinoma tissue both in local persistent disease and in distant metastases [32].
False negative findings (n = 7) were related to the ectopic localization of the parathyroid gland in one patient, a hyper-functioning parathyroid gland with a normal histologic appearance in one patient, and hyperplastic parathyroid glands in the context of a multi-glandular parathyroid disease in three cases, while in two patients, there was no apparent explanation for the negative 18F-FCH PET/CT. False-negative results have already been reported in previous studies in cases of ectopic glands, but also in cases of hyperplastic glands or adenomas with no specific characteristics [22, 23, 31].
To our knowledge, no study has been able to identify any predictive factor which can influence the performance of 18F-FCH PET/CT such as calcium levels, PTH levels or lesion size. In one study, PTH serum level was the only parameter which trended towards higher levels in patients with positive 18F-FCH PET/CT results than in those with a negative 18F-FCH PET/CT [29]. In our study, median PTH and calcium levels were similar on 18F-FCH PET/CT-positive and 18F-FCH PET/CT-negative cases.
Finally, our study has some limitations. The sample size is small, but similar to the majority of other studies. This is related to the selection criteria that focused on a subset of patients with primary HPT and led to the inclusion of a small percentage of patients. Moreover, the inclusion of patients with inconclusive standard imaging in most cases does not allow a comparison between 18F-FCH PET/CT and the other techniques. Nevertheless, the selection of patients with challenging detection of hyper-functioning parathyroid glands makes it possible to evaluate the added value of 18F-FCH PET/CT to standard work-up in a “real-life” setting. Some limitations are related to the 99mTc-sestaMIBI scintigraphy protocol: in particular, not all patients underwent a SPECT/CT or a dual-tracer protocol, which have been reported to have better performances than planar dual-phase imaging alone [9, 33].
Among PET tracers, before 18F-FCH, 11C-Methionine has been investigated in the pre-surgical localization of hyper-functioning parathyroid glands. A meta-analysis showed interesting results with a pooled sensitivity of 81% and a detection rate of 70%. However, its short half-life limits its applicability in daily practice [34]. Four-dimensional computed tomography (4D-CT) has been reported to be effective for the same purpose. In a meta-analysis, the sensitivity and PPV were 89.4% and 93.5% respectively; in studies in which 4D-CT was performed in patients with previously inconclusive US and scintigraphy, sensitivity and PPV were 71.8% and 74.9% respectively [12]. Moreover, promising results have been reported with magnetic resonance imaging (MRI), in particular using a 4D technique [35, 36]. As with 18F-FCH PET/CT, these techniques may be good “problem solving” modalities in patients with challenging pre-surgical localization imaging. In the absence of studies comparing their performances, the preference of one technique over the others may be based on the availability and the absence of contraindications.
Conclusion
Our study strengthens the interest of 18F-FCH PET/TC in the detection of hyper-functioning parathyroid glands in primary HPT, showing high sensitivity and specificity. Nevertheless, the use of 18F-FCH PET/CT as a first-line examination rather than 99mTc-sestaMIBI scintigraphy and US seems not to be as yet justified in all patients with HPT. The real added value appears to be in patients with inconclusive standard imaging, persistence or recurrence of HPT after previous surgery, or suspicion of multiple gland disease.
References
Al Zahrani A, Levine MA. Primary hyperparathyroidism. Lancet. 1997;349(9060):1233–8.
Iacobone M, Carnaille B, Palazzo FF, Vriens M. Hereditary hyperparathyroidism—a consensus report of the European Society of Endocrine Surgeons (ESES). Langenbecks Arch Surg. 2015;400(8):867–86.
Bilezikian JP, et al. Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the Fourth International Workshop. J Clin Endocrinol Metab. 2014;99(10):3561–9.
Khan AA, et al. Primary hyperparathyroidism: review and recommendations on evaluation, diagnosis, and management. A Canadian and international consensus. Osteoporos Int. 2017;28(1):1.
Elaraj DM, et al. Are additional localization studies and referral indicated for patients with primary hyperparathyroidism who have negative sestamibi scan results? Arch Surg. 2010;145(6):578–81.
Kunstman JW, Kirsch JD, Mahajan A, Udelsman R. Parathyroid localization and implications for clinical management. J Clin Endocrinol Metab. 2013;98(3):902–12.
Taieb D, Hindie E, Grassetto G, Colletti PM, Rubello D. Parathyroid scintigraphy: when, how, and why? A concise systematic review. Clin Nucl Med. 2012;37(6):568–74.
Taillefer R, Boucher Y, Potvin C, Lambert R. Detection and localization of parathyroid adenomas in patients with hyperparathyroidism using a single radionuclide imaging procedure with technetium-99m-sestamibi (double-phase study). J Nucl Med. 1992;33(10):1801–7.
Treglia G, et al. Detection rate of 99m Tc-MIBI single photon emission computed tomography (SPECT)/CT in preoperative planning for patients with primary hyperparathyroidism: a meta-analysis. Head Neck. 2016;38(S1):E2159–72.
Caldarella C, Treglia G, Pontecorvi A, Giordano A. Diagnostic performance of planar scintigraphy using 99mTc-MIBI in patients with secondary hyperparathyroidism: a meta-analysis. Ann Nucl Med. 2012;26(10):794–803.
Kelz RR, Fraker DL. Hyperparathyroidism. Adv Surg. 2015;49(1):247–62.
Cheung K, Wang TS, Farrokhyar F, Roman SA, Sosa JA. A meta-analysis of preoperative localization techniques for patients with primary hyperparathyroidism. Ann Surg Oncol. 2012;19(2):577–83.
Abboud B, et al. Ultrasonography: highly accuracy technique for preoperative localization of parathyroid adenoma. Laryngoscope. 2008;118(9):1574–8.
Reeder SB, Desser TS, Weigel RJ, Jeffrey RB. Sonography in primary hyperparathyroidism. J Ultrasound Med. 2002;21(5):539–52.
Parikh PP, Farra JC, Allan BJ, Lew JI. Long-term effectiveness of localization studies and intraoperative parathormone monitoring in patients undergoing reoperative parathyroidectomy for persistent or recurrent hyperparathyroidism. Am J Surg. 2015;210(1):117–22.
Shin JJ, Milas M, Mitchell J, Berber E, Ross L, Siperstein A. Impact of localization studies and clinical scenario in patients with hyperparathyroidism being evaluated for reoperative neck surgery. Arch Surg. 2011;146(12):1397–403.
Cazaentre T, Clivaz F, Triponez F. False-positive result in 18F-fluorocholine PET/CT due to incidental and ectopic parathyroid hyperplasia. Clin Nucl Med. 2014;39(6):e328–30.
Hodolic M, et al. Incidental uptake of 18F-fluorocholine (FCH) in the head or in the neck of patients with prostate cancer. Radiol Oncol. 2014;48(3):228.
Mapelli P, et al. Incidental finding of parathyroid adenoma with 11C-choline PET/CT. Clin Nucl Med. 2012;37(6):593–5.
Quak E, Lheureux S, Reznik Y, Bardet S, Aide N. F18-choline, a novel PET tracer for parathyroid adenoma? J Clin Endocrinol Metab. 2013;98(8):3111–2.
Lezaic L, Rep S, Sever MJ, Kocjan T, Hocevar M, Fettich J. 18F-Fluorocholine PET/CT for localization of hyperfunctioning parathyroid tissue in primary hyperparathyroidism: a pilot study. Eur J Nucl Med Mol Imaging. 2014;41(11):2083–9.
Michaud L, et al. A pilot comparison of 18F-fluorocholine PET/CT, ultrasonography and 123I/99mTc-sestaMIBI dual-phase dual-isotope scintigraphy in the preoperative localization of hyperfunctioning parathyroid glands in primary or secondary hyperparathyroidism: influence of thyroid anomalies. Medicine (Baltimore). 2015;94(41):e1701.
Michaud L, et al. Is 18F-fluorocholine-positron emission tomography/computerized tomography a new imaging tool for detecting Hyperfunctioning parathyroid glands in primary or secondary hyperparathyroidism? J Clin Endocrinol Metab. 2014;99(12):4531–6.
Hindié E, et al. 2009 EANM parathyroid guidelines. Eur J Nucl Med Mol Imaging. 2009;36(7):1201–16.
Kluijfhout WP, Vorselaars WMCM, Vriens MR, Borel Rinkes IHM, Valk GD, de Keizer B. Enabling minimal invasive parathyroidectomy for patients with primary hyperparathyroidism using Tc-99m-sestamibi SPECT–CT, ultrasound and first results of 18F-fluorocholine PET–CT. Eur J Radiol. 2015;84(9):1745–51.
Caron NR, Sturgeon C, Clark OH. Persistent and recurrent hyperparathyroidism. Curr Treat Options Oncol. 2004;5(4):335–45.
Wells SJ, Debenedetti M, Doherty G. Recurrent or persistent hyperparathyroidism. J Bone Min Res. 2002;17(Suppl 2):N158–62.
Orevi M, Freedman N, Mishani E, Bocher M, Jacobson O, Krausz Y. Localization of parathyroid adenoma by 11C-choline PET/CT: preliminary results. Clin Nucl Med. 2014;39(12):1033–8.
Kluijfhout WP, et al. Fluorine-18 fluorocholine PET-CT localizes hyperparathyroidism in patients with inconclusive conventional imaging: a multicenter study from the Netherlands. Nucl Med Commun. 2016;37(12):1246–52.
Quak E, et al. F18-choline PET/CT guided surgery in primary hyperparathyroidism when ultrasound and MIBI SPECT/CT are negative or inconclusive: the APACH1 study. Eur J Nucl Med Mol Imaging. 2018; https://doi.org/10.1007/s00259-017-3911-1.
M. Hocevar, et al. Focused parathyroidectomy without intraoperative parathormone testing is safe after pre-operative localization with 18F-Fluorocholine PET/CT. Eur J Surg Oncol. 2017;43(1):133–7.
Deandreis D, et al. 18Fluorocholine PET/CT in parathyroid carcinoma: a new tool for disease staging? Eur J Nucl Med Mol Imaging. 2015;42(12):1941–2.
Krakauer M, Wieslander B, Myschetzky PS, Lundstrøm A, Bacher T, Sørensen CH, et al. A prospective comparative study of parathyroid dual-phase scintigraphy, dual-isotope subtraction scintigraphy, 4D-CT, and ultrasonography in primary hyperparathyroidism. Clin Nucl Med. 2016;41:93–100.
Caldarella C, Treglia G, Isgrò MA, Giordano A. Diagnostic performance of positron emission tomography using 11C-methionine in patients with suspected parathyroid adenoma: a meta-analysis. Endocrine. 2013;43(1):78–83.
Merchavy S, Luckman J, Guindy M, Segev Y, Khafif A. 4D MRI for the localization of parathyroid adenoma: a novel method in evolution. Otolaryngol Head Neck Surg. 2016;154(3):446–8.
Sacconi B, et al. MR appearance of parathyroid adenomas at 3 T in patients with primary hyperparathyroidism: what radiologists need to know for pre-operative localization. Eur Radiol. 2016;26(3):664–73.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Serena Grimaldi declares that she has no conflict of interest, Jacques Young declares that he has no conflict of interest, Peter Kamenicky declares that he has no conflict of interest, Dana Hartl declares that she has no conflict of interest, Marie Terroir declares that she has no conflict of interest, Sophie Leboulleux declares that she has no conflict of interest, Amandine Berdelou declares that she has no conflict of interest, Julien Hadoux declares that he has no conflict of interest, Segolene Hescot declares that she has no conflict of interest, Hervé Remy declares that he has no conflict of interest, Eric Baudin declares that he has no conflict of interest, Martin Schlumberger declares that he has no conflict of interest, Désirée Deandreis declares that she has no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Grimaldi, S., Young, J., Kamenicky, P. et al. Challenging pre-surgical localization of hyperfunctioning parathyroid glands in primary hyperparathyroidism: the added value of 18F-Fluorocholine PET/CT. Eur J Nucl Med Mol Imaging 45, 1772–1780 (2018). https://doi.org/10.1007/s00259-018-4018-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-018-4018-z