Abstract
Background
The oncologic feasibility of video-assisted thoracoscopic (VATS) radical esophagectomy for esophageal cancer has yet to be proven. We evaluated the oncologic outcome of VATS-esophagectomy by reviewing our 10-year experience, with particular emphasis on the effect of lymph node dissection.
Methods
From January 2003 to December 2012, 146 patients with esophageal cancer underwent completion of VATS-esophagectomy in the left lateral position.
Results
The mean follow-up period was 37.1 months. Forty-six patients (31.5 %) had recurrence of cancer. Primary recurrence was hematogenous, lymphatic, peritoneal dissemination, pleural dissemination, locoregional, or port site in 20 (13.7 %), 23 (15.8 %), 2 (1.4 %), 5 (3.4 %), 4 (2.7 %), and 1 (0.67 %) patients, respectively. Pleural dissemination occurred more frequently after noncurative operation than curative operation (p = 0.010). The frequency of lymphatic metastasis within the mediastinal regional lymph nodes in the dissection field was only 5.5 %. The overall 5-year survival rate of stage I, II, and III disease after curative VATS-esophagectomy was 79.1, 77.9, and 56.7 %, respectively. T4 tumor, lymph node metastasis, R1 or 2, and concomitant lymph node metastasis in the cervical, mediastinal, and abdominal fields were indicators of unfavorable outcome. The lymph nodes in the abdominal region and those around the bilateral recurrent laryngeal nerves (RLNs) were frequent metastasis sites. Patients who had metastasis only around RLNs had favorable survival comparable to node-negative cases after curative VATS-esophagectomy.
Conclusions
Video-assisted thorascopic-esophagectomy has an excellent locoregional control effect with favorable oncologic outcome. The lymph node dissection procedure by VATS-esophagectomy has survival benefit for the patients having lymph node metastasis around bilateral RLNs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical resection is the primary therapy for local and locoregional disease in esophageal cancer. Esophagectomy with extended lymphadenectomy was recognized as a standard procedure in the treatment of esophageal cancer in Japan [1–3]. Video-assisted thoracoscopic (VATS) radical esophagectomy (VATS-esophagectomy) is a minimally invasive technique in the management of esophageal cancer. This procedure was developed to reduce the surgical insult in esophageal cancer treatment. Recently, VATS-esophagectomy was reported to be a safe procedure with low mortality and morbidity [4–6]. Meta-analysis showed that VATS-esophagectomy is a safe alternative to open surgery with less pulmonary morbidity [7]. The primary results of a prospective, multi-center, randomized trial showed the short-term benefits of minimally invasive esophagectomy compared with open esophagectomy [8]. Although the efficacy of VATS-esophagectomy with radical lymphadenectomy remains to be proven by a prospective randomized study, some reports have shown comparable results of VATS-esophagectomy and open esophagectomy by retrospective study [9–11]. We introduced VATS-esophagectomy with the patient in the left lateral position for the treatment of esophageal cancer in January 2003. The surgeons in our institution acquired the basic skill of performing VATS-esophagectomy by direct instruction from an experienced surgeon [12]. We have performed VATS-esophagectomy on all patients with resectable esophageal cancer as our standard curative operative procedure from then on [13]. The aim of the present study was to estimate the oncologic outcomes after VATS-esophagectomy by reviewing our 10-year experience. Especially, we analyzed the therapeutic effect of thoracoscopic lymph node dissection in each station by investigating the distribution of lymph node metastasis and the prognostic outcome after surgery.
Materials and methods
Preoperative assessment of tumors
Conventional staging modalities included esophagography, esophagoscopy with biopsy, and computed tomography of the neck, chest, and abdomen. Positron emission tomography has been performed as a routine examination since 2007. Magnetic resonance imaging and bronchofiberscopy were additionally performed if tumor invasion to the adjacent organ was suspected.
Patients
At Kanazawa University, we started to perform VATS-esophagectomy for esophageal cancer in 2003. We modified the indication for VATS-esophagectomy as we gained surgical skills and experience (Fig. 1). We initially limited VATS-esophagectomy to T1 and T2 tumors without lymph node metastasis. After attaining surgical skills from our experience with the initial six cases, we enlarged the criteria to include T3 tumors with regional lymph node metastasis, beginning in April 2004. Initially, patients who had pathologically positive lymph node metastasis underwent adjuvant chemotherapy with a combination of cisplatin and 5-fluorouracil. From January 2008, we have performed neoadjuvant chemotherapy consisting of cisplatin and 5-fluorouracil for stage II and III tumors. Furthermore, we expanded the criteria for VATS-esophagectomy to T4 tumors that were considered to be technically resectable after induction chemotherapy from August 2008. Initially, intrathoracic anastomosis by jejunal conduit was a contraindication of VATS-esophagectomy. From November 2009, we performed VATS-esophagectomy and subsequent thoracoscopic intrathoracic esophagojejunal anastomosis in patients who had previously undergone gastrectomy or who needed to undergo total gastrectomy because they had simultaneous gastric cancer. The criteria for VATS-esophagectomy also included the patient’s condition as follows: no previous radiation therapy; pulmonary function capable of sustaining single-lung ventilation; no concomitant serious medical condition such as liver cirrhosis, heart failure, or renal failure; and patient preference for VATS-esophagectomy. Initially, the abdominal procedure was performed by conventional laparotomy until the learning curve of the thoracoscopic procedure reached a plateau. After that, we performed hand-assisted laparoscopic surgery instead of laparotomy for patients without apparent abdominal lymph node metastasis, concomitant abdominal malignancy, or previous upper abdominal operations. Patients underwent three-field lymph node dissection including cervical, thoracic, and abdominal lymph nodes. Cervical lymph node dissection was omitted in the cases with T1 tumor in the lower thoracic esophagus, serious medical conditions, and suspicion of R1 resection. Patients with R1 and R2 resection underwent postoperative chemoradiotherapy.
Flow chart of esophagus cancer patients who underwent surgery from January 2003 to December 2012. We performed esophagectomy in a total of 176 patients with thoracic esophageal cancer. We modified the indication for VATS radical esophagectomy during this period as the surgeons acquired surgical skill. A total of 24 patients were estimated as not being eligible for VATS-esophagectomy, and 152 patients underwent VATS-esophagectomy. IC induction chemotherapy
Surgical procedure
All patients underwent esophagectomy and reconstruction as described previously [12]. During the thoracic procedure, patients were placed in the left lateral position. Initially, a 5 cm minithoracotomy was created and four 12 mm trocars were inserted around the minithoracotomy as described by Osugi et al. [14]. Recently, we have performed VATS-esophagectomy with six ports without minithoracotomy by using a two-component retractor (Endo HI Retractor, Sonne, Tokyo, Japan), which was inserted from a port and docked in the thoracic cavity to be a 3 cm-width. The right lung was deflated and the mediastinal lymph nodes were carefully dissected to expose the bilateral recurrent laryngeal nerves (RLNs), the aortic wall, the left mediastinal pleura, the pericardium, the membranous portion of the tracheobronchus, and the diaphragm, just as these steps are performed in open surgery. Especially, exhaustive upper mediastinal dissection was performed paying special attention to dissecting the lymph nodes around the bilateral RLNs. The lymph nodes around the right RLN were located on the dorsal side of the nerve, whereas those along the left RLN are situated on the ventral side of the left RLN. To dissect the left RLN lymph nodes, the trachea was rotated with a trachea retractor and the left RLN lymph nodes were dissected to expose the left side of the trachea (Fig. 2). The subaortic lymph nodes around the initial segment of the left RLN were dissected to expose the dorsal side of the left pulmonary artery. The dissection was accomplished using scissors that could be used for unipolar cautery. The usage of electric cautery around RLNs was limited to prevent damage to the nerves. The lymph nodes around the cervical RLNs caudal to the thyroid gland were additionally dissected in the cervical procedure. Abdominal and supraclavicular cervical lymph node dissection was done simultaneously by dividing the thoracic surgical team into two teams, with the patient in the supine position. The gastric tube was selected as the primary reconstruction conduit, and was pulled up through the posterior mediastinum. The operation was finished with cervical anastomosis. In cases of non-curative resection, the retrosternal route was selected for elevation of the gastric tube in order to allow subsequent chemoradiotherapy of the residual tumor. The small or large intestinal conduit was used in patients who had previously undergone gastrectomy or who needed to undergo total gastrectomy because of simultaneous gastric cancer. Reconstruction with the right hemicolon was done through the anterior sternal route. In the case of intrathoracic anastomosis by gastric or jejunal conduit, the operation was started with the abdominal procedure, followed by thoracic dissection and intrathoracic anastomosis. Reconstruction with a pedicled jejunal conduit was done by the Roux-en-Y method without vascular reconstruction. All of the operations were done or were directed by one of the authors (I.N.).
Schematic diagram of the lymph node dissection procedure around the left recurrent laryngeal nerve. After transection of the tracheoesophageal ligament, the esophagus was pulled dorsally by the operator (a). With trachea rotation by the assistant with a trachea retractor, the lymph nodes situated ventral to the left recurrent laryngeal nerve could be dissected (b). Bold arrow indicates the direction of esophageal traction. The arrow with dashed line indicates the dissection line. The bold arrow with dashed line indicates the direction of trachea rotation. E esophagus, R retractor, T trachea, LCA left common carotid artery, LN lymph node, LRN left recurrent nerve, LSA left subclavian artery
Data analysis
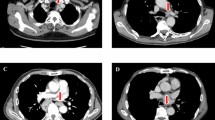
The tumor was staged according to the TNM classification of the American Joint Committee on Cancer and the Union Internationale Contra le Cancer, 7th Edition. The histological types of tumors were classified according to the WHO classification of tumours of the digestive system, 4th Edition. The dissected lymph nodes were classified into three fields: cervical, mediastinal, and abdominal. The mediastinal lymph node field was subdivided into three stations: RLN, paraesophageal, and subcarinal nodes (Fig. 3). Fisher’s exact test was used to compare categorical variables. Survival curves according to the TNM classification were estimated by the Kaplan–Meier method, and the significance of differences between the groups was assessed with the log rank test. A p value <0.05 was considered to be statistically significant. All analyses were done with IBM SPSS [IBM Statistics ver. 19 (IBM, Armonk, NY, USA)].
Classification and naming of regional lymph node stations in the mediastinum. Recurrent laryngeal nerve (RLN) nodes: the thoracic paratracheal, and left tracheobronchial lymph nodes along the bilateral RLN; subcarinal nodes: lymph nodes located in the caudal area of the carina of the trachea and the bilateral main bronchus; paraesophageal nodes: thoracic paraesophageal lymph nodes. AO aorta, DI diaphragm, E esophagus, P pericardium, RSA right subclavian artery, RRN right recurrent nerve, LRN left recurrent nerve, LPP left parietal pleura
Results
From January 2003 to December 2012, a total of 176 patients with esophageal cancer underwent esophagectomy at Kanazawa University. The indication for VATS-esophagectomy differed over the 10-year period as the surgical team gained experience and skill performing VATS-esophagectomy. The numbers of patients who were candidates or who had contraindication for VATS-esophagectomy in each period are shown in Fig. 1. In total, 24 patients were estimated as not being eligible for VATS-esophagectomy and 152 patients underwent VATS-esophagectomy. The VATS-esophagectomy was converted to conventional thoracotomy in 6 patients. The reasons for operative conversion were as follows: pleural adhesions in 1, aortic injury in 1, intrathoracic anastomosis in 1, and contiguous tumor spread in 3. Therefore, we could complete VATS-esophagectomy in 146 patients. The demographics and details of the surgical procedure in the 146 patients in whom VATS-esophagectomy was completed are shown in Table 1.
From August 2008, we performed induction chemotherapy and subsequent VATS-esophagectomy for T4 tumors. From August 2008 to December 2012, we made the clinical diagnosis of T4 disease in 26 patients. Among them, we performed induction chemotherapy in 20 cases. The other six patients had contraindications to surgery due to their general status, and they received chemoradiation, radiation, or palliative therapy. After induction chemotherapy, the tumors in 14 (70 %) of the 20 patients became resectable as a consequence of tumor regression, and the 14 patients underwent subsequent VATS-esophagectomy. All T4 tumors could be resected without organ injury or conversion to thoracotomy. Postoperative examination showed that 7 of the 14 resected cases after induction chemotherapy were pathologically T4. In addition, seven patients were found intraoperatively to have T4 tumors. Therefore, we carried out VATS-esophagectomy in 14 pathologically T4 patients. The organ into which the T4 tumor had spread and the degree of residual tumor (R) in the 14 pathologically T4 patients are presented in Table 2. Among the 14 pathologically T4 patients, seven patients had been diagnosed preoperatively with clinical T4 tumor and underwent induction chemotherapy. Co-resection of the involved organ could be performed only for the diaphragm or for pleural involvement. We were able to achieve R0 or R1 resection in all seven patients who underwent induction chemotherapy.
The mean duration of the thoracic procedure and that of the entire procedure in the 146 VATS-esophagectomy-completed cases were 287 ± 81 (SD) and 624 ± 129 min, respectively (Table 3). Mean blood loss during the thoracic procedure and that during the entire procedure was 250 ± 190 and 591 ± 523 g, respectively. Blood transfusion was performed in 26 (17.8 %) of the 146 operations. The mean number of dissected lymph nodes in the thoracic procedure was 33.3 ± 13.7. The incidence of mortality and morbidity is given in Table 4. One patient (0.68 %) died within 30 days after surgery; this patient died of postoperative acute respiratory distress syndrome (ARDS). There were 4 in-hospital deaths (2.7 %), among them, 2 patients (1.4 %) who died of ARDS. The other two patients (1.4 %) with noncurative resection died of tumor progression.
The most frequent complication was RLN palsy. Unilateral or bilateral RLN palsy was seen in 34 (23.3 %) and 22 (15.1 %) of the 146 patients, respectively. Tracheotomy was performed in 12 patients (8.2 %), and in two of them the tracheotomy was permanent. Almost all cases of RLN palsy were transient and resolved within 3 months. However, five patients including three patients in whom the RLN was transected, developed permanent nerve palsy. Pneumonia and atelectasis developed in 31 patients (21.2 %). The mean follow-up period was 37.1 months. Within this period, 46 patients (31.5 %) had recurrence of cancer, and 25 patients (17.1 %) died of cancer. The primary detectable recurrent sites are listed in Table 5. The recurrence rate after noncurative operation (R1 or 2) was significantly higher than that after curative resection (p = 0.008). Pleural dissemination occurred more frequently after noncurative operation than after curative operation (p = 0.010). Lymphatic metastasis showed the highest recurrence rate after operation and was found in 15.8 % of the patients. However, the frequency of lymphatic metastasis within the mediastinal regional lymph nodes in the dissection field was only 5.5 %. In addition, locoregional recurrence was found in only 2.7 %.
Overall survival curves according to the depth of tumor invasion (pT), the lymph node metastasis status (pN), the residual tumor (R), and pathological stage (pStage) are shown in Fig. 4. The patients with T4 tumor, R1 or R2 operation, and lymph node metastasis had poor prognosis. Patients who had more than seven lymph node metastases (pN3) had poor prognosis. The patients with pT2 or pStage II cancer showed quite favorable outcome, consistent with early-stage patients. The prognosis according to the distribution of metastatic lymph nodes was analyzed in the 130 patients who underwent curative operations (Fig. 5a). The patients who had metastases in all three fields (cervical, mediastinal, and abdominal fields) showed unfavorable prognosis. The metastasis rate and the impact of dissection in each lymph node station in 130 curative operations were analyzed (Table 6; Fig. 5). Lymph nodes in the abdominal region and those around the bilateral RLN were frequent metastatic sites. The overall survival curves after the curative dissection procedure demonstrated that the patients who had metastasis only around RLNs had favorable survival, similar to that of node-negative cases (Fig. 5b).
Overall survival curves of patients who underwent thoracoscopic esophagectomy according to tumor depth of invasion (pT) (a), lymph node status (pN) (b, c), and pathological stage (pStage) with residual tumor (R) classification (d). pT4 vs. pT1: p = 0.002, pT4 vs. pT2: p = 0.026, pN0 vs. pN1–3: p = 0.001, pN0 vs. pN1: p = 0.015, pN0 vs. pN3: p < 0.001, pStage I R0 vs. pStage III R0: p = 0.015, pStageI, II, III R0, vs. pStage III or IV and R1 or 2: p < 0.001, p < 0.001, p = 0.007, respectively, by log rank test
Overall survival curves after curative thoracoscopic esophagectomy according to the distribution of metastatic lymph nodes in the respective field (a) and mediastinal lymph node station (b, c). The regional lymph nodes were classified into three fields: cervical, mediastinal, and abdominal. Mediastinal and abdominal metastasis indicated that metastasis was localized to the respective field. Two-field metastasis indicated that metastasis was found in two of three fields. Three-field metastasis indicated that metastasis was found in all three fields. The mediastinal lymph node field was subdivided into three stations: RLN, paraesophageal, and subcarinal nodes. The overall survival of patients showing metastasis in the limited lymph node station was compared with that of patients without lymph node metastasis. pN-RLN lymph node metastasis found only in RLN nodes; pN-Paraeso lymph node metastasis found only in paraesophageal nodes. pN0 vs. three-field metastasis: p = 0.0000, pN0 vs. pN-RLN: p = 0.669, pN0 vs. pN-Paraeso: p = 0.001, respectively, by log rank test
Discussion
In this study, we report the favorable oncologic outcome of thoracoscopic esophagectomy with extended lymph node dissection in the left lateral position by reviewing our 10-year experience. Favorable oncologic outcome was observed after VATS-esophagectomy not only for early-stage cancer but also for advanced-stage disease. T4 tumor, lymph node metastasis, R1 or R2, or concomitant lymph node metastasis in the cervical, mediastinal, and abdominal fields were the indicators of unfavorable outcome. Lymph node metastasis around the bilateral RLNs was observed at high frequency. The lymph node dissection procedure in VATS-esophagectomy had survival benefit for patients having lymph node metastasis only around RLNs, comparable to the survival of node-negative cases.
In the thoracic procedure, we skeletonized the entire mediastinum to remove all posterior mediastinal regional lymph nodes under the magnified view through the thoracoscope. As a result of the exhaustive dissection procedure, local recurrence and mediastinal regional lymph node recurrence were found in only 4 (2.7 %) and 8 (5.5 %) cases, respectively. Especially, the lymph nodes around both RLNs were carefully dissected because of a high frequency of tumor dissemination to lymph nodes along the RLNs and because survival benefit of extended lymphadenectomy for patients with lymph node metastasis along the RLNs has been reported [1, 3]. In the present study, we analyzed the distribution of lymph node metastasis, metastatic rate, and the impact of dissection against oncologic outcome in each lymph node station. Because residual tumor (R) was a strong prognostic factor, we excluded the cases with noncurative operation to analyze the impact of lymph node dissection. The patients with lymph node metastasis had a poorer prognosis than the node-negative patients.
Concomitant lymph node metastasis in the cervical, mediastinal, and abdominal fields was also an indicator of poor survival. Lymph node metastasis was frequently seen in the lymph node station around both RLNs. It is noteworthy that the prognosis of the patients who had metastasis only around RLNs was similar to the prognosis of the node-negative patients after curative operation, even though the former group carried advanced cancer. Our dissection procedure around the RLNs was effective not only for regional control but also for survival benefit. Furthermore, the patients with pT2 or pStage II showed quite favorable outcome consistent with early-stage patients. The majority of esophageal cancers in pStage II might be a localized disease controllable by thoracoscopic surgery. The survival results of patients with each stage in the present study were favorable in comparison with those in previous reports of minimally invasive esophagectomy [6], as well as the results reported by the Comprehensive Registry of Esophageal Cancer in Japan of 2003 [15]. The dissection procedure in VATS-esophagectomy may be able to be performed during open thoracotomy. However, meticulous and exhaustive dissection was possible under the magnified view of the scope in thoracoscopic surgery rather than open thoracotomy in the deep mediastinum.
From 2008, we introduced preoperative chemotherapy for stage II and III disease, because a Japanese randomized clinical trial (JCOG9907) showed the superior survival benefit of preoperative chemotherapy against postoperative chemotherapy for localized advanced esophageal cancers [16]. Although the survival after preoperative chemotherapy and subsequent VATS-esophagectomy seems to be favorable in comparison with that with VATS-esophagectomy and postoperative chemotherapy, the survival difference between these two groups did not reach statistical significance (data not shown). Also, the short observation period of the patients who underwent preoperative chemotherapy might have affected the result. To prove the survival benefit of preoperative chemotherapy for patients who undergo VATS-esophagectomy, further observation is needed.
Initially, we decided that T4 tumor was a contraindication for the VATS-esophagectomy procedure. Although we excluded tumors that were assessed to be T4 by preoperative examination, we encountered T4 tumors intraoperatively. After the introduction of preoperative induction chemotherapy, the majority of T4 tumors seemed to be resectable by the therapeutic effect. We expanded the indications for VATS-esophagectomy to T4 tumors that were considered to be resectable after remission by preoperative induction chemotherapy. We considered that 14 (70 %) of the 20 T4 patients treated with induction chemotherapy had a resectable tumor and these 14 patients underwent VATS-esophagectomy. In case of excision of diminished tumor after induction chemotherapy, it is sometimes difficult to exfoliate the tumor from the adjacent organ due to fibrotic changes around the tumor bed. Careful attention was paid to avoid injury to adjacent organs. Although we tried to perform R0 resection, we left behind the fibrous tissue around the tumor bed to prevent organ injury in circumstances where strong fibrous adhesion to an adjacent organ was observed. Curative operation was promising in cases where there was a pathological therapeutic effect of induction chemotherapy by post-chemotherapy pathological examination. We could achieve R0 resection by VATS-esophagectomy in the majority of cases without any injury to adjacent organs. As a result, the patients who underwent pathologically curative VATS-esophagectomy had a quite favorable prognosis, regardless of the initial T-category. The patients with R1 and R2 resection of T4 tumors underwent postoperative chemoradiotherapy to prevent local recurrence. The recurrence rate after noncurative operation was higher than that after curative operation. Contrary to expectations, local recurrence was much less common after noncurative resection. However, the rate of pleural dissemination was higher after noncurative than after curative operation. The procedure of breaking the tumor bed might induce cancer cell dissociation to the pleural cavity. Patients should be observed for the possibility of postoperative pleural dissemination after noncurative operation. Indeed, in the present study, the patients with R1 or R2 had a poorer prognosis than those with R0 operations. Because we started to perform VATS-esophagectomy after induction chemotherapy for T4 tumors only recently, we do not have data on 5-year survivors yet. However, the 3-year survival rate of 36.0 % for patients with T4 tumor is quite favorable in comparison to that after surgery alone (9.2 %) [17] or definitive chemoradiotherapy (14 %) [18]. Exhaustive debulking surgery by VATS-esophagectomy and subsequent postoperative chemoradiotherapy might improve patient outcomes. It might be worthwhile to try VATS-esophagectomy in combination with induction chemotherapy for T4 tumors.
In the present series, the average total blood loss was 591 g. Only 26 (17.8 %) of the 146 VATS-esophagectomy-completed cases received blood transfusion. Precise dissection under the magnified view contributed to less blood loss, and was helpful in avoiding blood transfusion. Pulmonary complications were found in 31 (21.2 %) of the 146 cases, with the development of ARDS in seven patients (4.8 %). The incidence of pulmonary complication in our study was comparable to that in previous studies (7–36 %) [11, 19, 20]. A characteristic of our surgical morbidity was frequent postoperative RLN palsy. The relatively high pneumonia rate might have resulted from the aspiration related to RLN palsy. The rate of RLN palsy after VATS-esophagectomy has been reported to range from 7 to 14.3 % [4, 21–23]. The RLN palsy was transient and recovered within 3 months of operation in most cases. The use of monopolar electrocautery around RLNs might induce the nerve palsy. Further attention should be paid to manage bleeding around RLNs, with limited use of an electric device. Despite the high morbidity rate, the 1.4 % hospital mortality rate without recurrence was acceptable in comparison to the rates in recent reports of VATS-esophagectomy that ranged from 1 to 1.7 % [6, 22, 24]. VATS-esophagectomy accompanied by extended lymphadenectomy is tolerable for most patients.
Our standard reconstruction procedure was cervical esophagogastrostomy. We performed intrathoracic esophagojejunal anastomosis for patients who had previously undergone gastrectomy or who needed to undergo total gastrectomy because of simultaneous gastric cancer. Initially, intrathoracic esophagojejunal anastomosis was a contraindication for thoracoscopic surgery. From November 2009, we performed VATS-esophagectomy and subsequent thoracoscopic intrathoracic esophagojejunal anastomosis. By using our experience with thoracoscopic esophagojejunostomy, we had begun treating patients who were not candidates for cervical dissection with thoracoscopic esophagogastrostomy. We had to enlarge the mini-thoracotomy in the second case of thoracoscopic esophagogastrostomy, because of difficulty in inserting the circular stapler through the narrow intercostal space. We resolved the anastomotic problem by modifying the anastomosis technique to insert the circular stapler from the esophageal hiatus via laparotomy.
Thoracoscopic surgery is complex. Initially, we limited the indication of VATS-esophagectomy to T1 and T2 tumors without lymph node metastasis. After our initial experience with six cases, we expanded the indication to more advanced disease. However, expansion of the indication resulted in an increase in the rate of conversion to thoracotomy. Further attainment of surgical skill and anatomical knowledge overcame this problem. The challenging procedure of VATS-esophagectomy including operation for T4 tumors after induction chemotherapy and intra-thoracic anastomosis might demand further surgical skills and experience, which can be obtained performing a substantial number of operations.
Although VATS-esophagectomy with extensive mediastinal lymphadenectomy is associated with a certain degree of morbidity, including RLN palsy and pulmonary complications, this procedure has an excellent locoregional control effect. In addition, the favorable survival of patients who have undergone VATS-esophagectomy shows that the technique is oncologically feasible. The lymph nodes around bilateral RLNs are key nodes showing high metastatic rate. Thoracoscopic dissection around bilateral RLNs provides a powerful surgical tool with favorable survival benefit. Furthermore, VATS-esophagectomy might also be an effective treatment for locally advanced T4 tumor as a curative therapeutic modality, particularly when pathological curative dissection is combined with induction chemotherapy. In cases where T4 tumor is diagnosed during surgery, meticulous dissection by VATS-esophagectomy and subsequent chemoradiotherapy might help local control after non-curative resection. To confirm the usefulness of VATS-esophagectomy, phase II and III trials are needed.
References
Akiyama H, Tsurumaru M, Udagawa H et al (1994) Radical lymph node dissection for cancer of the thoracic esophagus. Ann Surg 220:364–372 discussion 372–373
Fujita H, Kakegawa T, Yamana H et al (1995) Mortality and morbidity rates, postoperative course, quality of life, and prognosis after extended radical lymphadenectomy for esophageal cancer. Comparison of three-field lymphadenectomy with two-field lymphadenectomy. Ann Surg 222:654–662
Udagawa H, Ueno M, Shinohara H et al (2012) The importance of grouping of lymph node stations and rationale of three-field lymphoadenectomy for thoracic esophageal cancer. J Surg Oncol 106:742–747
Schoppmann SF, Prager G, Langer FB et al (2010) Open versus minimally invasive esophagectomy: a single-center case controlled study. Surg Endosc 24:3044–3053
Sundaram A, Geronimo JC, Willer BL et al (2012) Survival and quality of life after minimally invasive esophagectomy: a single-surgeon experience. Surg Endosc 26:168–176
Luketich JD, Pennathur A, Awais O et al (2012) Outcomes after minimally invasive esophagectomy: review of over 1,000 patients. Ann Surg 256:95–103
Nagpal K, Ahmed K, Vats A et al (2010) Is minimally invasive surgery beneficial in the management of esophageal cancer? A meta-analysis. Surg Endosc 24:1621–1629
Biere SS, van Berge Henegouwen MI, Maas KW et al (2012) Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet 379:1887–1892
Osugi H, Takemura M, Higashino M et al (2003) A comparison of video-assisted thoracoscopic oesophagectomy and radical lymph node dissection for squamous cell cancer of the oesophagus with open operation. Br J Surg 90:108–113
Shen Y, Zhang Y, Tan L et al (2012) Extensive mediastinal lymphadenectomy during minimally invasive esophagectomy: optimal results from a single center. J Gastrointest Surg 16:715–721
Kinjo Y, Kurita N, Nakamura F et al (2012) Effectiveness of combined thoracoscopic-laparoscopic esophagectomy: comparison of postoperative complications and midterm oncological outcomes in patients with esophageal cancer. Surg Endosc 26:381–390
Ninomiya I, Osugi H, Fujimura T et al (2008) Results of video-assisted thoracoscopic surgery for esophageal cancer during the induction period. Gen Thorac Cardiovasc Surg 56:119–125
Ninomiya I, Osugi H, Tomizawa N et al (2010) Learning of thoracoscopic radical esophagectomy: how can the learning curve be made short and flat? Dis Esophagus 23:618–626
Osugi H, Takemura M, Higashino M et al (2002) Video-assisted thoracoscopic esophagectomy and radical lymph node dissection for esophageal cancer. A series of 75 cases. Surg Endosc 16:1588–1593
Ozawa S, Tachimori Y, Baba H et al (2011) Comprehensive registry of esophageal cancer in Japan, 2003. Esophagus 8:9–29
Ando N, Kato H, Igaki H et al (2012) A randomized trial comparing postoperative adjuvant chemotherapy with cisplatin and 5-fluorouracil versus preoperative chemotherapy for localized advanced squamous cell carcinoma of the thoracic esophagus (JCOG9907). Ann Surg Oncol 19:68–74
Kosugi S, Ichikawa H, Kanda T et al (2012) Clinicopathological characteristics and prognosis of patients with esophageal carcinoma invading adjacent structures found during esophagectomy. J Surg Oncol 105:767–772
Ohtsu A, Boku N, Muro K et al (1999) Definitive chemoradiotherapy for T4 and/or M1 lymph node squamous cell carcinoma of the esophagus. J Clin Oncol 17:2915–2921
Osugi H, Takemura M, Takada N et al (2002) Prognostic factors after oesophagectomy and extended lymphadenectomy for squamous oesophageal cancer. Br J Surg 89:909–913
Bakhos CT, Fabian T, Oyasiji TO et al (2012) Impact of the surgical technique on pulmonary morbidity after esophagectomy. Ann Thorac Surg 93:221–226 discussion 226–227
Osugi H, Takemura M, Higashino M et al (2003) Learning curve of video-assisted thoracoscopic esophagectomy and extensive lymphadenectomy for squamous cell cancer of the thoracic esophagus and results. Surg Endosc 17:515–519
Noshiro H, Nagai E, Shimizu S et al (2007) Minimally invasive radical esophagectomy for esophageal cancer. Esophagus 4:59–65
Ben-David K, Sarosi GA, Cendan JC et al (2012) Decreasing morbidity and mortality in 100 consecutive minimally invasive esophagectomies. Surg Endosc 26:162–167
Palanivelu C, Prakash A, Senthilkumar R et al (2006) Minimally invasive esophagectomy: thoracoscopic mobilization of the esophagus and mediastinal lymphadenectomy in prone position—experience of 130 patients. J Am Coll Surg 203:7–16
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was orally presented at an ISW 2013 as Grassi Prize Presentation.
Rights and permissions
About this article
Cite this article
Ninomiya, I., Okamoto, K., Fujimura, T. et al. Oncologic Outcomes of Thoracoscopic Esophagectomy with Extended Lymph Node Dissection: 10-year Experience from a Single Center. World J Surg 38, 120–130 (2014). https://doi.org/10.1007/s00268-013-2238-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-013-2238-8