Abstract
Background
Esophageal achalasia is characterized by the absence of esophageal peristalsis and by a dysfunctional lower esophageal sphincter (LES). Descriptions of clinical, radiological, and manometric findings in patients with achalasia usually have been based on small numbers of patients. This study was designed to determine in patients with untreated achalasia: (1) clinical presentation; (2) how often a diagnosis of gastroesophageal reflux disease (GERD) was erroneously made based on the presence of heartburn; (3) manometric profile; (4) relationship between chest pain and the manometric finding of vigorous achalasia.
Methods
Between 1990 and 2004, a diagnosis of esophageal achalasia was established in 145 patients. None of them had been previously treated (no previous endoscopic or surgical treatment). We evaluated the demographic and clinical characteristics, as well as the results of the endoscopy, barium swallow, esophageal manometry, and ambulatory pH monitoring. We also compared the clinical and the manometric profile of patients with classic and patients with vigorous achalasia.
Results
Most patients with untreated achalasia had dysphagia (94%). Regurgitation was present in 76% and heartburn in 52%. Chest pain (41%) and weight loss (35%) were less common. Acid-suppressing medications had been prescribed to 65 patients (45%) who complained of heartburn on the assumption that GERD was present. The LES was hypertensive in 43% of patients only. There was no significant difference in the prevalence, severity, and duration of chest pain in patients with classic and with vigorous achalasia.
Conclusions
These results show that in patients with untreated achalasia: (1) dysphagia was the most frequent complaint, but regurgitation and heartburn were frequently present; (2) a diagnosis of GERD based on the presence of heartburn was highly unreliable; (3) the LES was hypertensive in less than half of patients; and (4) the prevalence, severity, and duration of chest pain did not correlate with the manometric finding of vigorous achalasia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Esophageal achalasia is a primary esophageal motility disorder that is commonly defined by lack of peristalsis and the presence of a hypertensive lower esophageal sphincter (LES) that fails to relax in response to swallowing [1]. Vigorous achalasia is thought to be an earlier stage of the disease, typical of young patients who have been symptomatic for a short time, and characterized by high amplitude of the simultaneous, nonperistaltic contractions (≥37 mmHg) and high incidence of chest pain [2, 3]. These high amplitude, nonperistaltic contractions would represent an initial attempt by the esophageal body to overcome the functional obstruction caused by the LES. Existing descriptions of clinical and manometric findings in patients with classic and vigorous achalasia have shown that dysphagia is present almost uniformly [4]. However, it is still unclear whether chest pain is more common in patients with vigorous achalasia. In addition, it is not known how often the presence of heartburn erroneously leads to the prescription of acid-suppressing medications on the assumption that gastroesophageal reflux disease (GERD) is present.
The goal of this study was to determine in patients with untreated achalasia: (1) clinical presentation; (2) how often a diagnosis of GERD was made based on the presence of heartburn; (3) manometric profile of the LES; and 4) relationship between the presence, severity, and duration of chest pain and the manometric finding of vigorous achalasia.
Patients and methods
Between 1990 and 2004, esophageal achalasia was diagnosed in 145 consecutive patients who had no previous endoscopic (dilatation, botulinum toxin injection, or both) or surgical treatment at the time of their evaluation. Among the 145 patients, 77 were men and 68 were women. The mean age was 49 (range, 14–86) years. The median duration of symptoms was 57 (range, 1–480) months. Patients were asked whether they were taking acid-suppressing medications because their primary physician had assumed that heartburn was caused by GERD. The diagnosis of achalasia was based on the following evaluation.
Symptomatic evaluation
Patients were asked to score the severity of dysphagia, regurgitation, heartburn, and chest pain using a 5-point scale ranging from 0 (no symptom) to 4 (disabling symptom). The duration of symptoms and eventual weight loss also were recorded. Body mass index (BMI; kg/m2) was calculated for each patient.
Upper gastrointestinal series
The degree of esophageal dilatation was assessed by measuring the maximal esophageal width on a posteroanterior projection esophagogram using film Lite software (Merge eMed, Division of Merge Healthcare, Milwaukee, WI). The shape of the esophagus (straight or sigmoid) and the presence of a hiatal hernia were recorded.
Endoscopy
Upper endoscopy was performed in selected patients to rule out the presence of esophagitis or a peptic or neoplastic stricture of the distal esophagus.
Esophageal manometry
Medications that interfere with esophageal motility (calcium channel blockers, nitrates) were discontinued 3 days before the study. Patients were studied after an overnight fast by using an 8-lumen manometry catheter continuously perfused by a pneumohydraulic capillary infusion system connected to a polygraph, as previously described [5]. Position, pressure, length, and relaxation of the LES were measured by using the station pull-through technique (normal LES pressure, 14–24 mmHg). LES relaxation in response to swallowing was classified as complete when the LES pressure decreased to the gastric baseline pressure, absent when it did not change, and incomplete when it decreased but failed to reach the baseline completely. Esophageal body function was assessed by giving 10 wet swallows of 5 ml of water at 30-s intervals. The velocity and amplitude of the contractions were analyzed in the proximal (PEA; 13 and 18 cm above the LES) and the distal esophagus (DEA; 3 and 8 cm above the LES). Achalasia was defined manometrically by the absence of esophageal peristalsis (simultaneous contractions). Vigorous achalasia was defined by the presence of simultaneous contractions with an amplitude ≥37 mmHg [3].
Ambulatory pH monitoring
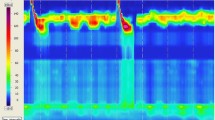
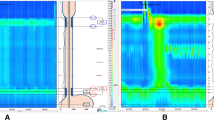
Acid-suppressing medications were discontinued 3 days (H2 blockers) or 14 days (proton pump inhibitors) before the study. The pH sensor was placed 5 cm above the upper border of the manometrically determined LES [5]. In patients with an abnormal DeMeester score (normal < 14.7), tracings were analyzed to distinguish between false reflux and real gastroesophageal reflux (Fig. 1) [6, 7].
Statistical analysis
An analysis of variance and Student’s t test were used for the statistical evaluation of data. Data are expressed as mean ± SD. Differences were considered significant at p < 0.05.
Results
Clinical profile
At the time of presentation, dysphagia was present in 94% of patients (score: 3.3 ± 0.6); regurgitation in 76% (score: 2.9 ± 0.9); heartburn in 52% (score: 2.4 ± 1.0); and chest pain in 41% (score: 2.7 ± 0.9). Weight loss was reported by 35% of patients. The average BMI was 25 ± 6.5 (range, 15–41). At the time of referral to our center, 95 patients (65%) were taking medications. Specifically, 50 patients were taking proton pump inhibitors, 9 were taking H2 blocking agents, and 6 were taking both, on the assumption that GERD was the cause of the heartburn. The diagnosis of GERD had been made by the referring physician. Poor response and persistence of symptoms despite therapy was the main indication for these patients to be referred for both esophageal manometry and ambulatory pH monitoring. Twenty-three patients were taking calcium channel blockers, 12 were taking nitrates, and 6 were taking both (Table 1).
Radiological profile
A barium esophagogram was available for review in 70 patients (48%; Table 2). In the remaining patients, X-rays were not available for our review, but a report indicating a diagnosis of achalasia was always present. The degree of dilatation was as follows: in 21 patients (30%) the esophageal diameter was <4 cm; in 35 patients (50%) it was between 4 and 6 cm; in 11 patients (16%) it was >6 cm. A sigmoid esophagus was present in three patients (4%). A hiatal hernia was present in five patients (7%).
Endoscopic profile
Endoscopy was performed in 114 patients (79%). Esophageal narrowing or resistance at the gastroesophageal junction suggestive of achalasia was recorded by the endoscopist in 30 patients (26%) only. No patient had Barrett’s esophagus, a peptic stricture, or cancer.
Manometric profile
Every patient underwent esophageal manometry (Table 2). In 118 patients (81%) the catheter was placed by transnasal intubation without problems. In 17 patients (12%) the catheter was placed under fluoroscopic guidance and in 10 patients (7%) by endoscopy. The average LES pressure was 25 ± 14 mmHg. The LES was hypotensive in 25% of patients, normotensive in 32%, and hypertensive in 43%. LES relaxation was complete in 13% of patients, incomplete in 50%, and absent in 37%. All patients had aperistalsis of the esophageal body. The average amplitude in the distal esophagus was 39 ± 27 mmHg. Vigorous achalasia was present in 49 patients (34%).
Ambulatory esophageal pH monitoring
Ambulatory pH monitoring was performed in 54 patients (37%). The DeMeester score was normal in 47 patients (87%) and abnormal in 7 (13%). In these seven patients, the analysis of the pH monitoring tracings showed that the abnormal score was caused by false reflux [6, 7].
Classic and vigorous achalasia: comparison of clinical, radiographic, and manometric findings
Sex, age, duration of symptoms, and weight loss were similar in patients with classic and with vigorous achalasia (Table 3). Ninety-eight percent of patients with classic achalasia complained of dysphagia compared with 86% of patients with vigorous achalasia (p = 0.01). Patients with classic achalasia had more severe regurgitation than patients with vigorous achalasia. There was no difference in the prevalence, severity, and duration of chest pain between patients with classic and patients with vigorous achalasia (Table 3). Endoscopic and radiographic findings also were similar between the two groups. By definition, patients with vigorous achalasia had greater amplitude of contraction in both the proximal (PEA: 46 vs. 22 mmHg; p = 0.001) and distal esophagus (DEA: 67 vs. 21 mmHg; p = 0.001).
Discussion
The results of this study show that in patients with untreated achalasia: (1) dysphagia was the most common complaint, but regurgitation and heartburn were frequently present; (2) patients often were treated with acid suppression medications on the assumption that GERD was present; (3) the LES was hypertensive in less than half of patients; and (4) the prevalence, severity, and duration of chest pain did not correlate with the manometric finding of vigorous achalasia
Heartburn is an unreliable marker of the reflux status
It is commonly believed that a diagnosis of GERD can be made reliably from the clinical history. If a patient has heartburn it is presumed that acid reflux is present, therefore, acid-suppressing medications are prescribed. However, when this strategy has been tested, symptoms have been found to be far less sensitive and specific than usually thought and it has been shown that symptoms alone cannot distinguish patients with and without real GERD [8]. For instance, among 822 patients with a clinical diagnosis of GERD, we found that abnormal reflux was present in 70% only. In addition, among the patients who had a normal reflux profile, a primary esophageal motility disorder, such as achalasia or diffuse esophageal spasm, was present in 18% [8].
Patients with achalasia frequently describe the presence of heartburn. In untreated patients, heartburn is thought to be caused by stasis and fermentation of food in the esophagus secondary to the impaired esophageal emptying, rather than by real gastroesophageal reflux [6, 7]. If a pH monitoring is not performed, there is the risk that some of these patients may be advised to have a fundoplication, because they do not respond well to acid-reducing medications. We believe that the reflux status should be assessed by a pH monitoring test in any patients before surgery. In addition, in patients who have an abnormal score, the tracings should be reviewed to distinguish between real and false reflux [6, 7]. In our study we found that among the patients who were thought to have reflux, the pH monitoring score was abnormal in seven patients only. It was the review of the tracings, however, that showed that there was no real gastroesophageal reflux (Fig. 1). It is important to underline that in some of these patients a pH monitoring probably could have been avoided, because the combination of dysphagia, barium swallow, and esophageal manometry clearly pointed to a diagnosis of achalasia. However, the tests were ordered by the referring physician and performed in our Swallowing Center.
LES in achalasia is hypertensive in less than half of patients
A common misconception is that the LES is hypertensive in all patients with esophageal achalasia [1]. Our findings contradict this general belief, because only 43% of our patients with untreated achalasia had a hypertensive LES. The LES had a normal resting pressure in 47 patients (32%), and it was hypotensive in 36 patients (25%). As expected, the LES failed to relax properly in response to swallowing in most patients. The relaxation appeared complete in a minority of patients only, but it probably represented an artifact caused by the movement of the distal sensors of the manometry catheter in and out of the LES (high-pressure zone) during swallowing [9]. The knowledge that the LES is hypertensive in less than half of patients with achalasia has important clinical implications. Although some authors believe that a preoperative low LES pressure negatively affects the outcome of a laparoscopic myotomy [10], we have found that a preoperative low LES pressure was not associated with a worse outcome [11].
Overall, the diagnosis of achalasia in all patients rested firmly on the presence of dysphagia, the findings of a barium swallow, and the absence of esophageal peristalsis. In addition, in the majority of patients the LES failed to relax appropriately in response to swallowing. In patients with heartburn, the ambulatory pH monitoring excluded the presence of abnormal reflux, which can be the presenting symptoms of patients with connective tissue disorders in whom peristalsis often is absent.
The presence of chest pain and the duration of symptoms do not predict the manometric finding of vigorous achalasia
It has been suggested that chest pain is present early in the course of the disease and that it is caused by high amplitude contractions (vigorous achalasia) [3, 12]. However, the findings of our study contradict this theory. A similar percentage of patients with classic and with vigorous achalasia had chest pain. In addition, there was no difference in severity and duration of chest pain between the two groups. We believe that these patients should all be treated when possible by a laparoscopic Heller myotomy and partial fundoplication because it has been shown that the clinical outcome of this operation is similar for patients with classic achalasia and patients with vigorous achalasia [13, 14].
Conclusion
Our study underlines the importance of a careful evaluation in patients with foregut symptoms before ascribing them to a specific diagnosis and deciding a treatment plan. Specifically, it would avoid costly medical treatment or a wrong operation in patients with achalasia who experience heartburn.
References
Spechler SJ, Castell DO (2001) Classification of oesophageal motility abnormalities. Gut 49:145–151
Eckardt VF, Stauf B, Bernhard G (1999) Chest pain in achalasia: patient characteristics and clinical course. Gastroenterology 116:1300–1304
Sanderson DR, Ellis FH, Schlegel JF, Olsen AM (1967) Syndrome of vigorous achalasia: clinical and physiologic observations. Dis Chest 52:508–517
Podas T, Eaden J, Mayberry M, Mayberry J (1998) Achalasia: a critical review of epidemiological studies. Am J Gastroenterol 93:2345–2347
Patti MG, Feo CV, Arcerito M, De Pinto M, Tamburini A, Diener U, Gantert W, Way LW (1999) Effects of previous treatment on results of laparoscopic Heller myotomy for achalasia. Dig Dis Sci 11:2270–2276
Patti MG, Arcerito M, Tong J, De Pinto M, de Bellis M, Wang A, Feo CV, Mulvihill SJ, Way LW (1997) Importance of preoperative and postoperative pH monitoring in patients with esophageal achalasia. J Gastrointest Surg 1:505–510
Crookes PF, Corkill S, DeMeester TR (1997) Gastroesophageal reflux in achalasia. When is reflux really reflux? Dig Dis Sci 42:1354–1361
Patti MG, Diener U, Tamburini A, Molena D, Way LW (2001) Role of esophageal function tests in diagnosis of gastroesophageal reflux disease. Dig Dis Sci 46:597–602
Katz PO, Richter JE, Cowan R, Castell DO (1986) Apparent complete lower esophageal sphincter relaxation in achalasia. Gastroenterology 90:978–983
Arain MA, Peters JH, Tamhankar AP, Portale G, Almongy G, DeMeester SR, Crookes PF, Hagen JA, Bremner CG, DeMeester TR (2004) Preoperative lower esophageal sphincter pressure affects the outcome of laparoscopic esophageal myotomy for achalasia. J Gastrointest Surg 8:328–334
Gorodner MV, Galvani C, Fisichella PM, Patti MG (2004) Preoperative lower esophageal sphincter pressure has little influence on the outcome of laparoscopic Heller myotomy for achalasia. Surg Endosc 18:774–778
Bondi JL, Godwin DH, Garrett JM (1972) “Vigorous” achalasia. Its clinical interpretation and significance. Am J Gastroenterol 58:145–155
Perretta S, Fisichella PM, Galvani C, Gorodner MV, Way LW, Patti MG (2003) Achalasia and chest pain: effect of laparoscopic Heller myotomy. J Gastrointest Surg 7:595–598
Patti MG, Galvani C, Gorodner MV, Tedesco P (2005) Timing of surgical intervention does not influence return of esophageal peristalsis or outcome for patients with achalasia. Surg Endosc 19:1188–1192
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fisichella, P.M., Raz, D., Palazzo, F. et al. Clinical, Radiological, and Manometric Profile in 145 Patients with Untreated Achalasia. World J Surg 32, 1974–1979 (2008). https://doi.org/10.1007/s00268-008-9656-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-008-9656-z