Abstract
Background
It is believed that in untreated patients with achalasia, the lower esophageal sphincter (LES) is almost always hypertensive and a Heller myotomy resolves symptoms by decreasing the LES pressure. The incidence of a normal or hypotensive LES in untreated achalasia patients is unknown. The goals of this study were to determine the incidence of a normal or hypotensive LES in untreated achalasia patients and the outcome of laparoscopic Heller myotomy in achalasia patients with either normal or low LES pressure.
Methods
Between January 1990 and May 2002, a diagnosis of achalasia was made in 239 patients. Among 109 patients (46%) who had not previously received any form of treatment, 53 patients underwent laparoscopic Heller myotomy and Dor fundoplication. Based on the preoperative LES pressure (normal, 14–24 mmHg) they were divided into three groups: group A—four patients (7.5%), LES pressure <14 mmHg; group B—18 patients (34%), LES pressure 14–24 mmHg; and group C—31 patients (58.5%), LES pressure >24 mmHg.
Results
Among the 109 untreated patients, the LES was hypertensive in 49 patients (45%), normal in 29 patients (27%), and hypotensive in 31 patients (28%). The clinical outcome was good among the three groups of patients who underwent laparoscopic Heller myotomy, with poor outcome in only approximately 10% in each group.
Conclusions
These data show that in 55% of untreated. achalasia patients the LES pressure is either normal or low, and that laparoscopic Heller myotomy usually relieves symptoms regardless of preoperative LES pressure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Esophageal achalasia is a primary esophageal motility disorder of unknown etiology characterized by the presence of dysphagia and regurgitation. This disorder is traditionally defined on esophageal manometry by the absence of esophageal peristalsis and by the presence of a hypertensive lower esophageal sphincter (LES) that fails to relax appropriately in response to swallowing [3, 4, 11]. Treatment is considered palliative because it is directed toward the elimination of the outflow resistance caused by the hypertensive LES. However, sometimes a normal or even low LES pressure has been documented by esophageal manometry in untreated patients with achalasia [10]. This finding can be a source of diagnostic confusion because the picture is similar to that of a connective tissue disorder. In addition, it creates a therapeutic dilemma because it is not known if the results of a Heller myotomy in patients with a hypotensive LES are as good as those obtained in patients with a hypertensive LES.
The goals of this study were to determine the incidence of a normal or hypotensive LES in untreated patients with achalasia and to determine the outcome of laparoscopic Heller myotomy in patients whose LES pressure is either normal or low.
Patients and methods
Between June 1990 and June 2002, a diagnosis of esophageal achalasia was made in 239 patients. There were 131 men and 108 women, whose mean age was 49 years. A total of 130 patients (54%) had previously been treated with pneumatic dilatation (105 patients, 81%), intrasphincteric injection of botulinum toxin (nine patients, 7%), or both (16 patients, 12%). A total of 109 patients had never been treated before, and they are the focus of this study. There were 63 men and 46 women, whose mean age was 48 years (range, 14–86). They had been symptomatic for an average of 51 months. Their preoperative workup included an esophagogram, upper endoscopy, and esophageal manometry.
Symptomatic evaluation
The severity of dysphagia and regurgitation was scored by the patients using a 5-point scale ranging from 0 (no symptoms) to 4 (disabling symptoms). The ability to swallow was graded as follows: excellent (no dysphagia), good (occasional dysphagia, less than two times week); fair (frequent dysphagia, two times/week or more, requiring dietary adjustments), and poor (severe dysphagia preventing ingestion of solid food). Patients were questioned before and after the operation by a fellow (not involved with the operation), who explained to them the questionnaire. All patients complained of dysphagia and 72% complained of regurgitation.
Barium esophagogram
The barium esophagogram showed a characteristic bird beak appearance of the esophagus in 96 patients (88%). The esophageal diameter was less than 4 cm in 53% of patients, between 4 and 6 cm in 22% of patients, and more than 6 cm in 25% of patients.
Upper endoscopy
Endoscopy was performed to rule out the presence of a peptic or neoplastic stricture of the distal esophagus.
Esophageal manometry
The patients were studied after an overnight fast using a technique previously described [8]. Medications that might interfere with esophageal motor function (i.e., metoclopramide, nitrates, and calcium channel-blocking agents) were discontinued at least 48 h before the study. The following variables were assessed: resting pressure of the LES and esophageal peristalsis:
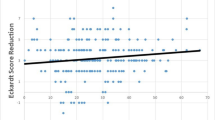
Based on the LES pressure (normal, 14–24 mmHg), the patients were divided into three groups (Table 1 and Fig. 1):
-
Group A: LES pressure <14 mmHg, 31 patients (28%)
-
Group B: LES pressure 14–24 mmHg, 29 patients (21%)
-
Group C: LES pressure >14 mmHg, 49 patients (45%)
LES relaxation in response to a fluid bolus of 5 ml of water was absent in 30% of patients, partial in 60%, and normal in 10%. Primary peristalsis was absent in all patients.
Ambulatory 24-h pH monitoring
Acid-suppressing medications were discontinued 3 (H2 blocking agents) to 14 days (proton pump inhibitors) before the study. During the study, the patients consumed an unrestricted diet and took no medications for gastroesophageal reflux disease. Ambulatory pH monitoring was performed by placing a pH probe 5 cm above the upper border of the manometrically determined LES [8].
Operative technique
Fifty-three of the 109 patients (49%) had a laparoscopic myotomy and Dor fundoplication (group A, four patients; group B, 18 patients; group C, 31 patients) (Table 2). The myotomy was 7 cm long and extended for approximately 2.0 cm onto the gastric wall. After completion of the myotomy, the short gastric vessels were divided, and an anterior 180° anterior fundoplication (Dor fundoplication) was constructed [9].
Follow-up
No patient was lost to follow-up. All patients were examined 2 and 6 weeks after surgery, and they were subsequently seen in the office or contacted by telephone every 3 or 4 months. The mean duration of follow-up was 44 ± 29 months for group A patients, 48 ± 24 months for group B patients, and 34 ± 23 months for group C patients.
Statistical analysis
Analysis of variance, Wilcoxon’s signed-rank test, Fisher’s exact test, and the Kruskall–Wallis test were used for statistical evaluation of the data. Results are expressed as mean ± standard deviation. Differences were considered significant at p < 0.05. The rates of postoperative dysphagia and regurgitation in each group and differences in these rates between groups were calculated, along with 95% confidence intervals (CIs).
Results
Operation
All operations were completed laparoscopically. There was no difference in the mean duration of the operation among the three groups. The esophageal mucosa was perforated during the myotomy in one patient, and it was repaired laparoscopically without consequences.
Hospital course
The average length of hospital stay (LOS) was 36 ± 21 h (range, 23–144). LOS appeared to be similar among the three groups of patients. Overall, 61% of patients were discharged within 24 h and 94% within 48 h. Three patients (6%) had minor postoperative complications (e.g., aspiration pneumonia and pneumothorax) that prolonged their hospital stay. There were no deaths.
Symptomatic evaluation
Overall, 48 of 53 (91%) patients judged their swallowing status after the operation as excellent (77%) or good (13%). There was a similar improvement in the symptom score among the three groups of patients who underwent laparoscopic Heller myotomy regardless of the preoperative LES pressure (Table 2). Specifically, the estimated risk of postoperative dysphagia in patients in group B (two of 18 patients, 11% failure) was only 1% (CI, −16 to 19%) higher than that of patients in group C (three of 31 patients, 10% failure). Similarly, comparing patients in groups A and B combined versus group C produced a risk difference of −0.5% (CI, −16 to 15%). Furthermore, the risk difference of postoperative regurgitation in patients in group B versus group C was −1% (CI, −15 to 13%). Similarly, in patients in groups A and B combined versus group C, the risk difference was 2% (CI, −12 to 17%). The failure rate of the surgical treatment in relieving dysphagia for all the groups was 9% (five of 53 patients; CI, 3–21%). The failure rate in relieving regurgitation was 8% (four of 53 patients; CI, 2–18%).
Esophageal manometry
Manometry was repeated postoperatively in 18 patients (Fig. 2). LES pressure decreased from 11 ± 1 to 9 ± 3 mmHg in group A (p = NS), it decreased from 18 ±3 to 9 ± 3 mmHg in group B (p < 0.05), and it decreased from 36 ± 9 to 8.5 ± 3 mmHg in group C (p < 0.05). Patients who had excellent/good results and patients who had fair/poor results had similar LES pressures and length postoperatively. In all patients, esophageal peristalsis was absent preoperatively and did not return postoperatively.
Ambulatory pH monitoring
Ambulatory pH monitoring was performed postoperatively in 16 patients. Gastroesophageal reflux was present in two patients (12.5%)—one group B and one group C patient.
Discussion
The results of our study show that in 55% of untreated achalasia patients the LES pressure is either normal or low, and laparoscopic Heller myotomy usually relieves symptoms regardless of preoperative LES pressure.
Manometric profile in patients with esophageal achalasia
For many years, the diagnosis of esophageal achalasia rested almost exclusively on the presence of a hypertensive LES. Even widely used textbooks for medical students and surgical residents stressed the importance of this finding, which was considered essential for the diagnosis and constituted the rationale for the therapy [11]. However, other investigators have shown that in untreated patients with achalasia the LES pressure can be normal in up to 45%. of patients [10], suggesting that the key finding for the diagnosis on esophageal manometry is the complete absence of esophageal peristalsis. This means that 100% of the swallows are followed by simultaneous contractions, with each wave often representing the mirror image of the other waves throughout the entire length of the esophagus. In our swallowing center, we found that only 45% of untreated achalasia patients had a hypertensive LES: the LES pressure was instead normal (14–24 mmHg) in 27% and below normal (<14 mmHg) in 28% of patients. Therefore, based on the old diagnostic criteria, the diagnosis would have been questioned in 55% of patients.
In patients with absent esophageal peristalsis and a hypotensive LES, the differential diagnosis with a connective tissue disorder such as scleroderma must be considered. In these cases, it is important to reach a conclusion after reviewing the results of the clinical evaluation, barium swallow, endoscopy, and pH monitoring in addition to the esophageal manometry. In esophageal achalasia, dysphagia is usually the presenting symptom, whereas in patients with scleroderma heartburn is more frequent. A barium swallow shows distal esophageal narrowing in most patients with achalasia, whereas the gastroesophageal junction is wide open in patients with scleroderma (Fig. 3). The endoscopy shows a dilated esophagus with retained food in achalasia, whereas esophagitis or a stricture is often present in patients with scleroderma. The pH monitoring is usually negative in untreated achalasia patients.
Outcome of surgical therapy in achalasia patients with a normal pressure or hypotensive LES
The goal of therapy in esophageal achalasia is the elimination of the outflow resistance caused by the LES. For instance, a decrease in the absolute LES resting pressure below 10 mmHg has been traditionally considered the therapeutic goal of pneumatic dilatation [3]. However, in some patients dysphagia persists even though LES pressure has dropped below this value. In these cases, esophagectomy has been recommended as the only logical therapy, on the assumption that a Heller myotomy can do no more to relieve dysphagia [7, 10]. However, when we tested this hypothesis and treated nine symptomatic patients with a hypotensive LES after pneumatic dilatation, dysphagia resolved in eight of them (89%) and the results were similar to those obtained in patients with a hypertensive LES [2]. These results suggest that a laparoscopic Heller myotomy is indicated if dilatation does not relieve dysphagia, even if the LES pressure has been decreased to less than 10 mmHg, and that esophagectomy should be reserved for the occasional failure of this simpler operation.
Because we were confident about the diagnosis of achalasia even in those patients with a normal or low LES pressure, we decided to perform a laparoscopic Heller myotomy and Dor fundoplication. This operation has, in fact, an excellent track record and it is associated to very low morbidity and no mortality [1, 5, 6, 9]. The results show indeed that this operation improves the swallowing status in the majority of patients, regardless of the preoperative LES pressure. Excellent or good results were obtained in 90% of patients with a hypertensive LES, in 89% of patients with a normal pressure LES, and in 100% of patients with a hypotensive LES. Although we acknowledge that only four patients had a hypotensive LES and that these results need to be confirmed in a larger cohort of patients, we suggest that a Heller myotomy should be tried in every patient, regardless of the LES pressure. Interestingly, when we repeated the manometry postoperatively we found that there was a significant decrease in LES pressure in group B and C patients, but the pressure appeared to remain the same in patients who had a hypotensive LES preoperatively (Fig. 2). This finding suggests that factors other than the absolute measured pressure of the LES must play a role in the response of dysphagia to therapy. A myotomy uncovers approximately 40–50% of the circumference of the esophageal mucosa, probably eliminating any degree of sphincteric obstruction.
Conclusions
Less than half of untreated achalasia patients have a hypertensive LES. A Heller myotomy is a safe and effective operation, which should be considered the primary form of therapy irrespective of the LES pressure. Esophagectomy should be reserved for failures of this simpler operation.
References
R Ackroyd DI Watson PG Devitt GG Jamieson (2001) ArticleTitleLaparoscopic cardiomyotomy and anterior partial fundoplication for achalasia. Surg Endosc 15 683–686 Occurrence Handle10.1007/s004640080037 Occurrence Handle1:STN:280:DC%2BD3MrksV2lug%3D%3D Occurrence Handle11591968
U Diener MG Patti A Molena P Tamburini PM Fisichella K Whang LW Way (2001) ArticleTitleLaparoscopic Heller myotomy relieves dysphagia in patients with achalasia and low LES pressure following pneumatic dilatation. Surg Endosc 15 687–690 Occurrence Handle10.1007/s004640080098 Occurrence Handle1:STN:280:DC%2BD3MrksV2luw%3D%3D Occurrence Handle11591969
VF Eckardt C Aignherr G Bernhard (1992) ArticleTitlePredictors of outcome in patients with achalasia treated by pneumatic dilation. Gastroenterology 103 1732–1738 Occurrence Handle1:STN:280:ByyD1czosFU%3D Occurrence Handle1451966
I Hirano RP Tatum G Shi Q Sang RJ Joehl PJ Kahrilas (2001) ArticleTitleManometric heterogeneity in patients with idiopathic achalasia. Gastroenterology 120 789–798 Occurrence Handle1:STN:280:DC%2BD3M7mtVaktQ%3D%3D Occurrence Handle11231931
JG Hunter TL Trus GD Branum JP Waring (1997) ArticleTitleLaparoscopic Heller myotomy and fundoplication for achalasia. Ann Surg 225 655–665 Occurrence Handle10.1097/00000658-199706000-00003 Occurrence Handle1:STN:280:ByiA2svjsFM%3D Occurrence Handle9230806
BK Oelschlager L Chang CA Pellegrini (2003) ArticleTitleImproved outcome after extended myotomy for achalasia. Arch Surg 138 490–497 Occurrence Handle10.1001/archsurg.138.5.490 Occurrence Handle12742951
MB Orringer MC Stirling (1989) ArticleTitleEsophageal resection for achalasia: indications and results. Ann Thorac Surg 47 340–345 Occurrence Handle1:STN:280:BiaC1M3mtV0%3D Occurrence Handle2649031
MG Patti M Arcerito J Tong M Pinto ParticleDe M Bellis Particlede A Wang CV Feo SJ Mulvihill LW Way (1997) ArticleTitleImportance of preoperative and postoperative. pH monitoring in patients with esophageal achalasia. J Gastrointest Surg 1 505–510 Occurrence Handle10.1016/S1091-255X(97)80065-0 Occurrence Handle9834385
MG Patti PM Fisichella S Perretta C Galvani MV Gorodner T Robinson LW Way (2003) ArticleTitleImpact of minimally invasive surgery on the treatment of esophageal achalasia: a decade of change. J Am Coll Surg 196 698–705 Occurrence Handle10.1016/S1072-7515(02)01837-9 Occurrence Handle12742198
MF Vaezi JE Richter (1999) ArticleTitleDiagnosis and management of achalasia. Am J Gastroenterol 94 3406–3412 Occurrence Handle10.1016/S0002-9270(99)00698-X Occurrence Handle1:STN:280:DC%2BD3c%2Fnt1eisw%3D%3D Occurrence Handle10606295
LW Way GM Doherty (2003) Current surgical diagnosis and treatment. EditionNumber11 Lange McGraw-Hill New York
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gorodner, M.V., Galvani, C., Fisichella, P.M. et al. Preoperative lower esophageal sphincter pressure has little influence on the outcome of laparoscopic Heller myotomy for achalasia. Surg Endosc 18, 774–778 (2004). https://doi.org/10.1007/s00464-003-8826-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-003-8826-1