Abstract
Purpose
The goal of this study was to investigate whether locally available Nylon mosquito net might be a useful alternative to expensive commercial mesh implants for hernia repair, a clinical randomized double-blind study was performed.
Materials and Methods
Over a period of 3 months 35 patients with a total of 40 inguinal hernias were randomized for hernia repair with either a commercial graft (Ultrapro®) or a piece of sterilized 100% Nylon mesh available as mosquito net in most African village markets. The surgeons’ comfort in handling the meshes, the incidence of complications, and the patients’ quality of life before and 30 days after hernia repair were evaluated. In addition, the costs of the two materials were compared.
Results
There was no significant difference in the clinical short-term outcome of the hernia treatment or the surgeons’ comfort in handling the two different materials. The price of the locally bought Nylon mesh was 0.0043 US$ as compared to 108 US$ for the commercial mesh.
Conclusions
In situations where superior results of hernia repair depend on the use of a mesh prosthesis but where commercial material is not available or affordable, the use of Nylon mosquito net may be an alternative. Further studies with a larger number of patients and longer follow-up are justified and recommended.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The positive results of hernia repair with prosthetic meshes and the surgeon’s comfort with this method are reasons why this technique has gained importance in developed countries. Among the open techniques of inguinal hernia repair, the Lichtenstein repair is most commonly used.1 Particularly for large hernias, the mesh technique permits a tension-free repair with less pain, faster recovery, and lower recurrence rates.2 Although most hernias in African countries are voluminous and therefore ideal for the tension-free mesh repair, meshes are either not available or unaffordable for most patients in resource-poor countries.
In 1949 Nylon (Polyamide 6-6) was introduced as the first synthetic surgical thread and has been in use ever since. It is used for all kinds of sutures. In poor countries where commercial thread is not available, surgeons use sterilized Nylon fishing line bought at the local market.3–6 Nevertheless, despite extensive clinical experience with Nylon sutures, there are few publications about the use of Nylon meshes in hernia repair. Nylon implants have mostly been used for closure of laparostomies or darn.7–10
Why not use Nylon as a material for mesh hernia repair where the commercial propylene mesh is not available? Nylon as a material for mesh hernia repair could be considered an attractive alternative in regions where commercial propylene meshes are not available.
To investigate the feasibility of the use of locally available Nylon meshes, we compared a 100% Nylon mosquito net with a commercial mesh in a clinical randomized double-blind study performed at the University Hospital of Ouagadougou in Burkina Faso.
MATERIALS AND METHODS
Patients
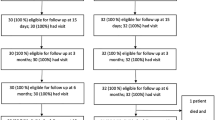
The study was approved by the Ethical Commission of the University in Ouagadougou. A detailed written consent form was signed by each patients or his/her guardian. From August 2005 to October 2005, 35 patients with 40 inguinal hernias were recruited consecutively (five patients with bilateral hernias). As soon as the surgeon had decided (mostly intraoperatively) that the hernia repair should be performed with a mesh, the patient was randomized.
Surgical Technique
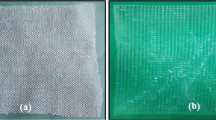
The standard Lichtenstein operation1 for hernia repair was performed under spinal anesthesia. A prophylactic single shot of intravenous 2 g ampicillin was given before incision. The mesh was trimmed and tailored in the typical way to the necessary size and shape and fixed with Nylon sutures underneath the external fascia (inlay technique; see Fig 1). All operations were performed by the same team of two certified general surgeons.
Materials
Ultrapro Mesh
The 10 × 15 cm sized Ultrapro (Ethicon Products, Norderstedt, Germany) is a composition of absorbable polyglactin fibers and nonabsorbable polypropylene fibers. Its weight is 28 g/m2, its thickness 0.5 mm, and the maximal diameter of pores is 3.5 mm.
Nylon Mesh
The Nylon mesh was bought as knitted mosquito net at the local market, trimmed to a standard size of 10 × 15 cm, cleaned with alcohol and water, packed into cotton gauze, and sterilized in the autoclave of the hospital. The manufacturer of the mosquito net confirmed that it was made of 100% Nylon (Polyamide 6/6). The mosquito net was not impregnated with pyrethrum or other insecticides. Its weight is 27 g/m2, its thickness 0.22 mm, and the maximal diameter of pores is 2.5 mm.
Observations
The primary end point was the difference between the preoperative and postoperative quality of life index (operative outcome). Outcome of the operation for the Ultrapro and for the Nylon group were compared. The Standard Multidimensional Questionnaire (SF 36)11 was modified and translated for African settings after hernia repair (Table 1). This adapted quality of life index was named “Ouagadougou Life Quality Index” (OLQUI). It ranges from 0 (worst) to 100 (best) and is achieved by adding the score points and multiplying them by the factor 2.5. This index describes not the general quality of life in Africa but predominantly the specific comfort and discomfort in the groin before and after hernia repair on the operated side under African settings. Thus in cases of bilateral hernia each side was randomized and considered a separate case and evaluated with its proper index. All patients and the observer (a certified general surgeon) were blinded. The same observer evaluated all the patients before and 30 days after the operation.
Three secondary criteria were also evaluated:
-
Both surgeons judged after each operation whether the handling of the mesh was “very practical,” “practical,” or “not practical.”
-
The local prices of the two meshes were compared.
-
Because of the great concern about infections, the rate of infections was evaluated as a separate criterion in both groups. It was registered whether there was local inflammatory reaction without fever (grade I), infection with general signs (grade II), or severe infection that required reoperation (grade III).
The baseline characteristics included age, general condition of the patients, and some characteristics of the hernia (Table 2). Concerning the primary end point, a difference of less than 15 score points on average between the two groups was regarded as not clinically relevant.
Statistical Analysis
The χ2-test was used to compare observed proportions of categorial data in the two groups. If the conditions of the χ2-test were not fulfilled, Fisher’s exact test was used alternatively. The operative outcome (i.e., the difference between the preoperative and postoperative life quality index) in each group was assessed by the paired t-test. The patient’s age and the preoperative and postoperative Ouagadougou Life Quality Indexes in the two groups were compared with the two-sample t-test. Normal distribution was checked by the Kolmogorov-Smirnov goodness-of-fit test. All statistical calculations were done with SAS software, release 8.02. The sample size (40 cases; 20 in each group) was calculated on the basis of a two-sample t-test for the operative outcomes assuming a mean difference of 15, with a power of 0.90 and allowing a type I error of 0.05. A result was considered statistically significant for P < 0.05.
RESULTS
As shown in Table 1, the baseline characteristics were comparable. Furthermore, the Ouagadougou Life Quality Indexes before operation were similar in the two groups (Table 3). There were two dropouts in each group because patients did not appear for control examination (n = 3) or violation of protocol (n = 1). No severe complications were observed. There was not even a single grade I infection, and no reoperations were needed in either group.
The postoperative OLQUI improved from 72.6 to 86.8 on average in the Nylon group and from 72.5 to 88.5 in the Ultrapro group (Table 3). This represents an improvement after operation of about 20% in the Nylon group versus 22% in the Ultrapro group. These two differences within each group are statistically significant (P = 0.0091 and P = 0.0001, respectively; paired t-test; Table 3) indicating a real improvement after operation. However, the differences between the mean outcomes of the two groups are neither statistically significant (P = 0.7566; two-sample t-test; 95%-CI: [–13.55; 9.94]; Table 3) nor clinically relevant.
The surgeons judged the ease of use as “very practical” in both groups. No difficulties in handling were observed.
The price of a 10 × 15-cm Ultrapro mesh purchased in Europe and shipped to Burkina Faso is 108 US$. Meshes for hernia repair are only available in Burkina Faso through special orders for about 200% of the price paid in the USA. A Nylon mosquito net measuring 15 m2 (not impregnated with insecticides) costs 4.30 US$ at the local market in Ouagadougou. The price of a piece of 10 × 15 cm2 mosquito mesh would amount to 0.0043 US$, which is a negligible amount even in Burkina Faso. The effort of cutting and stocking the homemade mesh does not exceed the effort of buying the commercial graft. Even the sterilization can be performed together with the other surgical instruments used for the operation, so that no extra costs accrue.
For a hernia repair without mesh at the Yalgado University Hospital of Ouagadougou, a patient pays 40 US$, which equals two average monthly salaries.
DISCUSSION
This study suggests that the hernia repair with locally available Nylon mesh is feasible with the same good short-term results obtained with commercial mesh.
In Burkina Faso the use of a commercial mesh increases the price for hernia repair by approx. 250% from 40 US$ to 140 US$. Most patients can not afford the operation if a commercial graft is used.
Much like the locally available Nylon thread (fishing line) used as surgical suture material by surgeons in Africa for many years, the mosquito mesh could be a cost effective alternative in countries where commercial meshes are not available or affordable.
The evidence that Nylon is an acceptable material for intracorporeal implant has been shown by many studies, also with long-term results. It is widely used as suture material for hernia repair.7–9 As a mesh, it was used for closure of laparostomies.10 The reason it has not been used for mesh hernia repair could be that at the origin of the mesh technique polypropylene was the favorite material for nonabsorbable suture material. Polypropylene is still the preferred material for meshes for hernia repair because it induces less chronic inflammatory response than Nylon. However, in contrast to Nylon, polypropylene causes extensive fibrosis. The resulting stiffness of the abdominal wall and the foreign body sensation have recently been under debate.12 Therefore, meshes that induce less fibrosis are now more frequently used.
Although we have good long-term results with Nylon as a material for intracorporeal implant, results are not yet available for its use as a mesh for hernia repair. However, the same applies to other commercial meshes.12 Beside the material, one difference remaining is that commercial suppliers guarantee a certain quality of their brand. The surgeon might feel more comfortable using this material. But is this really necessary? Quality assurance (QA) is important, as it offers valid and sustainable confirmation of manufacturing purity for a given product. International QA standards for health devices are high, but they are unlikely to justify or account for the extreme difference in price between two products with a similar performance.
The outcome of this trial suggests that for these homemade Nylon meshes, which were sterilized prior to use, the quality was adequate. Local production of cost-saving materials such as those described in this article will require compliance with appropriate QA standards, but would offer an affordable product nonetheless. The surgeon must take responsibility for the quality and sterility of the material. But this is nothing exceptional, because surgeons do the same for all the other materials used and the sterilized instruments, as well as for their own work.
Local production by surgical units warrants exploration. Nevertheless surgeons using the local Nylon mesh should try to collect long-term results, even though this may not always be easy in Africa, where patients disappear to their villages once they are cured. One danger could remain: in areas with high endemic load of malaria. If the implants are cut from actively used mosquito nets anopheles could get a window of opportunity, resulting in a higher risk of malaria.
References
Lichtenstein IL, Shulman AG, Amid PK, et al. The tension free hernioplasty. Am J Surg 1989;157:188–193
Scott NW, McCormack K, Graham P, et al. Open mesh versus non-mesh repair of inguinal hernia. Cochrane Database Syst Rev 2002:CD 002197
Longombe AO, Ralaimiarison A, Lusi KM. The use of fishing Nylon for surgery in rural areas in north east Zaire. Trop Doct 1993;23:179–180
Bewes P. Abdominal closure. Trop Doct 2000;30:39–41
Hodges AM. Fishing line: a valuable suture material. Trop Doct 2001;31:98–99
Freudenberg S, Nyonde M, Mkony C, et al. Fishing line suture is a cost saving alternative for atraumatic intracutaneous skin closure–a randomised clinical trial in Rwanda. World J Surg 2004;28:421–424
Saha SK. Hernioplasty: a new approach against the recurrence. Hernia 2005;9:134–139
El-Bakry. Application of darn for the repair of inguinal hernia. A University hospital experience. Saudi Med J 2002;23:1347–1349
Koukourou A, Lyon W, Rice J, et al. Prospective randomized trial of polypropylene mesh compared with Nylon darn in inguinal hernia repair. Br J Surg 2001;88:931–934
Shah SR, Abhayankar AB, Mathur SK. Meshlaparostomy—a comparison between polypropylene mesh and indigenous Nylon net.Trop Gastroenterol 1996;17:49–54
Ware JE Jr, Sherebourne CD. The MOS 36-36 item short-form health-survey (SF 36). 1. Conceptual framework and item selection. Med Care 1992;30:473–483
Post S, Weiss B, Willer M, et al. Randomized clinical trial of lightweight composite mesh for Lichtenstein inguinal hernia repair. Br J Surg 2004;91:44–48
Acknowledgments
The authors are grateful to the German Academic Exchange Service (DAAD) for sponsorship and financial support of the academic exchange program between Burkina Faso and Siegen. Many thanks go to the entire staff of the surgical department in Ouagadougou, where the study was performed. We also gratefully acknowledge the editorial input of Reinhart Freudenberg.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Freudenberg, S., Sano, D., Ouangré, E. et al. Commercial Mesh versus Nylon Mosquito Net for Hernia Repair. A Randomized Double-blind Study in Burkina Faso. World J. Surg. 30, 1784–1789 (2006). https://doi.org/10.1007/s00268-006-0108-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-006-0108-3