Abstract
Background
Adverse economic conditions often prevent the widespread implementation of modern surgical techniques in third world countries such as in Sub-Sahara Africa.
Aim of the study
To demonstrate that a modern technique (laparoscopic totally extraperitoneal inguinal hernioplasty [TEP]) can safely be performed at significantly lower cost using inexpensive mesh material.
Settings
Douala University Hospital Gynecology, Obstetrics and Pediatrics and two affiliated centers, Ayos Regional Hospital and Edéa Regional Hospital in Cameroon.
Patients and methods
Prospective randomized controlled trial (RCT) of consecutive adult patients presenting with primary inguinal hernia treated by TEP, comparing implantation of sterilized mosquito mesh (MM) with conventional polypropylene mesh (CM). Primary endpoints were peroperative, early and midterm postoperative complications and hernia recurrence at 30 months.
Results
Sixty-two patients (48 males) were randomized to MM (n = 32) or CM (n = 30). Groups were similar in age distribution and occupational features. Peroperative and early outcomes differed in terms of conversion rate (2/32 MM) due to external (electrical power supply) factors and mesh removal for early obstruction (1/30 CM). No outcome differences, including no recurrences, were noted after a median follow-up of 21 months.
Conclusion
In this RCT with medium-term follow-up, TEP performed with MM appears not inferior to CM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Despite reported superior outcomes of tension-free mesh hernioplasty such as Lichtenstein’s repair, many surgeons operating in economically unfavored areas still routinely perform primary closure herniorrhaphy to avoid the cost of mesh material. However, thanks to the pioneer work of Reddy [1] towards the end of the previous century, the cost issue of mesh use has been largely mitigated by the introduction of custom-made mosquito mesh, which allowed for the rapid spread of mesh inguinal hernioplasty in poor countries such as in sub-Saharan Africa. Recently, Löfgren et al. provided level A evidence that MM could indeed safely be used in Lichtenstein’s inguinal hernia repair, at least in men and with a follow-up of 1 year [2]. On the other hand, despite mounting evidence [3] on the benefits of the laparoscopic technique for inguinal hernia repair, reports on the use of this inexpensive material for laparoscopic hernia repair are scarce. The hardware needed for laparoscopic surgery (i.e. the endoscope, laparoscopic tower and insufflator) is by now widely distributed all over the world, including in developing countries, and laparoscopic techniques are currently in widespread use. The cost-determining factor and therefore the main limiting hurdle for wide distribution remains the disposable material, such as staplers and implants. Our recent study indicated that TEP with MM was feasible, cost-effective, with good outcomes in an economically underprivileged hospital setting [4].The purpose of the current study was to provide high level evidence that the use of inexpensive prosthetic material (MM) actually allowed to extend the field of indications of allegedly expensive procedures such as laparoscopic TEP procedure to poor areas of the world.
Patients and methods
Study design
After the Institutional Review Boards (IRB) approval was obtained from the Ministry of Health ref 2018/0042/HGOPED/DG/CEI, this prospective randomized study was carried out as per submitted protocol from the University Hospital of Douala. (Appendix). Reference of study registration: ISRCTN24826334.
The main endpoint of the study was the assessment of the clinical efficacy for laparoscopic inguinal hernia treatment performed with sterilized MM in comparison to the use of traditional mesh material (non-inferiority study) in terms of peroperative, early and midterm postoperative complications and clinical recurrence rate (primary endpoint). The secondary endpoint was the demonstration of the cost-saving potential of this novel approach weighed against a conventional approach.
Patients and study setting
All consecutive adult (> 16 years) native patients presenting at one of our hospitals between October 2018 and March 2020 and suffering from reducible primary or recurrent inguinal hernia, either uni- or bilateral, were included.
Exclusion criteria were: history of laparotomy or retroperitoneal surgery, as well as strangulated (irreducible) inguinal hernias, inguinoscrotal hernias and non-inguinal hernias. Patients who refused to consent to the study, or were deemed unfit to undergo general anesthesia as per anesthesiologist’s assessment were excluded.
All patients were examined preoperatively by at least one of the authors and checked as per routine by a senior anesthesiologist. After informed consent had been obtained, both for surgery and for inclusion in the study, the patients were scheduled for surgery, described in the consent form as laparoscopic TEP unilateral/bilateral inguinal hernioplasty (the study protocol included systematic exploration of the contralateral side, even in the absence of clear signs of contralateral hernia). In case of bilateral hernia, the type of mesh used was identical on both sides.
The interventions were free of charge for patients and were part of a cooperation agreement between the Université Libre of Brussels and the University of Douala funded by the (ARES/Belgium) in order to train Cameroonian surgeons in minimally invasive surgery (PFS2016).
Treatment of possible complications related to the herniorrhaphy was provided, as needed, at no cost to the patients.
Material
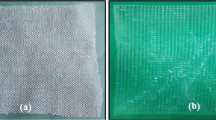
The two meshes used were sterilized MM (Nylon), and CM polypropylene Parietene macroporous® Medtronic, Puerto Rico (Table 1).
The MM nylon prosthesis was tailored by cutting out areas of mosquito netting into 15 cm × 15 cm pieces, which is similar in area to conventional prostheses. Sterilization was carried out in a type 3 autoclave at a pressure of 100 Kilo-Pascal at 121° for 20 min. The packaging was carried out in sterile packaging in semblance to those of CM.
All procedures were performed by the same team of surgeons. All patients received antibiotic prophylaxis (2 g Ceftriaxone intravenous) before skin incision.
Randomization and blinding
On the day of surgery, an even number of patients (n = 6) was programmed. In the absence of the surgeon and the patients, an equal number of prostheses were prepared by the nurse, half of them MM (code A) and the other half CM (code B). In order to anticipate the possibility of bilateral hernias, 3 × 2 prostheses of the same type were inserted in a sealed envelope, and an external doctor (not involved in the study)arbitrarily attributed a number of 1 to 6 to each envelope. Patients and surgeons were unaware of the selection and processing of the types of prostheses. Each patient drew one number between 1 and 6 before entering the operating room. The corresponding prosthesis was handed out to the surgeon in the operating room after dissection had been completed. The name of the patient and the corresponding code of the implanted prosthesis were mentioned in a special register. The type of prosthesis however was not mentioned in the operative report and remained unknown to the patient and the nursing team throughout the postoperative period and follow-up.
Procedure
The patient was placed supine, arms alongside the body, and general anesthesia with endotracheal intubation initiated as per routine. The patient was prepared and draped, the preperitoneal space entered, and the preperitoneal inguinal dissection carried out as described by others [5]. After full dissection of the retro-inguinal space by the surgeon, a sterile mesh was provided from the operating theatre supply, and the code on the drawn envelope number was recorded by the circulating nurse in the “ad hoc” registry. As previously mentioned, in case of bilateral hernias (either foreseen or unexpected), the mesh used for the contralateral side was automatically of the same material as the opposite side. In case of unilateral hernia, the superfluous mesh was discarded.
Operative time was measured as duration between first incision and placement of the last skin stitch. After conclusion of the procedure, the patient was taken to the recovery room and subsequently to the ward for overnight stay, followed by discharge from the hospital the following day. Again, no mention was made of the type of implanted material in the patient’s chart, nor verbally to the patient. Hospital stay was recorded as the duration between the start of the operation and the time of discharge.
Study outcomes and data collection
Registered information included demographics, occupation, and hernia status as recorded during the operation. Possible early complications (within 30 postoperative days) were registered in the patient’s chart, as registered the day of patient’s discharge. Patients had visit after 15 days, at 3 months and every 6 months, and relevant data were recorded by a staff member who was unaware of the material used for hernia repair, yet were informed that the patient was part of an ongoing clinical trial. At each visit, the patient was interrogated and physically examined to rule out the presence of complications, such as hematoma, infection, seroma, hernia recurrence or abnormal (neural) pain. Data were kept in the patient's chart. Conclusive assessment was performed by analysis of the patient's chart and confrontation with the labelling in the ad hoc register. Finally, after conclusion of the clinical evaluation, a final financial count was made and registered.
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics 20.0 software. Data, when normally distributed, are presented as mean ± SD (range) or, in case of non-normal distribution, as median (interquartile range—IQR). For qualitative variables, a χ2 test was used. When comparing means of quantitative variables, a Student’s t test was used. A p value lower than 0.050 was considered statistically significant.
Results
Between October 2018 and March 2020, 62 consecutive patients (48 males), median age 48, 52 years (IQR 18-77) (Table 2), with a clinical diagnosis of unilateral inguinal hernia or bilateral inguinal hernia and who did not meet the exclusion criteria, underwent TEP treatment with implantation of either MM or (CM). After randomization, 32 patients, with 8 bilateral and 24 unilateral hernias, as peroperatively diagnosed, received a MM (total 40 MM implants) (group 1). Thirty patients, with 5 bilateral and 25 unilateral hernias as peroperatively diagnosed, were treated by CM (total 35 CM implants) (group 2) (Table 3).
Mean operative time in group 1 (MM) was 66.95 ± 22.52 (45–120) min for unilateral hernia repair, and 86.62 ± 24.43 (50–120) min for bilateral hernia. Operative time in group 2 (conventional mesh) was 64.32 ± 18.77 (42–125) min for unilateral hernia, and 73.40 ± 11.95 (60–90) min for bilateral hernia (p = 0.450 for unilateral and p = 0.100 for bilateral hernia, NS).
All patients in group 1 (MM) and group 2 (CM) left the hospital on the first postoperative day. One patient in group 2 was readmitted to the hospital on the 8th postoperative day because he developed an obstruction on a peritoneal rent that had been noticed but left untreated during the hernia operation. This patient required a laparotomy and mesh removal and conversion to open herniorrhaphy procedure.
Median follow-up was 21 months (IQR 12–30 months) short-term outcomes were similar in both groups, with no recurrence noted (n = 29) in group 1 (1 patient joined only by phone), and (n = 30) in group 2 (1 patient joined only by phone; 1 patient in group 2 died from brain stroke) more than 6 months postoperatively. None of the patients who presented for postoperative evaluation spontaneously complained of any significant pain. The physical examination at the last visit was unremarkable in all participants examined.
Group 1’s financial balance sheet was statistically significantly less expensive than that of group 2, both for unilateral and bilateral repair, at 192650F (293€) and 193300F (294€), respectively, in group 1, versus 236000F (360€) and 280000F (427€), respectively, in group 2, (intergroup difference p < 0.05 for unilateral and bilateral hernia).
Discussion
Less privileged countries worldwide are facing medical conditions that require-specific care. Financial limitations constitute a sizeable hurdle for adequate treatment. Cameroon is a low- and middle-income country of central Africa with 25 million inhabitants. It was ranked 153rd /189 according to the index of human development by the United Nations in 2019.
Nevertheless, potentially threatening conditions such as inguinal hernias are at least as frequent as in developed countries, and demand adequate treatment just as imperatively as elsewhere. The complications of untreated inguinal hernias are well known, especially in individuals with a long history of clinically present hernia [6]. There is mounting evidence that mesh placement is an important component of effective hernia repair in adults [7]. Mesh placement allows for tension-free repair, a low number of recurrences, results in less pain, and faster return to work, which is even more important in less-economically privileged populations than in richer communities, who usually benefit from better social coverage [4, 6]. Mesh placement can be performed either by open approach or by laparoscopic technique. In the literature, the laparoscopic approach has proven its efficacy and likely superiority compared to the open mesh technique [8].
The laparoscopic approach and its inherent costs have not yet been specifically studied in economically less privileged areas. However, the cost issue is of particular interest in Cameroon, since this country has a health system with a high proportion of out-of-pocket payers (72%), which constitutes a heavy financial burden to most households [9].
Over the recent years, many large centers in Africa have been equipped with up-to-date laparoscopic hardware, to the benefit of many surgical, urological and gynecological departments. As could be expected, laparoscopic inguinal hernia repair has become mainstream in many centers in Africa, and the essential question is now how to avoid for poorer regions and nations within Africa such as Cameroon to lag behind more favored countries in the continent. The key to cost reduction may reside in the use of MM.
In the literature, there have been several favorable reports on the use of MM in hernia repair. An important and critical issue appears to be the type of MM and sterilization. Sterilization may potentially alter both net surface and pore size, and sterilization > 121 °C may turn the mesh into poorly useable material, especially with certain types of mosquito nets [10]. Fortunately, steam sterilization, as used in our department does not appear to affect mesh tensile strength or tear force [11]. Along the same lines, there is no evidence that MM should be more at risk of becoming infected than commercially available meshes. On the contrary, one type of commercial mesh appears to provide substantial bacterial adherence, hence susceptibility for infection [12]. In fact, data from the literature shows that when comparing three commercially available plastic meshes and a gas-sterilized polyethylene terephthalate (polyester) MM, no significant difference was noted in terms of biocompatibility between the marketed mesh types studied and the MM [13]. One can therefore conclude that appropriately sterilized MM should be no less reliable than CM. This statement was recently confirmed in a meta-analysis [14]. Similarly, another meta-analysis showed no significant difference between commercial mesh and MM in terms of adverse events [15].
In our department, laparoscopic TEP was introduced early in the second decade of this century [16]. Hence, by October 2018, when the current study was performed, the learning curve had been completed for some time and TEP had become part of the training package for surgical residents, in accordance with the French surgical training program [17].
In terms of feasibility, the operating time was in line with literature data [18], including a meta-analysis [19]. In real world circumstances however, operating time remains dependent on several factors. We observed that some patients had overly fibrous tissue in the pre-peritoneal space, despite the absence of previous surgery in that area. This finding is possibly related to genetic factors or, perhaps, to the heavy-duty occupations of most of our patients. In patients with significant fibrosis, inserting the prosthesis mesh was obviously less straightforward, which resulted in longer operating time for certain individuals. Most importantly, and regrettably, repeated power outages, often belatedly taken over by back-up generators, and causing malfunction of respirators and of the laparoscopic tower hardware necessitated conversion to open approach on 2 occasions (MM group).
In terms of early postoperative outcomes, there was no difference between groups in terms of seroma/hematoma. Actually, only one patient (in the CM group) required reoperation, but this complication was unrelated to the type of mesh used (obstruction caused by a peroperatively unnoticed rent in the peritoneum in contact with the mesh).
All patients were evaluated within about 10 days after surgery, and the number of seroma/hematoma—similar across the 2 groups—approached 10%, a figure that is in accordance with literature findings. In a recent meta-analysis, Gavriilidis et al. found an incidence of hematoma ranging from 2.9 to 12%, and an incidence of seroma of 4.6 to 5% [20]. We were concerned about mesh infections, but we were pleasantly surprised that there was no infection in our study. This could be explained by optimal sterilization of mesh coupled to the sterile working conditions during the procedures, as well as the use of 2 g of Ceftriaxone antibiotic prophylaxis. However, a larger sample size is needed to confirm these results (Figs. 1, 2).
When excluding 2 patients who needed conversion for external causes, the perioperative financial benefit of using a MM in laparoscopic TEP appears obvious. In the literature, the economic value and clinical non-inferiority of MM has been demonstrated in a number of publications [4, 21]. Prices of low-cost MM at 1/1000 the price of commercial mesh have been reported [22].
To our knowledge, the present study is the first randomized comparative trial of the TEP technique evaluating CM versus customly sterilized MM. It highlights the fact that with some ingeniousness, and provided some inexpensive essential steps are incorporated, "modern" surgical techniques can be implemented in third world countries, and should no longer be denied to their economically frail native population.
Conclusions
The mosquito mesh constitutes a valuable and financially advantageous alternative to the conventional mesh in tension-free techniques for treatment of inguinal hernias. We showed that mosquito mesh can safely be inserted laparoscopically, and its use does not result in poorer peroperative, short-term and medium-term outcomes than more expensive commercially available conventional prosthetic meshes. This finding may be of particular benefit in specific conditions where the laparoscopic approach clearly outscores the open approach, such as recurrent hernias previously treated by anterior (open) approach. These results are encouraging but a large sample and longer follow-up are necessary to confirm the current findings.
References
Tongaonkar RR, Reddy BV, Mehta VK, Singh NS, Shivade S (2003) Preliminary multicentric trial of cheap indigenous mosquito-net cloth for tension-free hernia repair. Ind J Surg 65(1):89–95
Löfgren J, Nordin P, Ibingira C, Matovu A, Galiwango M, Wladis A (2016) A randomized trial of low-cost mesh in groin hernia repair. N Engl J Med 374:146–153
Bittner R, Arregui M, Bisgaard T et al (2011) Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal Hernia [International Endohernia Society (IEHS)]. Surg Endosc 25(9):2773–2843
Essola et al (2021) The socio-economic aspects of laparoscopic approach in the treatment of inguinal hernia by mesh in Cameroon. J Surg Res 4(1):158–166
Agrawal M, Bhagwat S, Rao P (2020) Dulucq’s technique for laparoscopic totally extraperitoneal hernioplasty. J Minim Access Surg 16(1):94–96
Leubner KD, Chop WM Jr, Ewigman B, Loven B, Park MK (2007) Clinical inquiries. What is the risk of bowel strangulation in an adult with an untreated inguinal hernia. J Fam Pract 56(12):1039–1041
Naveen N, Srinath R (2014) A comparative study between modified bassini’s repair and lichtenstein mesh repair (LMR) of inguinal hernias in rural population. J Clin Diagn Res 8(2):88–91
Bullen NL, Massey LH, Antoniou SA, Smart NJ, Fortelny RH (2019) Open versus laparoscopic mesh repair of primary unilateral uncomplicated inguinal hernia: a systematic review with meta-analysis and trial sequential analysis. Hernia 23(3):461–472
http://iloglobalprogramme.Social-protection.org. Accessed 26 July 2020
Löfgren J, Beard J, Ashley T (2018) Groin hernia surgery in low-resource settings—a problem still unsolved. N Engl J Med 378(14):1357–1358
Mitura S, Koziel S (2018) The influence of different sterilization types on mosquito net mesh characteristics in groin hernia repair. Hernia 22(3):483–490
Sanders D, Kingsnorth A, Moate R, Staer J (2013) An in vitro study assessing the infection risk of low-cost polyethylene mosquito net compared with commercial hernia prosthetics. Surg Res 183(2):e31–e37
Wiessner R, Kleber T, Ekwelle N, Ludwig K, Richter D-U (2017) In-vitro examination of the biocompatibility of fibroblast cell lines on alloplastic meshes and sterilized polyester mosquito mesh. Hernia 21(3):407–416
Ahmad MH, Pathak S, Clement KD, Aly EH (2019) Meta-analysis of the use of sterilized mosquito net mesh for inguinal hernia repair in less economically developed countries. BJS Open 3(4):429–435
Patterson T, Currie P, Patterson S, Patterson P, Meek C, McMaster R (2017) A systematic review and meta-analysis of the post-operative adverse effects associated with mosquito net mesh in comparison to commercial hernia mesh for inguinal hernia repair in low income countries. Hernia 21(3):397–405
Fiennes M, Himpens J (1997) The totally extraperitoneal laparoscopy hernia repair. Surg Endosc 11:696
Barac C, Voreux JP, Occelli G, Catheline JM, Champault G (1999) Influence de la formation chirurgicale et de l’apprentissage sur les résultats du traitement laparoscopique des hernies de l’aine. Chirurgie 124:298–303
Koeckerling F (2019) TEP for elective primary unilateral inguinal hernia repair in men: what do we know? Hernia 23(3):439–459
Gavriilidis P, Davies R, Wheeler J, de Angelis N, di Saverio S (2019) Total extraperitoneal endoscopic hernioplasty (TEP) versus Lichtenstein hernioplasty: a systematic review by updated traditional and cumulative meta-analysis of randomised-controlled trials. Hernia 23(6):1093–1103
Stephenson BM, Kingsnorth AN (2011) Inguinal hernioplasty using mosquito net mesh in low income countries: an alternative and cost effective prosthesis. BMJ 343:d7448
Yang J, Papandria D, Rhee D, Perry H, Abdullah F (2011) Low-cost mesh for inguinal hernia repair in resource-limited settings. Hernia 15(5):485–489
Funding
The Project was funded by Accadémie de Recherche de l’Enseignement Supérieur (ARES) Belgium, ARES-PFS2016-Cameroon grant to J. S.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The authors: Dr Essola Basile, Professor Himpens Jacques, Dr Engbang Ndamba Jean Paul, Dr. Limgba Augustin,Dr. Djomo Tamchom Dominique, Dr. Landenne Jacques, Dr.Ngaroua Esdras, Professor Hermans P. Michel,, Mboudou Emile Telesphore, Dr. Lingier Pierre, Professor Souopgui Jacob, Professor Loi Patrizia declare no conflict of interest in relation to the content of this manuscript.
Ethical approval
The study was performed in accordance with the principles of the Declaration of Helsinki. All patients provided written informed consent. IRB approval was obtained from the ministry of health under the reference 2018/0042/HGOPED/DG/CEI. Reference of study registration: ISRCTN24826334.The study was conducted according to CONSORT guidelines and Checklist (Schulze et al., 2010).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix

Rights and permissions
About this article
Cite this article
Essola, B., Himpens, J., Ndamba, J.E. et al. Prospective, randomized clinical trial of laparoscopic totally extraperitoneal inguinal hernia repair using conventional versus custom-made (mosquito) mesh performed in Cameroon: a short-term outcomes. Surg Endosc 36, 6558–6566 (2022). https://doi.org/10.1007/s00464-022-09046-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09046-8